ORIGINAL ARTICLES
Aim. To assess the severity of heart failure (HF) 1 year after aortic valve replacement with a novel bioprosthetic valve with the “easy change” system.
Material and methods. The study included 59 patients (24 men and 35 women) diagnosed with degenerative aortic valve disease without concomitant cardiac pathology. The mean age of the patients was 69,6±4,3 years. An assessment of NYHA HF class using six-minute walk test was carried out. The venous plasma level of N-terminal pro-brain natriuretric peptide (NT-proBNP) before and after surgery was also used to determine the severity of HF. In 31 patients (52,5%), NYHA class III HF was determined before surgery.
Results. Comparative analysis of HF classes revealed a significant difference. Thus, after implantation of MedEng-BIO prosthetic aortic valve, the distance of the six-minute walk test increased by an average of 125 m (p=0,001). NT-proBNP level decreased from 162,2 pg/ml to 63,7 pg/ml (p=0,003).
Conclusion. One-year follow-up of patients after implantation of a novel bioprosthetic aortic valve showed an objective decrease in the severity of HF according to six-minute walk test and NT-proBNP level in venous blood plasma.
The Ross procedure was first proposed by Donald Ross in 1967. Numerous studies show excellent long-term outcomes of the Ross operation. One of its disadvantages is the intervention on two valves due to pulmonary homograft dysfunction.
Aim. To study long-term outcomes of pulmonary homograft use after Ross operation (cumulative incidence of pulmonary homograft dysfunction, freedom from reoperation on pulmonary homograft, long-term survival, predictors of pulmonary homograft dysfunction) using data from one Russian center.
Material and methods. A retrospective study included patients aged 18 years and older with aortic valve disease who underwent Ross procedure from April 2009 to December 2020 by a single surgeon. The age of the patients was 35 (26-44) years (men, 159 (75%)). Infective endocarditis as a cause of aortic valve pathology was diagnosed in 55 (26%) patients. Bicuspid aortic valve was diagnosed in 131 (62%) patients. The median follow-up period was 79 (26,5102,7) months.
Results. Combined interventions were performed in 40 cases (18,9%). The modified Ross procedure was used in 54 (25,5%) cases (intra-aortic — 29, using Dacron tube graft — 25). Inhospital mortality was 0,5%. The 5- and 10-year allcause survival rates were 98,5% and 95,4%, while the 10-year cumulative pulmonary valve reoperation rate and pulmonary homograft dysfunction was 4,6% and 35,2%, respectively. The only factor affecting pulmonary homograft dysfunction was patient age ≤30 years (odds ratio =0,2 with 95% confidence interval: 0,06-0,7; p=0,02).
Conclusion. Fresh pulmonary homografts have a low incidence of dysfunction and reintervention after Ross procedure. Young age is the only independent risk factor for pulmonary homograft dysfunction.
Aim. To compare the incidence of thromboembolic and hemorrhagic events after left atrial appendage occlusion (LAAO) or without prevention of thromboembolic events (TEEs) during prospective follow-up of patients with atrial fibrillation (AF) and a high risk of ischemic stroke (IS) who have contraindications to long-term anticoagulant therapy.
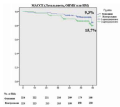
Material and methods. The study included 134 patients with AF, a high risk of IS, and contraindications to long-term anticoagulation. Patients were divided into 2 groups as follows: the first group included patients who underwent LAAO (n=74), while the second one — those who did not undergo any TEE prevention (n=60). The follow-up period was 3 years. The cumulative rate of all-cause mortality, IS, transient ischemic attacks (TIA), and systemic embolism (SE) was taken as the primary efficacy endpoint. The primary safety endpoint included major bleeding according to GARFIELD registry criteria.
Results. The rate of composite efficacy endpoint in the LAAO group was significantly lower than in the group without thromboembolic prophylaxis (5,2 vs 17,4 per 100 patient-years; adjusted odds ratio (OR), 4,08; 95% confidence interval (CI): 1,7-9,5; p=0,001). The rate of major bleeding was comparable in both groups (2,4 in the LAAO group vs 1,3 per 100 patient-years in the group without thromboembolic prophylaxis; adjusted OR, 0,55; 95% CI: 0,1-3,09; p=0,509). In addition, the event rate of net clinical benefit (all-cause mortality + ischemic stroke/TIA/SE + major bleeding) in the LAAO group was also significantly lower (5,9 vs 18,2 per 100 patient-years; adjusted OR, 3,0; 95% CI: 1,47-6,36; p=0,003).
Conclusion. Among patients with AF and contraindications to long-term anticoagulation after 3 years of follow-up, LAAO demonstrated the significant reduction of cumulative rate of all-cause mortality and non-fatal thromboembolic events. At the same time, the frequency of major bleeding was comparable between the groups, even taking into account access-site bleeding and postoperative antithrombotic therapy (ATT)-associated bleeding in the LAAO group. Further randomized clinical trials are required to confirm these data.
Aim. To analyze the long-term outcomes of a novel method of femoropopliteal bypass (FPB) surgery.
Material and methods. This retrospective, open-label, comparative study for the period from October 1, 2016 to December 25, 2019 at the Research Institute of the S. V. Ochapovsky Regional Clinical Hospital №1 (Krasnodar Krai) included 473 patient who underwent FBP. Depending on the type of graft, 5 groups were formed: group 1 (n=266) — reversed vein (great saphenous vein (GSV)); group 2 (n=59) — autologous vein graft (GSV) prepared in situ; group 3 (n=66) — autologous vein graft (GSV) prepared ex situ; group 4 (n=9) — synthetic graft (Jotec, Germany); group 5 (n=73) — upper limb veins. In all cases, Multislice computed tomography angiography revealed an extended (25 cm or more) Trans-Atlantic Inter-Society Consensus (TASC II) class D occlusion of the superficial femoral artery. The longterm follow-up period was 16,6±10,3 months. The technical result of novel FPB technique was achieved using proposed type of an autologous vein graft preparation, in which, after GSV isolation, ex situ valvulotomy was performed, followed by the non-reversed subfascial orthotopic graft passage along the neurovascular bundle by tunneling (Sheath Tunneler Set; Peripheral Vascular, USA) soft tissues. The GSV ex situ was prepared as follows: the GSV was isolated from the saphenofemoral fistula in the distal direction to the required length and removed from the wound. Further, valvulotomy was performed through the proximal end of GSV. Then the valvulotome was removed and a metal cannula was inserted. Through it, a saline solution at indoor temperature with unfractionated heparin was injected into the GSV lumen, simulating blood flow, and the quality of the performed valvulotomy was assessed.
Results. In the inhospital postoperative period, all complications developed in groups 1, 2, 3 and 5. However, no significant intergroup statistical differences were found. In the long-term follow-up, there were no significant intergroup differences in the prevalence of deaths (group 1: 4,6%; group 2: 1,7%; group 3: 4,6%; group 4: 0%; group 5: 2,8%; p=0,78), myocardial infarction (group 1: 1,9%; group 2: 0%; group 3: 1,5%; group 4: 0%; group 5: 0%; p=0,62), ischemic stroke (group 1: 0,8%; group 2: 1,7%; group 3: 1,5%; group 4: 0%; group 5: 0%; p=0,8) and shunt thrombosis (group 1: 14,5%; group 2: 19,3%; group 3: 18,5%; group 4: 44,4%; group 5: 19,7%; p=0,16). However, the highest number of limb amputations (group 1: 4,2%; group 2: 5,3%; group 3: 9,2%; group 4: 22,2%; group 5: 1,4%; p=0,03) and the highest rate of composite endpoint (sum of all complications) (group 1: 26,0%; group 2: 28,1%; group 3: 35,4%; group 4: 66,7%; group 5: 23 ,9%; p=0,05) were observed in patients with synthetic prosthesis.
Conclusion. FPB with the autologous vein graft ex situ is characterized by a comparable inhospital and long-term outcomes with BPS using the reversed autologous vein and autologous vein in situ. Thus, this surgical technique may become one of the preferable operations for patients with extended occlusion of the superficial femoral artery.
Aim. To conduct a comparative analysis of clinical and functional parameters and quality of life (QoL) in patients with chronic thromboembolic pulmonary hypertension (CTEPH), depending on the presence of a depressive disorder in long-term postoperative period.
Material and methods. The study included 182 patients with CTEPH in the long term after surgery. Depending on the Patient Health Questionnaire 9 ( PHQ-9) data, all patients were divided into 2 groups: the 1st group — patients without depressive syndrome in the long-term postoperative period, the 2nd — patients with depressive syndrome. A comparative assessment of the initial clinical and functional characteristics, as well as QoL was carried out using the SF-36 questionnaire in both groups of patients. In patients who had a coronavirus disease 2019 (COVID-19), a comparative assessment using the Post-COVID-19 Functional Status (PCFS) scale was carried out.
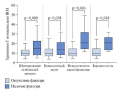
Results. Clinically relevant depressive syndrome in patients with CTEPH in the long term after surgery was registered in 25,3% of cases. In the 2nd group of patients, prior myocardial infarction (p=0,02), concomitant chronic cerebrovascular disease (p=0,01), as well as moderate and severe post-COVID-19 functional limitations according to the PCFS scale (p=0,004) were significantly more often recorded compared with the 1st group. In the 2nd group of patients, the level of QoL in almost all parameters was significantly lower in comparison with the 1st group (p<0,05). Decreased QoL (score <40) in the 2nd group concerned numerous parameters, including the physical and mental health components. In the 1st group of patients, reduced QoL was observed only in some physical parameters.
Conclusion. The group of patients with CTEPH with depressive syndrome in the long-term postoperative period was characterized by a higher incidence of concomitant chronic cerebrovascular disease and a history of myocardial infarction compared with patients without depressive disorders. In the group of patients with depressive disorders, moderate and severe post-COVID-19 functional limitations according to the PCFS scale were more often observed. Depressive disorders in patients with CTEPH in the long-term postoperative period were accompanied by significantly reduced QoL parameters. Patients experienced the greatest difficulties both during normal daily activities and in professional activities.
Aim. To evaluate changes of left ventricular (LV) diastolic function in patients with multivessel coronary artery disease before coronary artery bypass grafting (CABG) and in the early postoperative period (7-10 days), as well as to assess the relation- ship between diastolic LV dysfunction and postoperative atrial fibrillation (POAF).
Material and methods. This original prospective study of included 50 patients undergoing CABG at the Cardiac Surgery Unit № 1 of the N. V. Sklifosovsky Research Institute for Emergency Medicine from December 2020 to December 2021. All patients underwent standard echocardiography before and after surgery. Diastolic function was assessed using the following parameters: septal mitral annulus velocity (e’septal), lateral mitral annulus velocity (e’lateral), the ratio of the peak early transmitral velocity to peak early diastolic velocity of the mitral annulus movement (E/e’), left atrial volume index (ml/m2), peak tricuspid regurgitation velocity (m/s), the ratio of the peak early to late filling velocity (E/A).
Results. After CABG, 35 patients maintained sinus rhythm in the early postoperative period (group 1), while 15 patients had POAF (group 2). According to echocardiography, type 1 diastolic dysfunction prevailed in both groups; types 2 and 3 LV diastolic dysfunction were not identified. Among the parameters characterizing myocardial relaxation, in group 1 after CABG, a significant increase in the peak E (p=0,001) was noted, and due to this, the normalization of the E/A ratio was recorded (p<0,0001). An increase in e’lateral (p=0,05) was also revealed, in connection with which an increase in the E/e’ (p=0,02) was noted. In the group of patients with POAF, such changes were not detected. Left atrial volume index (ml/ m2) was significantly higher in the POAF group (p=0,02).
Conclusion. Surgical myocardial revascularization has a positive effect on LV diastolic function. Improvement in LV diastolic function after CABG may be a sign of the restoration of hibernating myocardium function, while the absence of LV diastolic function improvement, together with left atrial dilatation, may be predictors of early POAF.
Aim. To compare the results of diagnosing heart failure with preserved ejection fraction (HFpEF) in patients with hypertension (HTN) according left atrial (LA) strain values with the results obtained using the H2FPEF score and diastolic stress testing (DST).
Material and methods. The study included 293 patients with previously established HTN who were examined due to complaints of shortness of breath and/or palpitations (men, 97 (33,5%), mean age, 62,0 (55,0; 67,0) years). All patients underwent transthoracic echocardiography with the assessment of LA strain parameters and probability of HFpEF using the H2FPEF score. Eighty five patients with an intermediate probability of HFpEF underwent DST.
Results. A low probability of HFpEF according to the H2FPEF score was registered in 35 (11,9%) patients, uncertain — in 206 (70,3%), high — in 52 (17,7%). DST was negative in 43 (50,6%) and positive in 42 (49,4%) patients with an intermediate probability of HFpEF. LA strain in the reservoir phase in patients with a low probability of HFpEF averaged (median and interquartile interval) 28,0 (23,6; 31,5)%, while in patients with an intermediate probability and negative DST — 24,0 (22,0; 26,8)%, with an intermediate probability and positive DST — 20,0 (18,0; 21,0)%, and with a high probability of HFpEF — 19,6 (16,9; 21,8)%. HFpEF was diagnosed in 94 patients, including 52 with a high probability on the H2FPEF score and 42 with an intermediate probability and positive DST. The diagnosis of HFpEF was ruled out in 78 patients, including 35 with a low probability on the H2FPEF score and 43 with an intermediate probability and negative DST. Further, 172 patients with confirmed or excluded HFpEF were randomly divided into two equal cohorts. In the training cohort, HFpEF was diagnosed in 44 (51,2%) patients, in the validation cohort — in 50 (58,1%). ROC analysis performed on the training cohort for the LA strain in reservoir phase showed AUC of 0,920 (95% confidence interval (CI), 0,842-0,968) and cut-off point of 21,5%. In the training cohort, the results of HFpEF diagnosis using the indicated criterion coincided with those using H2FPEF score and DST in 86,1% (95% CI, 77,2-91,8) of cases. The Cohen’s kappa was 0,721 (95% C,I 0,575-0,868). In the validation cohort, agreement was observed in 84,9% (95% CI 75,8-91,0) of cases with Cohen’s kappa of 0,702 (95% CI 0,553-0,851).
Conclusion. In hypertensive patients, the diagnosis of HFpEF made on the basis of a decrease in the LA strain in reservoir phase to ≤21,5%, is in good agreement with the diagnosis made using the H2FPEF score and DST.
Aim. To evaluate the predictive potential of the parameters of complete blood count (CBC), lipid profile and their ratios for predicting obstructive coronary artery disease (oCAD) in patients with non-ST elevation acute coronary syndrome (NSTEACS).
Material and methods. The study included 600 patients with NSTE-ACS with a median age of 62 years who underwent invasive coronary angiography (CA). Two groups were formed, the first of which consisted of 360 (60%) patients with oCAD (stenosis ≥50%), and the second — 240 (40%) with coronary stenosis <50%. The clinical and functional status of patients before CAG was assessed by 33 parameters, including parameters of CBC, lipid profile and their ratio. For statistical processing and data analysis, the Mann-Whitney, Fisher, chi-squared tests, univariate logistic regression (LR) were used, while for the creation of predictive models, multivariate LR (MLR) was used. The quality was assessed by 4 metrics: area under the ROC curve (AUC), sensitivity (Se), specificity (Sp), and accuracy (Ac).
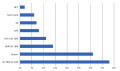
Results. CBC and lipid profile analysis made it possible to identify factors that are linearly and non-linearly associated with oCAD. Univariate LR revealed their threshold values with the highest predictive potential. The quality metrics of the best prognostic model developed using MLR were as follows: AUC — 0,80, Sp — 0,79, Ac — 0,76, Se — 0,78. Its predictors were 8 following categorical parameters: age >55 years in men and >65 years in women, lymphocyte count (LYM) <19%, hematocrit >49%, immune-inflammation index >1000, high density lipoprotein cholesterol (HDL-C) to low density lipoprotein cholesterol (LDL-C) ratio <0,3, monocyte (MON)-to-HDL-C ratio >0,8, neutrophil (NEUT)-to-HDL-C ratio >5,7 and NEUT/LYM >3. The relative contribution of individual predictors to the development of end point was determined.
Conclusion. The predictive algorithm (model 9), developed on the basis of MLR, showed a better quality metrics ratio than other models. The following 3 factors had the dominant influence on the oCAD risk: HDL-C/LDL-C (38%), age of patients (31%), and MON/HDL-C (14%). The influence of other factors on the oCAD risk was less noticeable.
For the diagnosis of myocardial infarction during cardiac surgery, various thresholds for high-sensitivity troponins have been proposed. However, studies show that the actual thresholds can be much higher. The factors associated with increased troponins after coronary artery bypass grafting (CABG) and the relationship of this marker with echocardiographic data remain unexplored.
Aim. To determine the clinical value of high-sensitivity troponin T after CABG.
Material and methods. The study included 50 patients after CABG. Before and after the operation, a blood test for high-sensitivity troponin T (Cobas E411 analyzer) and echocardiography were performed to determine the left ventricular end-systolic (ESV), end-diastolic volume (EDV) and ejection fraction.
Results. Before surgery, in 21 (42%) patients, the marker was higher than the upper normal limit (UNL), by a maximum of 5,9 times. After surgery, 23 (46%) and 2 (4%) patients had more than 10-fold and 35-fold excess of UNL, respectively. When using cardiopulmonary bypass and cardioplegia in all patients, troponin T values were 10 or more times higher than ULN, which is significantly higher (p=0,003 and p=0,018, respectively) than in patients after off-pump surgery. An average positive correlation was found between the number of grafts and troponin T concentration after surgery (r=0,40; p=0,004). At the same time, the relationship with the operation duration was not significant (r=0,19; p=0,191). After the operation, there was a moderate decrease in EDV by an average of 7,4 ml (p<0,001), a decrease in ESV by 3,5 ml (p=0,007) and an increase in ejection fraction by 2,2% (p=0,020). The dynamics of these indicators does not correlate with the troponin T after surgery (|r|<0,2; p>0,05).
Conclusion. High-sensitivity troponin T may vary depending on surgery tactics, as a result of which it reflects myocardial ischemic injury directly related to surgical procedures. This elevation is not clinically significant. Evaluation of high-sensitivity troponin T, without taking into account other research methods, cannot be used for a differentiated approach in determining perioperative myocardial infarction and used to make clinical decisions in patients after CABG.
GUIDELINES FOR THE PRACTITIONER
Aim. To assess the effect of a pharmacological protocol for the prevention of radial artery spasm, which is based on the systemic and local use of dihydropyridine calcium channel blockers, on the long-term outcomes of autoarterial coronary artery bypass grafting.
Material and methods. According to the protocol, oral nifedipine at a dose of 5 mg/day is prescribed 3 days before surgery. Then, after the radial artery is isolated, the vessel is preserved in a solution of nifedipine (adalat) until it is used. After releasing the clamp from the aorta, a nifedipine (adalat) is infused intravenously at a dose of 0,63 mg/h. In the postoperative period, the infusion of nifedipine continues for 6 hours. In the future, patients are recommended to take dihydropyridine calcium channel blockers at a dose of 5 mg/day after discharge from the hospital.
Results. The use of the pharmacological protocol (n=225) is associated with a lower number of major cardiovascular events (mortality, myocardial infarction, stroke) compared with the control group (n=230) (9,3% and 15,7%, p=0,031) during the 5-year follow-up. This result was achieved mainly by reducing the incidence of myocardial infarction (6,2% and 12,6%, p=0,018). Also, the use of the pharmacological protocol led to a decrease in repeated revascularizations (4,4% and 16,1%, p=0,0001) compared with the control group.
Conclusion. The use of a pharmacological protocol for the prevention of radial artery spasm based on the systemic use of dihydropyridine calcium channel blockers improves the long-term outcomes of autoarterial coronary artery bypass grafting.
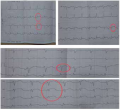
Aim. To study the effectiveness of Fortelyzin® in subgroups with different body weights in patients with ST-segment elevation acute myocardial infarction (STEMI) in the FRIDOM1 study and real clinical practice.
Material and methods. Fortelyzin® was administered in a single-bolus dose of 15 mg over 10 seconds, regardless of the body weight of patients. Metalyse® was administered in a single-bolus dose of 30-50 mg over 10 seconds, depending on body weight. The one-year results of the FRIDOM1 study were evaluated by the clinical centers using telephone contact. Monitoring of Fortelyzin® use was carried out by inpatient physicians, emergency doctors and paramedics by filling out a monitoring sheet in the period from June 2013 to December 2021 in 19243 patients with STEMI.
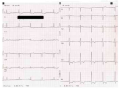
Results. In the FRIDOM1 study, the distribution of patients depending on body weight in the Fortelyzin® (n=190) and Metalyse® (n=191) drug groups was as follows: up to 60 kg — 4 people each (p=1,00); from 60 to 70 kg — 21 and 23 (p=0,87); from 70 to 80 kg — 39 and 43 (p=0,71), from 80 to 90 kg — 63 and 47 (p=0,07); from 90 to 100 kg — 30 and 41 (p=0,19); over 100 kg — 33 people (p=1,00) in each group. The effectiveness of thrombolysis according to electrocardiographic (ECG) data in the Fortelyzin® and Metalyse® groups was as follows: up to 60 kg — 75% each (p=1,00); from 60 to 70 kg — 76% vs 83% (p=0,72); from 70 to 80 kg — 82% vs 86% (p=0,76); from 80 to 90 kg — 81% vs 77% (p=0,64); from 90 to 100 kg — 80% vs 81% (p=1,00); over 100 kg — 79% vs 76% (p=1,00); in total — 80% vs 80% (p=0,87). The effectiveness of thrombolysis according to coronary angiography (CAG) (TIMI 2-3) in the Fortelyzin® and Metalyse® groups was as follows: up to 60 kg — 100% vs 50% (p=0,43); from 60 to 70 kg — 81% vs 67% (p=0,48); from 70 to 80 kg — 74% vs 84% (p=0,41); from 80 to 90 kg — 70% vs 72% (p=1,00); from 90 to 100 kg — 67% vs 66% (p=1,00); over 100 kg — 58% vs 64% (p=0,80); in total — 70% vs 71% (p=0,76). The one-year survival rate in the FRIDOM1 study in the Fortelyzin® and Metalyse® groups was 94% (p=0,91). The administration of Fortelyzin® in patients with STEMI caused blood flow restoration according to ECG data in 14624 of 19243 patients (76%), while according to CAG (TIMI 2-3) — in 3422 of 4805 patients (71%). Inhospital mortality was 5% (n=962), while intracranial hemorrhage developed in 0,5% (n=92).
Conclusion. The use of Fortelyzin® in the FRIDOM1 study and in real clinical practice in a single-bolus (10 sec) dose of 15 mg in patients with STEMI with any body weight showed its high efficacy and safety, including at the prehospital stage.
ПРЕСС-РЕЛИЗ
CLINICAL CASES
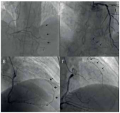
Patients with multivessel coronary artery disease require an individual approach when choosing tactics for myocardial revascularization. In some cases, additional methods for assessing the stenosis significance should be used, such as measuring the fractional or instantaneous wave-free ratio, in order to decide on the most optimal and safe management of a patient. The article presents a case report of a change in the functional significance of stenosis of the left anterior descending artery (donor artery) after endovascular treatment in the right coronary and circumflex artery systems in a patient with three-vessel coronary disease and diabetes.
This article describes the patient selection procedure for subcutaneous cardioverter-defibrillator implantation, the implantation technique, and the features of postoperative follow-up of patients, the features of programming at all stages of patient treatment.
Introduction. Allergic reactions and side effects are a common consequence of drug use and account for ~5% of all hospital admissions. The co-occurrence of ana phylactic shock and acute myocardial infarction (AMI) is called Kounis synd rome (KS).
Brief description. The article analyzes the case of ceftriaxone-induced KS in a 56-year-old female patient with a history of anaphylactic shock after ampicillin therapy. The patient was treated on an outpatient basis due to an acute upper respiratory infection. The patient was diagnosed with acute bronchitis, in connection with which antibiotic therapy with azithromycin was started. Due to inefficiency the drug was canceled and ceftriaxone 1 g in 3,5 ml of 1% lidocaine solution 2 times a day was prescribed. After the first intramuscular injection, the patient developed anaphylactic shock, which was stopped by intravenous administration of prednisolone 120 mg, dexamethasone 8 mg and adrenaline hydrochloride 1,0 ml. Almost immediately, the ST segment elevation was recorded, in connection with which thrombolytic therapy with fortelyzin 15 mg was performed. Coronary angiography revealed thrombotic occlusion of the left anterior descending artery in the upper segment. Further examination verified AMI in the patient.
Discussion. This case of AMI is pathogenetically associated with anaphylactic shock. However, the available data on the state of patient coronary system and no data on the morphologic characteristics of thrombus do not make it possibelr to define a type of KS.
Conclusion. This clinical case indicates the need for a thorough allergic anamnesis collection by physicians of any specialty and prescribing medications taking it into account.
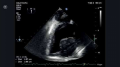
Cardiac tumors are rare, and their diagnosis is a clinical problem associated with significant heterogeneity of pathology. The purpose of this publication is to report a rare known disease and analyze the problem for the purpose of medical education. In a case report, the following characteristic signs of a heart tumor were demonstrated: rapid progression of heart failure symptoms, systemic manifestations (anemia, severe weakness). The results of transthoracic and transesophageal echocardiography made it possible to interpret the intracardiac mass as a tumor recurrence. Histological examination confirmed the diagnosis of left atrial rhabdomyosarcoma. A specific of this case is the tumor recurrence 2 years after surgery.
REVIEW
Mitral regurgitation (MR) is the second most common valvular heart disease in terms of prevalence and frequency of indications for cardiac surgery. Severe MR is characterized by a significant decrease in exercise tolerance and high mortality. The most common cause of organic MR is degenerative diseases. A detailed and systematic assessment of mitral valve and MR mechanisms is critical for the management of these patients, planning the type and timing of surgical intervention. Echocardiography plays a leading role among modern imaging methods in such patients. Examination of a patient with MR should include determining the pathogenesis of regurgitation, its severity and hemodynamic consequences. The aim of the review was to analyze the potential for using conventional and novel echocardiographic parameters to select the management strategy for patients with degenerative mitral regurgitation.
Novel biological markers, such as fibrosis marker galectin-3, peptide hormone adrenomedullin, soluble ST2, chemokine CX3CL1, surrogate marker of vasopressin, and others, are every year one step closer to being introduced into health practice. Over the past decades, significant progress has been made in the study of cardiovascular biomarkers. A key moment was the introduction of deter mining the concentration of natriuretic peptides used as markers for the diagnostic and prognostic evaluation of patients with heart failure. Currently, in order to search for novel markers for early diagnosis and risk stratification, studies have been conducted on the analysis of promising inflammatory marker tenascin-C (TNC) in cardiovascular patients. Data have been obtained that allow us to consider TNC as a tool for risk stratification and assessment of cardiovascular disease prognosis. The combination of TNC with other biological markers, in particular brain natriuretic peptide, may improve prognostic power. Nevertheless, serial testing to assess the prognosis and effectiveness of ongoing treatment, including in the conditions of a multimarker model, requires further research.
Currently, heart transplantation is the key treatment for patients with end-stage heart failure. At the same time, the immunopathogenesis of chronic allograft rejection, which is a key factor in the long-term outcome, is still poorly understood, which, in turn, explains the absence of effective non-invasive methods for its detection. This review discusses up-to-date aspects of the interaction between the microbiota and immune system factors leading to inflammation and T-cell polarization, and their participation in heart transplant rejection. Special attention is paid to the role of microvesicles in immune response modulation within heart transplant rejection.
The coronary blood flow plays an important role in protecting the myocardium from ischemia and maintaining the cardiomyocyte function in the event of occlusion of one of the epicardial arteries. It also has a potential for restoring the contractile function during subsequent myocardial revascularization, which requires its more detailed research. Most methods for assessing coronary collaterals are carried out to define the potential of their use for Retrograde chronic total occlusion recanalization. Currently, the most widely used method for assessing collateral blood flow is angiography, which, despite its relative simplicity and good knowledge, has following limitations: invasiveness, operator dependence, limited visualization, etc. At the same time, a number of other diagnostic methods can also be used to assess collateral flow. This review article is aimed at a detailed study of modern invasive and non-invasive methods for assessing the development and function of collateral vessels.
ISSN 2618-7620 (Online)