ORIGINAL ARTICLES
Aim. To reveal the association of the INS/DEL polymorphism of the angiotensinconverting enzyme (ACE) gene with acute and long-term complications of elective percutaneous coronary interventions (PCI).
Material and methods. This prospective study included 286 patients with chronic coronary artery disease who underwent elective endovascular myocardial revascularization in accordance with current guidelines. The ACE gene INS/DEL (I/D) polymorphism was determined in patients using polymerase chain reaction. Acute periprocedural complications were recorded. Acute myocardial injury (AMI) was detected in 30,4% of patients. Type 4a acute myocardial infarction developed in 3,1% of patients. A significant decrease in the glomerular filtration rate by more than 30% due to periprocedural acute kidney injury (AKI) was diagnosed in 6,5% of patients. Outcomes of elective PCIs were assessed after 4 years via telephone interviews. Cardiovascular and any-cause mortality was 3,6% and 5,1%, respectively. Acute coronary syndrome during the follow-up period developed in 15,2%, while cerebrovascular accident — in 5,4% of patients. Any-stent thrombosis was detected in 10%, and restenosis ≥30% — in 21,8% of patients. Statistical analysis was carried out using the STATISTICA 10. The odds ratio (OR) was calculated with a 95% confidence interval.
Results. Analysis of the association of ACE gene I/D polymorphism with acute and long-term complications of the PCI revealed that the presence of I allele is associated with the risk of periprocedural AKI (p=0,017; OR, 2,627 (1,161- 5,947)), as well as long-term cardiovascular events, vascular complications such as acute coronary syndrome (p=0,045; OR, 1,610 (1,007-2,573)) and stent thrombosis (p=0,01; OR, 2,073 (1,178-3,650)). The presence of genotype II further increases the risk of AKI (p=0,029; OR, 5,138 (1,022-25,824)), any acute clinical complications of PCI (p=0,041; OR, 1,996 (1,024-3,980)), and stent thrombosis (p=0,018, OR, 3,498 (1,178-10,392)).
Conclusion. In patients with chronic coronary artery disease, the carriage of allele I and genotype II of the ACE gene I/D polymorphism is associated with the risk of acute clinical complications of elective PCI, periprocedural AKI, as well as the risk of stent thrombosis and acute coronary syndrome within 4-year follow-up period after PCI.
Aim. To assess the level of microRNA (miR) -21, -22, -126, -221 in patients with coronary artery disease (CAD) with borderline coronary artery stenosis depending on comorbidities and sex.
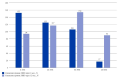
Material and methods. We examined 37 patients with class 1-3 stable CAD aged 49-59 years with borderline (40-70%) coronary artery stenosis. The relative level of miRNA was determined using real-time polymerase chain reaction. Statistical analysis was performed using the non-parametric Mann-Whitney U-test. P<0,05 were considered statistically significant. Results. The miR-221 level was higher in the group of patients with stable CAD with borderline coronary artery stenosis with a metabolically unhealthy obesity (MUO) phenotype, but without diabetes (p=0,042). The level of miR-22 and miR-126 was higher in the group of patients with stable CAD phenotype with borderline stenosis and diabetes (p=0,007 and p=0,034, respectively). The analysis of miR levels in stable CAD patients depending on sex, without taking into account the phenotype, found that miR-21 and miR-221 values were higher in men (p=0,021 and p=0,014, respectively). The study of the sex characteristics of miR content in relation to different phenotypes revealed an increase of miR22 levels in men with MUO and diabetes (p=0,048) and an increase of miR-126 levels in women with concomitant diabetes in the comparison both with patients without MUO and diabetes (p=0,018), as well as with MUO and without diabetes (p=0,007). Conclusion. The study of the miRNA level in patients with CAD with borderline coronary artery stenosis is of great interest and reflects a promising direction in diagnosis based on comorbid pathology. Keywords: miRNA, obesity phenotypes, coronary artery disease, borderline coronary artery stenosis. Relationships and Activities: none. 1Novosibirsk State Medical University, Novosibirsk; 2Federal Research Center of Fundamental and Translational Medicine, Novosibirsk; 3E.N. Meshalkin National Medical Research Center, Novosibirsk, Russia.><0,05 were considered statistically significant.
Results. The miR-221 level was higher in the group of patients with stable CAD with borderline coronary artery stenosis with a metabolically unhealthy obesity (MUO) phenotype, but without diabetes (p=0,042). The level of miR-22 and miR-126 was higher in the group of patients with stable CAD phenotype with borderline stenosis and diabetes (p=0,007 and p=0,034, respectively). The analysis of miR levels in stable CAD patients depending on sex, without taking into account the phenotype, found that miR-21 and miR-221 values were higher in men (p=0,021 and p=0,014, respectively). The study of the sex characteristics of miR content in relation to different phenotypes revealed an increase of miR22 levels in men with MUO and diabetes (p=0,048) and an increase of miR-126 levels in women with concomitant diabetes in the comparison both with patients without MUO and diabetes (p=0,018), as well as with MUO and without diabetes (p=0,007).
Conclusion. The study of the miRNA level in patients with CAD with borderline coronary artery stenosis is of great interest and reflects a promising direction in diagnosis based on comorbid pathology.
Aim. To study the contribution of rare and low-frequency variants of ANGPTL3, ANGPTL4, APOA5, APOB, APOC2, APOC3, LDLR, PCSK9, LPL genes in assessing the risk of coronary artery disease (CAD) in a cohort of Russian patients with various cardiovascular risks.
Material and methods. The study was conducted on a sample of participants in cohort and epidemiological studies (n=2405). Targeted enrichment of coding sequences and exon-intron regions of nine genes (ANGPTL3, ANGPTL4, APOA5, APOB, APOC2, APOC3, LDLR, PCSK9, LPL) was performed. Genetic diagnostics was carried out by next generation sequencing.
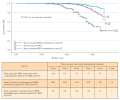
Results. CAD was confirmed in 267 patients (11%). After genetic diagnosis, all patients were divided into three following groups: individuals with previously described genetic variants associated with elevated levels of low-density lipoprotein cholesterol (LDL-C) and/or triglycerides (TGs); individuals with genetic variants associated with reduced levels of LDL-C and/or TGs; individuals without genetic variants associated with LDL-C and/or TG levels, or with two or more variants with opposite effects on LDL-C and/or TG levels. Kaplan-Meier method revealed that the groups significantly differ in cumulative risk of CAD (p<0,001 for the log-rank test), the maximum risk was in group 1, and the minimum risk in group 2. When conducting the Cox regression, we found that in persons from group 1, the hazard ratio (HR) for CAD is 2,63 times higher (HR =2,63, 95% confidence interval (CI), 1,6-4,34; p><0,001), and in persons from group 2 lower by 1,88 times (HR =0,53, 95% CI, 0,3-0,98; p=0,042) compared with persons from group 3, adjusted for other CAD risk factors: sex, age, smoking, LDL-C and hypertension. Conclusion. Genetic testing in young patients makes it possible to identify individuals with an increased genetic risk of CAD and to focus preventive and therapeutic measures primarily for this category of patients. Keywords: coronary artery disease, cardiovascular diseases, low-density lipoprotein cholesterol, genetic testing. Relationships and Activities: none. 1National Medical Research Center for Therapy and Preventive Medicine, Moscow; 2Pirogov Russian National Research Medical University, Moscow; 3E. I. Chazov National Medical Research Center of Cardiology, Moscow; 4Lomonosov Moscow State University, Moscow; 5Moscow Institute of Physics and Technology, Dolgoprudny, Russia.><0,001 for the log-rank test), the maximum risk was in group 1, and the minimum risk in group 2. When conducting the Cox regression, we found that in persons from group 1, the hazard ratio (HR) for CAD is 2,63 times higher (HR =2,63, 95% confidence interval (CI), 1,6-4,34; p<0,001), and in persons from group 2 lower by 1,88 times (HR =0,53, 95% CI, 0,3-0,98; p=0,042) compared with persons from group 3, adjusted for other CAD risk factors: sex, age, smoking, LDL-C and hypertension.
Conclusion. Genetic testing in young patients makes it possible to identify individuals with an increased genetic risk of CAD and to focus preventive and therapeutic measures primarily for this category of patients.
Aim. To assess the contribution of polymorphic variants of inflammatory response genes to the predisposition to rheumatic heart disease.
Material and methods. Using real-time polymerase chain reaction, we analyzed the prevalence of 18 polymorphic variants of 8 genes involved in the inflammatory process in 251 patients with rheumatic heart disease and 300 healthy donors.
Results. We found that homozygous TT genotypes of rs1800871 (IL10) (p=0,02) and TT rs1800872 (IL10) polymorphisms (p=0,027), as well as TT genotypes of CRP gene (rs1205) (p=0,015) and GG genotypes of rs375947 (IL12RB) (p=0,037) are "risky" and associated with the development of rheumatic heart disease.
Conclusion. Associations of polymorphic variants rs1800871 and rs1800872 of the IL10 gene, rs1205 of the CRP gene, and rs375947 of the IL12RB gene can be an important link in the pathogenesis of rheumatic heart disease and can later be used as biological markers for a personalized assessment of the disease risk.
Aim. To determine the associations of variable sites of fibrogenesis genes with the risk of left ventricular (LV) diastolic dysfunction (DD) in patients with epicardial adiposity (EA).
Material and methods. The study included 101 men with general obesity (Altai Territory) without cardiovascular diseases, diabetes and documented LVDD, of which, after determining the epicardial fat thickness (EFT), 2 groups were formed: group 1 — with EA (EA+), EFT ≥7 mm or more (n=70); group 2 — without EA (EA-), EFT <7 mm (n=31). The control group was formed from Kemerovo region residents of the corresponding sex and age and without a history of cardiovascular diseases and general obesity. Polymorphisms of the MMP9 rs17576, TGFB1 rs1800469, MMP3 rs6796620, MMP3 rs626750, MMP1 rs514921, LOC101927143 rs4290029, TIMP2 rs2277698 genes were determined in all patients using the polymerase chain reaction. After 4,7±0,3 years, all patients with general obesity underwent repeated echocardiography to assess LVDD.
Results. We found that in the group with EA for rs626750 MMP3, the carriage of the homozygous T allele is 2 times more common (recessive inheritance, p=0,0022). After 4,7±0,3 years, LVDD was registered in 18 patients in the EA+ group and in 2 patients in the EA- group. When analyzing inheritance patterns, as well as comparing genotypes in groups of patients with EA with developed LVDD (n=20) and without LVDD (n=78), we found that patients with EA and LVDD are 3,4 times more likely to be a carrier of the homozygous T allele (recessive inheritance, p=0,02) for rs1800469 TGFB1.
Conclusion. In patients with EA and LVDD, the carriage of the T rs1800469 TGFB1 allele is more common, which probably contributes to cardiac fibrosis and LVDD according to a recessive inheritance.
Aim. To study and compare genotypic and phenotypic signs in patients with non-compaction cardiomyopathy (NCM) and dilated cardiomyopathy (DCM), to conduct a comparative analysis of clinical outcomes and 5-year cumulative survival of patients with NCM and DCM.
Material and methods. The study included 144 unrelated patients with cardiomyopathy: NCM (n=74) and DCM (n=70). Mean age was 39 [30; 49] years (men, 96 (66,7%); left ventricular ejection fraction (LVEF) was 30,5 [24; 46]%. A comprehensive clinical examination included electrocardiography, Holter monitoring, echocardiography, cardiac magnetic resonance imaging, coronary angiography, DNA diagnostics (NGS+Sanger), cascade screening, and cosegregation analysis. To assess clinical outcomes, the NCM group was divided into 2 subtypes according to baseline LV systolic function (NCM/DCM phenotype — 50 individuals with LVEF ≤49%; and isolated NCM — 24 patients with LVEF ≥50%). The following adverse events were assessed as the composite endpoint: cardiovascular death, heart transplantation (HT), sustained ventricular tachycardia, ventricular fibrillation, successful cardiopulmonary resuscitation, cerebral thromboembolism. The follow-up period was 62 months.
Results. Among patients with LVEF ≤49% at a 5-year follow-up, 37 (74,0%) of 50 patients with the NCM/DCM phenotype and 41 (58,6%) of 70 patients with DCM achieved composite endpoint. Out of 24 patients with NCM with LVEF ≥50% (median LVEF, 56 [51; 61]%), 2 (8,3%) patients achieved composite endpoint (χ2=28,8; p=0,001). In the NCM/DCM group with LVEF ≤49%, a higher level of pathogenic genetic variants (64% vs 41,4%/DCM vs 29,2%/NCM; χ2=11,4; p=0,003), cerebral thromboembolism (χ2=11,8; p=0,003) and HT (χ2=10,6; p=0,005). The results of the 5-year survival analysis (Kaplan-Meier) showed a worse prognosis for NCM with LVEF ≤49% compared with DCM (log rang: χ2=11,5; p=0,001) and isolated NCM (log rang: χ2=17,02; p=0,0001). In the overall cohort (n=144), gene-positivity was also associated with worse prognosis (log rang: χ2=5,38; p=0,02).
Conclusion. In the present study, patients with dilated subtype of NCM showed a worse prognosis compared with DCM and isolated NCM. Heart failure progression and cerebral thromboembolism were the most common complications in patients with NCM/DCM.
Aim. To study the role of molecular biomarkers potentially influencing the formation and progression of heart failure (HF) with preserved ejection fraction (HFpEF) in non-obstructive coronary artery disease (CAD).
Material and methods. We examined 48 patients with newly diagnosed HFpEF against the background of non-obstructive CAD. Group 1 (n=31) included patients with class I-II HF and group 2 (n=17) included patients with class III HF; the control group consisted of patients without heart failure (n=17). The content of NT-proBNP and sST2, diastolic dysfunction and coronary flow reserve parameters were assessed.
Results. The content of NT-proBNP in patients of group 1 was 45% higher than in group 2 (p<0,001). The mean levels of sST2 did not exceed the reference values and significantly exceeded the control group (p<0,001). Coronary flow reserve (CFR) decreased (p<0,001) depending on the severity of HF. Negative associations of sST2 levels with LVEF, septal e’ and CFR were revealed, as well as NT-proBNP with CFR.
Conclusion. HFpEF in non-obstructive CAD is triggered due to progressive impairment of endothelial function, which affects the decrease in coronary and myocardial flow reserves, diastolic function, hyperproduction of humoral factors that initiate perivascular fibrosis and apoptosis of cardiomyocytes.
Aim. To study the prevalence of hyporesponse to statin therapy and its impact on the development of heart failure (HF) among patients after acute coronary syndrome (ACS) in a short-term follow-up.
Material and methods. This retrospective analysis of outpatient medical records of 400 patients observed at the Omsk Clinical Cardiology Dispensary after ACS was carried out. Optimal medication therapy was prescribed as part of the preferential provision of medicines under the 1H Program, including high-dose atorvastatin therapy (80 mg/day). Low-density lipoprotein cholesterol (LDL-C) was assessed at baseline and 1 and 12 months after therapy. Hyporesponse to statins was defined as the percentage reduction in LDL-C 14; left atrial volume index >34 ml/m2) function.
Results. There were 107 patients with hyporesponse (26,8%). Depending on the initial response to therapy, patients were divided into two groups: group 1 (hyporesponse, n=107), group 2 (more pronounced response, n=293). After 1 month, patients in the hyporesponse group had a higher level of LDL-C — 2,4 [2,2; 2,9] mmol/l (Me [25; 75%]) vs 2,0 [1,7; 2,5] mmol/l (p>0,05) in the second group. There was no difference in the prevalence of hospitalizations for recurrent ACS in the compared groups, as well as in the prevalence of new HF cases between groups.
Conclusion. The prevalence of hyporesponse to statin therapy was 26,8%, which required correction of lipid-lowering therapy in order to prevent recurrent cardiovascular events. Given the pleiotropic effects of statins that can participate in HF pathogenesis, as well as the inconsistency of current research results, further prospective long-term studies are required.
In patients with initially elevated levels of creatine phosphokinase MB (CPK-MB), its increase after percutaneous coronary intervention (PCI) may be due not only to additional injury, but also to natural release during myocardial infarction. Therefore, CPK-MB should be evaluated relative to the initial values.
Aim. To compare the CPK-MB dynamics after myocardial reperfusion relative to baseline values and the upper limit of normal (ULN) for the optimal approach to determining myocardial reperfusion injury in patients with acute coronary syndrome.
Material and methods. A single center observational study was conducted with the participation of 90 patients hospitalized with a diagnosis of acute coronary syndrome. Patients underwent a biochemical blood test for CPK-MB twice and its dynamics was determined relative to the initial value and ULN.
Results. Between the ischemia time and CPK-MB dynamics relative to the initial values, there is a moderate negative correlation. At the same time, the ratio of CPKMB after surgery to ULN is not associated with ischemia time. Analysis of covariance showed that the CPK-MB dynamics, determined relative to the initial values, is 20% dependent on the ischemia time. Individual features of coronary system anatomy, localization of the infarct-associated artery and the subsequent reperfusion procedure together explain the CPK-MB dynamics after surgery by 27%. When the ratio of CPK-MB to ULN is included in the analysis of covariance, all the above factors lose statistical significance.
Conclusion. Thus, for a more accurate assessment of myocardial reperfusion injury after PCI, not the upper limit of normal should be analyzed, but the initial values of CPK-MB. In patients with the left heart dominant, as well as in the infarction localization in the system of right or left anterior descending artery, there is a slight change in the marker. On the contrary, more pronounced dynamics is observed in patients with tortuous coronary arteries and with implantation of 2 or more stents. At the same time, the assessment of CPK-MB in relation to ULN is not associated with the ischemia time and does not depend on the clinical and angiographic characteristics and tactics of the operation.
Aim. To assess the predictive value of anthropometric indices in relation to the risk of myocardial infarction in patients with coronary artery disease (CAD) and obesity after coronary stenting.
Material and methods. The study included 229 patients with class II-IV angina pectoris, hospitalized for elective percutaneous coronary intervention with stenting. The median age was 55±7,5 years. Depending on the presence of obesity according to the World Health Organization criteria (1999), patients were divided into 2 groups. Group 1 included 107 obese patients, while group 2 — 122 non-obese patients. Patients were measured waist circumference (WC) and hip circumference (HC). In addition, waist-to-hip ratio was assessed. Lipid spectrum parameters were determined (total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C). The following indices were calculated: body mass index, visceral adiposity index, Homeostasis Model Assessment of Insulin Resistance (HOMA-IR), Metabolic Score for Insulin Resistance (METS-IR), TG-glucose index, lipid accumulation product, TG/HDL-C ratio, and metabolic index.
Results. In the group of patients with obesity, higher values of cholesterol (p<0,001), TG (p<0,001), LDL-C (p=0,006), and lower HDL-C (p<0,001) levels were established. Comparative analysis of metabolic indices showed that all indices significantly differed in both groups. In order to determine the critical values for quantitative predictors, ROC curves were constructed with the determination of threshold values that increase the likelihood of myocardial infarction after revascularization. It has been shown that only the METS-IR has prognostic significance. It was found that the METS-IR >48,16 is a predictor of myocardial infarction in patients with CAD and obesity (area under the ROC curve, 0,653, sensitivity — 75%, specificity — 64,39%; 95% confidence interval: 0,587-0,716; p=0,045).
Conclusion. In our study, we demonstrated the significance of the novel METS-IR. We found that the value of METS-IR >48,16 is a predictor of myocardial infarction in patients with CAD and obesity after coronary revascularization (area under the ROC curve, 0,653, sensitivity — 75%, specificity — 64,39%).
SUPPORTING A PRACTITIONER
According to epidemiological studies, in Russia there is a tendency towards an increase in sudden cardiac death (SCD), including among young workingage people. The leading mechanism for SCD in young patients, including those with undifferentiated connective tissue disease, is recognized as rhythm and conduction disorders. At the same time, the most tragic cases are the first and only manifestation of SCD in children and young people without structural heart disease. The article presents a brief analysis of the genetic causes of life-threatening rhythm and conduction disorders in young people, as well as a generalization of the modern possibilities of a personalized diagnostic approach from the standpoint of early cardiovascular prevention. Timely genetic diagnosis of SCD risk makes it possible to identify a predisposition to the development of a fatal event long before its occurrence, which contributes to the timely implementation of preventive measures within a high cardiovascular risk strategy and secondary prevention, maintaining working capacity, creative and social activity of young patients, and improving the quality of life.
REVIEW
In this literature review, we analyzed studies on the influence of genetic specifics of patients on the restoration of myocardial contractility after acute myocardial infarction. Data on the influence of genetic characteristics on the myocardial repair, remodeling process, and the restoration of cardiac contractility are presented. The use of genetic methods in the examination of patients and further consideration of individual characteristics when prescribing therapy will make it possible to implement a personalized approach to each patient. This will improve the effectiveness of treatment and the disease prognosis.
Recent studies in single cell RNA sequencing have improved understanding of the structure of the immune cell subpopulation in atherosclerosis. With the help of novel technologies, new subpopulations of immune cells involved in atherosclerosis have been identified. In addition, a following relatively common and strong cardiovascular risk factor has emerged: clonal hematopoiesis of indeterminate potential resulting from the accumulation of somatic mutations during life with the appearance of populations of mutant leukocyte clones. Individuals with this condition are at high risk for cardiovascular complications such as myocardial infarction and stroke, regardless of conventional risk factors. This review highlights the latest data on the study of cellular heterogeneity of immune system cells in atherosclerosis, as well as the role of clonal hematopoiesis in its development.
Cerebrovascular accident (CVA) in patients with various cardiovascular diseases is a life-threatening complication, the development of which can be contributed by both environmental and genetic factors, the understanding of which is necessary to determine the tactics of treatment and predict the disease course. The article presents a brief review of studies on genetic predictors of CVA, in particular the association of the ABCA1 rs2230806 polymorphism and the risk of CVA in cardiovascular patients. Targeted studies of associations of the ABCA1 rs2230806 polymorphism with cerebrovascular diseases in the Russian Federation, except for studies at our university, could not be found.
The article presents a literature review on the study of the relationship of FGA, FGB, F2, F5, PAI, ITGA2 gene polymorphisms with the development of pulmonary embolism (PE). We concluded that genetic factors in the development of PE are to a greater extent mutations in the F2, F5, PAI, ITGA2 genes. There is a positive correlation between the presence of combined genetic mutations and the development of PE. The study of allelic polymorphism of hemostasis genes makes it possible to predict coagulation system disorders, including PE.
CLINICAL GUIDELINES
ISSN 2618-7620 (Online)