PROGNOSIS AND DIAGNOSTICS
What is already known about the subject?
- In obese individuals, circulating levels of interleukin-6 (IL-6) are higher than in non-obese individuals.
What might this study add?
- In acute decompensated heart failure, an increase in body mass index (BMI) is accompanied by a decrease in serum IL-6 levels.
- In patients with stable heart failure, no association between IL-6 levels and BMI was found.
Aim. To estimate IL-6 levels in patients with acute decompensated heart failure (ADHF) depending on body mass index (BMI).
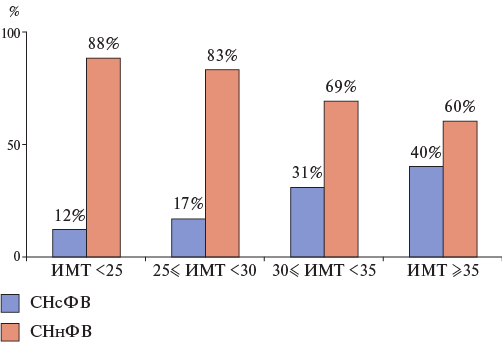
Material and methods. The study included 110 patients with ADHF. The patients were assigned into 4 groups depending on BMI. The first group included 17 patients with BMI<25 kg/m2; the second group, 29 patients with 25≤BMI<30 kg/m2; the third group, 33 patients with 30≤BMI<35 kg/m2; and the fourth group, 31 patient with BMI ≥35 kg/m2. All patients underwent standard general clinical and biochemical studies. IL-6 levels were determined using monoclonal antibodies. After 1 year of observation, clinical condition of all patients was assessed as stable.
Results. IL-6 levels in ADHF patients decreased as BMI increased. The highest IL6 values were recorded in group 1 patients (14,61(8,65; 21,14) pg/ml) and the lowest in group 4 patients (6,34(3,61; 10,17) pg/ml). As BMI increased in groups, the percentage of patients with HFpEF increased (from 12% in group 1 to 40% in group 4). Under stable condition, the intergroup differences between IL-6 were insignificant, with IL-6 levels being lower than in ADHF. A negative correlation was established between IL-6 levels and BMI (r =-0.265, p = 0.006), IL-6 levels and LVEF (r = -0,201, p= 0,040) and between BNP concentrations and BMI (r = -0,486, p < 0,001) in patients with ADHF.
Conclusion. In patients with ADHF, an increase in BMI is accompanied by a decrease in circulating IL‑6 levels, which may indicate differences in inflammatory response mechanisms in patients with normal body weight and obesity. Further research will make it possible to develop novel personalized approaches to the treatment of heart failure in overweight and obese patients.
- To assess the prognosis in elderly and senile patients with heart failure (HF), the role of hepcidin as a marker involved in the pathogenesis of both anemia and inflammation, which often accompany HF in these patients due to high comorbidity, was studied.
- The identified U-shaped relationship between hepcidin and death risk in elderly and senile patients with HF, anemia and inflammatory syndrome implies an unfavorable prognosis both at low (3,05-10,33 ng/ml) and at elevated hepcidin levels (25,81-70,71 ng/ml); therefore, hepcidin levels should be determined in addition to N-terminal pro-brain natriuretic peptide.
Aim. To study the role of hepcidin in assessing the prognosis of elderly and senile patients with heart failure (HF) and anemia.
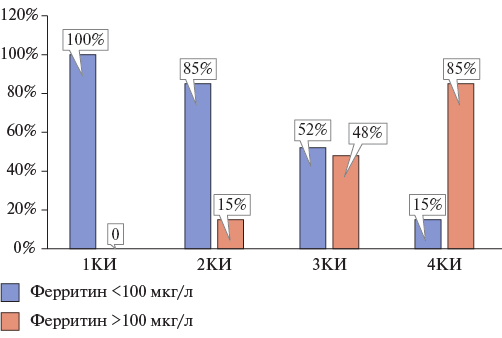
Material and methods. The study included 105 patients aged 65 to 90 years with NYHA class II‑IV HF of ischemic origin with anemia. Patients were tested for hepcidin and N‑terminal pro‑brain natriuretic peptide (NT‑proBNP) levels once upon admission. Patients were followed up until the primary endpoint of cardiovascular and non‑cardiovascular death for up to 24 months. To assess the effect of hepcidin levels on the risk of death, patients were stratified by quartiles (Q) of hepcidin levels. In each quartile, patients were divided into 2 following groups: with absolute and functional iron deficiency. Cox proportional hazards regression analysis was used to assess the effect of hepcidin levels on the death risk.
Results. In patients with HF and anemia, hepcidin levels differed significantly between Q1 and Q4 (p<0,001). Severity of absolute iron deficiency decreased from Q1 to Q4, while the severity of the systemic inflammatory response, on the contrary, increased from Q1 to Q4. During the first 6 months of follow‑up, the highest mortality was found in patients in Q1 (40%), and during 24 months — in patients in Q4 (77%). Regression analysis revealed a significant effect on the death risk of low hepcidin levels (3,0510,33 ng/ml) in patients of Q1 in model 1 (odds ratio (OR) 1,661 (95% confidence interval (CI): 1,198‑2,303), p=0,002), in model 2 (OR 1,911 (95% CI: 1,350‑2,705), p<0,001). There was also a tendency towards a significant effect of elevated hepcidin levels on the death risk (25,81‑70,71 ng/ml) in Q4 patients in model 1 (OR 1,044 (95% CI: 0,997‑1,099), p=0,070), while in model 2, no significant effects on the death risk were found (OR 1,036 (95% CI: 0,989‑1,086), p=0,135). The relationship between hepcidin and the death risk had a U‑shaped curve in both models.
Conclusion. To assess the prognosis in elderly and senile patients with HF and anemia, taking into account the identified effect of both low and elevated hepcidin levels on the death risk, hepcidin levels should be determined in addition to NT‑proBNP.
- In ischemic stroke (IS), there is a high rate of venous thromboembolism (VTE) (49%) in patients with limited mobility (RMI ≤3).
- VTE in ischemic stroke can be divided into "early" (3±1 days) and "late" (10±1 days of hospitalization).
- Identification of predictors of "early" and "late" thromboses makes it possible to determine indications for anticoagulant administration for VTE prevention in patients with IS.
Aim. To identify predictors of venous thromboembolism (VTE) in patients with ischemic stroke (IS).
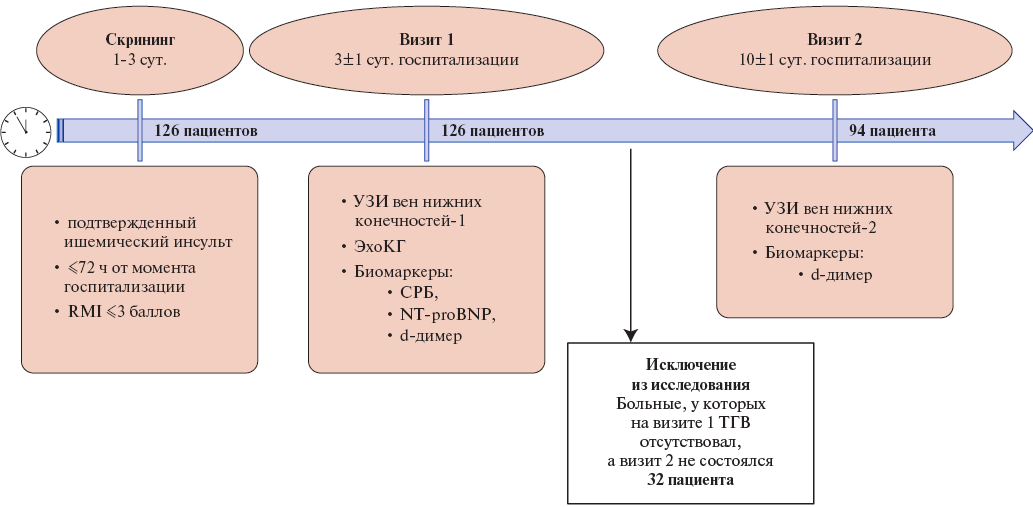
Material and methods. This single‑center prospective study had following inclusion criteria: 1) IS confirmed by neuroimaging, 2) length of hospital stay at the time of inclusion ≤72 h, 3) Rivermead Mobility Index (RMI) ≤3. A total of 126 patients were screened. The study involved 2 visits: on day 3±1 of hospitalization and day 10±1 of hospitalization. Patients without deep vein thrombosis (DVT) detected at the first visit, who did not have the second visit, were excluded from the study. The study group consisted of 94 patients. During the visits, lower limb vein and cardiac ultrasound and biomarker assessment were performed. If deep vein thrombosis was detected, CT pulmonary angiography was performed.
Results. In total, 46 cases of DVT (49%) were detected in the studied group of patients with IS, including 26 "early" thromboses (DVT at visit 1) and 20 "late" thromboses (DVT diagnosed at visit 2). Predictors of "early" thromboses are white blood cell (WBC) count upon admission >10,6 (odds ratio (OR) 3,58, 95% confidence interval (CI): 1,12‑11,39, p=0,028) and Padua score >5 (OR 5,14, 95% CI: 1,62‑16,29, p=0,005). The following are proposed as predictors of "late" thrombosis: d‑dimer level on day 3 ≥3‑fold exceeding the upper reference limit (OR 26,6, 95% CI: 3,0232,9, p=0,004) and the ratio of anterior tibial vein (ATV) flow velocity on the affected side to the opposite one ≤0,90 (OR 4,1, 95% CI: 1,1‑15,4, p=0,039).
Conclusion. In IS, there is a high rate of VTE (49%) among low‑mobility patients (RMI ≤3). Thrombosis can be divided into "early" (3±1 days) and "late" (10±1 days of hospitalization). Predictors of "early" thrombosis are Padua score >5 and WBC count on admission >10,6*109. Predictors of "late" thrombosis are 3‑fold increase in the d‑dimer upper reference level and the ratio of ATV flow velocity on the affected side to the opposite one ≤0,90 on day 3±1 of hospitalization.
- The highest predictive potential for new-onset atrial fibrillation (AF) in patients with ST-segment elevation myocardial infarction (STEMI) after percutaneous coronary intervention (PCI) has neutrophil-to-eosinophil ratio, acute heart failure Killip class, erythrocyte sedimentation rate, systemic inflammatory response index.
- Electrocardiographic and echocardiographic parameters in isolated form had lower prognostic value.
- The structure of the best prognostic model of new-onset AF in patients with STEMI after PCI, developed on the basis of multivariate logistic regression, included 9 categorical predictors.
Aim. To assessment predictive potential of electrocardiographic, echocardiographic and hematological parameters for predicting new‑onset atrial fibrillation (AF) in patients with ST‑segment elevation myocardial infarction after percutaneous coronary intervention (PCI), as well as to develop novel prognostic models based on machine learning.
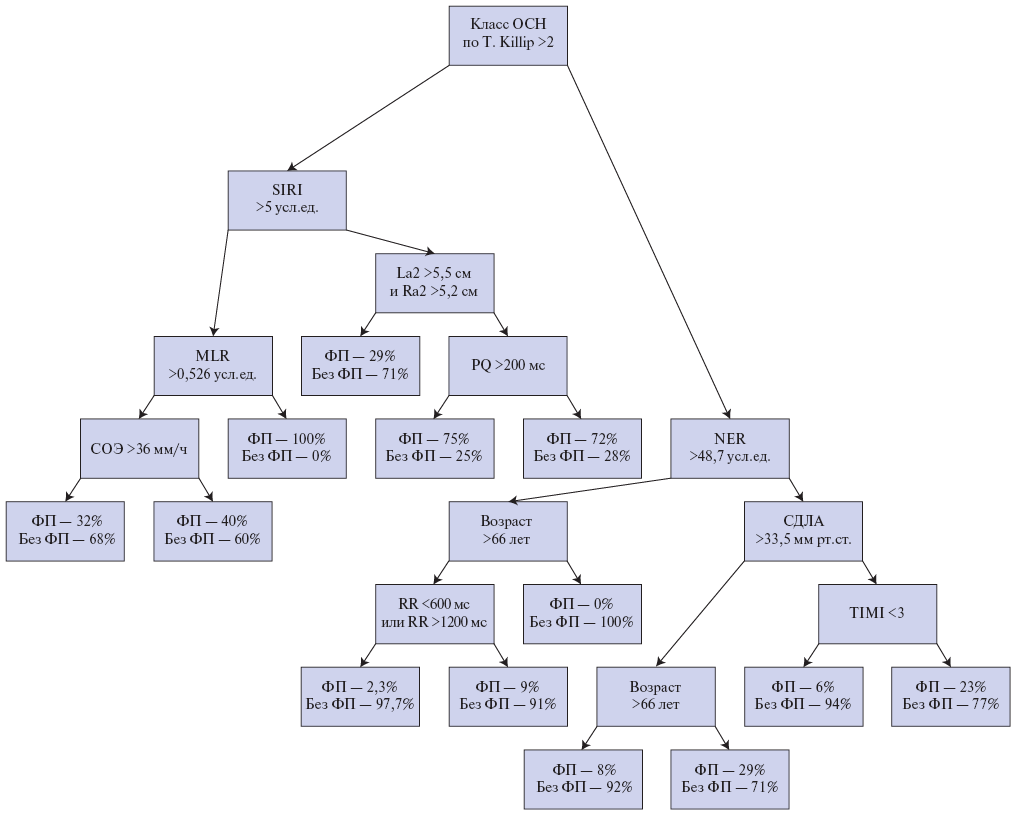
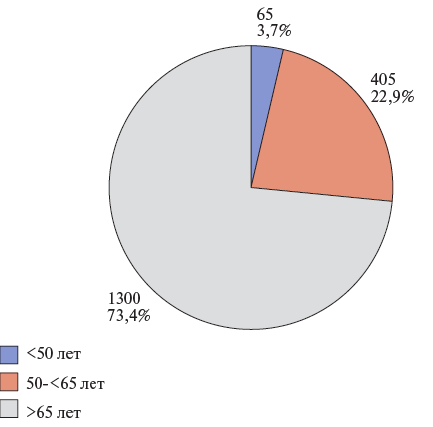
Material and methods. This single‑center prospective study included 733 patients with ST‑segment elevation myocardial infarction. Two following groups were identified: the first — 57 (7,8%) patients with new‑onset postoperative AF after PCI, and the second — 676 (92,2%) patients without cardiac arrhythmia. To predict AF, univariate and multivariate logistic regression, decision trees, CatBoost gradient boosting were used.
Results. Comparative analysis of electrocardiography, echocardiography, hematological and clinical data demonstrated that following parameters has the highest predictive potential: neutrophil‑to‑eosinophil ratio (NER) >48,7 (odds ratio (OR) 7,1), Killip class >2 acute heart failure (OR 4,44), erythrocyte sedimentation rate (ESR) >36 mm/h (OR 4) and systemic inflammatory response index (SIRI) >5 (OR 3,8). The best prognostic model of new‑onset AF after PCI (AUC=0,806) included 9 following categorical predictors: NER >48,7 conventional units, SIRI >5 conventional units, erythrocyte sedimentation rate >36 mm/h, PQ >200 ms, 600 ms< RR >1200 ms, pulmonary artery systolic pressure >33,5 mm Hg, age >66 years, TIMI <3 and Killip class >2 acute heart failure.
Conclusion. Improving the accuracy of predicting new‑onset AF after PCI can be achieved by expanding the range of potential predictors and using modern explainable artificial intelligence technologies.
- There are insufficient studies on the rationale of coronary computed tomography angiography (CCTA) in patients with acute coronary syndrome (ACS) and prior stenting and/or coronary artery bypass grafting.
- CCTA in patients with low-risk ACS and prior percutaneous coronary intervention and/or coronary artery bypass grafting allows avoiding invasive coronary angiography in 75% of patients.
- CCTA is a reliable method for assessing the condition of coronary bypass grafts.
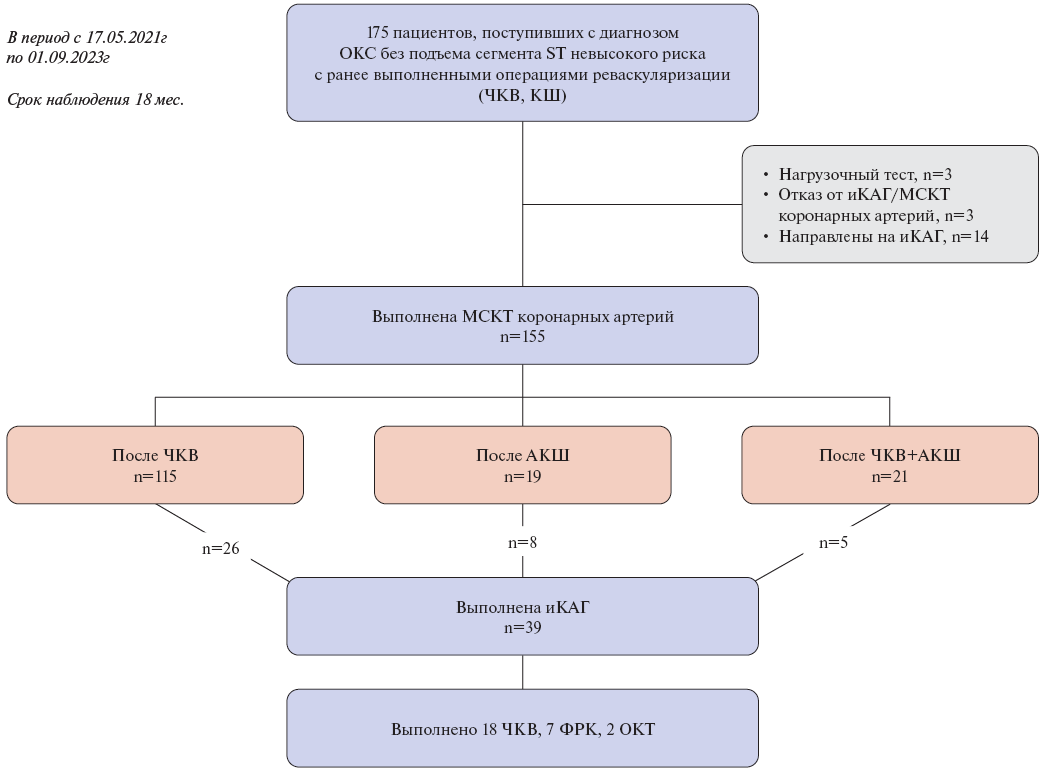
Aim. To evaluate the use of coronary computed tomography angiography (CCTA) in suspected non‑ST segment elevation (NSTE‑ACS) acute coronary syndrome in patients with prior percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
Material and methods. The study included 155 patients with prior PCI or CABG (men, 57,4%; mean age, 65,1±9,2 years) with low‑risk NSTE‑ACS who underwent CCTA.
Results. Of the 155 patients who underwent CCTA, every fourth patient, namely 39 patients (25,2%), were referred for invasive coronary angiography (ICA). Among them, 26 patients had prior PCI, 8 patients — CABG, and 5 patients — both interventions. Patients indicated for ICA had higher coronary calcium score compared to patients who did not undergo ICA as follows: Me 268,0, Q1‑Q3: 78,5‑714,0 versus Me 163,5, Q1‑Q3: 18,0‑404,0, p=0,02. The positive and negative predictive value of CCTA in diagnosing stent damage was 66,7% and 92,2%, respectively, while in diagnosing bypass graft damage — 100% and 100%, respectively.
Conclusion. CCTA in patients with low‑risk NSTE‑ACS with prior PCI and/or CABG allows avoiding ICA in 75% of patients. CCTA is a reliable method for assessing the condition of coronary bypass grafts. At the same time, assessing stent patency using CCTA is a more complex task.
- Patients with a common origin of innominate and left common carotid artery, compared to patients with normal vessel anatomy, have shortened tubular ascending aorta, lengthened aortic root and arch, as well as higher rate of type I arch and lower rate of type III arch.
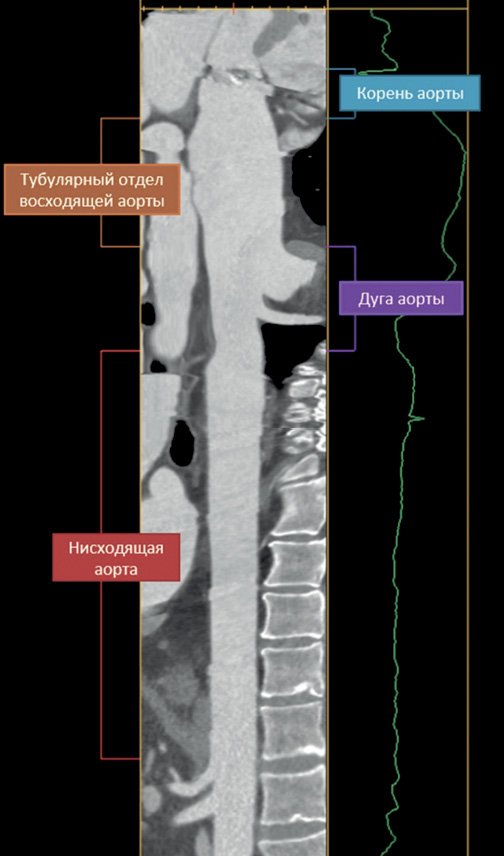
Aim. To analyze thoracic aortic geometry in patients with ascending aortic aneurysm in combination with normal or variant anatomy of innominate artery (IA).
Material and methods. The study included 72 patients with non-syndromic ascending aortic aneurysms, which were divided into 2 following groups depending on IA anatomy: patients with a common origin of innominate and left common carotid artery (CILCA, n=28) and patients with normal vessel (No CILCA, n=44). Based on multispiral computed tomography, the ascending aorta and aortic arch geometry were analyzed in all patients.
Results. Both groups of patients had ascending aortic aneurysm and aortic root dilatation without significant differences. The ascending aortic length in No CILCA patients was 113 [89; 144] mm vs 108 [63; 143] mm in CILCA patients (p=0,021). The length of tubular ascending aorta in No CILCA and CILCA patients was 86 [63; 123] mm and 82 [40; 103] mm, respectively (p=0,018). Compared to patients in the CILCA group, patients with normal IA anatomy were more often diagnosed with type III aortic arch (27,3% vs 3,6%, p=0,017) and less often with type I aortic arch (63,6% vs 89,3%, p=0,036).
Conclusion. Variant IA anatomy ("bovine arch") in patients with ascending aortic aneurysm does not worsen thoracic aortic geometry compared to patients with normal IA anatomy.
- A positive family history for cardiovascular diseases is a significant risk factor for restenosis.
- Restenosis develops significantly more often in men.
- Apolipoprotein A1 has a cardioprotective effect. In patients with restenosis, a significant decrease was revealed.
- A significant increase in alanine aminotransferase levels in patients with restenosis may be a risk factor for restenosis.
Aim. To study risk factors for coronary artery restenosis in a retrospective (identification of patients with restenosis) and prospective (biomarker analysis) study.
Material and methods. Patients with coronary stenosis were identified within 7 years after primary stenting. In 181 patients (67 — with coronary restenosis, 114 — without coronary restenosis), the clinical, demographic and serum biomarker profiles of patients were studied.
Results. The incidence of coronary restenosis was significantly higher in men (82,1% and 69,3%, p=0,047). Propensity score matching was used to balance the groups by sex, and as a result, a higher hereditary predisposition to cardiovascular diseases (p=0,024), sinus rhythm (p=0,020), low serum apolipoprotein A1 (p=0,048) and high alanine aminotransferase (p=0,023) were shown for the restenosis group.
Conclusion. Coronary artery restenosis was characterized by male sex, sinus rhythm, hereditary predisposition, increased alanine aminotransferase and decreased apolipoprotein A1.
CARDIOSURGERY
- Cardiovascular diseases and cancer remain the leading causes of hospitalization and mortality worldwide. In some cases, both diseases occur in one person and require surgical intervention.
- Surgical tactics for managing patients with a combination of hemodynamically significant coronary atherosclerosis and lung tumor have not been determined worldwide.
- The study results are important for the practicing surgeon and cardiologist as they will improve his decision-making process regarding the type of myocardial revascularization in a patient with a lung tumor.
Aim. To compare the immediate and long-term outcomes of surgical treatment of patients with lung tumor and concomitant coronary artery disease (CAD) requiring myocardial revascularization with revascularized patients without a lung tumor.
Material and methods. The work included data on examination, treatment and follow-up of 30345 patients who underwent elective surgery at the Research Institute — Ochapovsky Regional Clinical Hospital № 1 in the period from January 1, 2015 to June 1, 2024. In total, 21909 patients were diagnosed with stable CAD aged 28 to 90 years (mean age, 64,1±12,4 years) and 9426 underwent myocardial revascularization by coronary artery bypass grafting (CABG). Two following groups of patients were formed: Group A — patients with CAD and a lung tumor verified by chest computed tomography, who underwent combined surgery of CABG and lung resection (n=71); Group B — patients with CAD without a lung tumor, who underwent isolated CABG, selected using a random number generator due to the large number of the original cohort (n=154).
Results. Patients from group A had more frequent inhospital complications (acute heart failure 6,86% vs 2,6%, p=0,02; arrhythmias such as atrial fibrillation 15,49% vs 4,55%, p=0,005; pneumonia 16,9% vs 4,55%, p=0,002; shunt thrombosis 2,82% vs 0%, p=0,04; sepsis 8,45% vs 1,3%, p=0,007), which naturally led to an increase in hospital stay length (15,06±8,69 vs 9,36±8,26 days, p<0,001). In group A, 2 patients died during hospitalization due to shunt thrombosis, and in group B no patients died. However, this indicator did not reach statistical significance (p=0,06). In the long-term follow-up period (6 months — 6 years), high mortality was found in patients from group A due to cancer progression, while cardiovascular mortality and ischemic events were comparable in both groups. In addition, the prognosis of patients depended on tumor histology and, predictably, the best long-term survival was in patients with benign lung neoplasms, as well as with lung adenocarcinoma.
Conclusion. Our results have important implications for the practicing surgeon, as they will improve his decision-making process about the revascularization type. However, further studies are needed on the factors underlying the decision to perform CABG in cancer patients, the impact of patient and physician perception of cancer prognosis, and factors associated with survival after CABG among cancer patients.
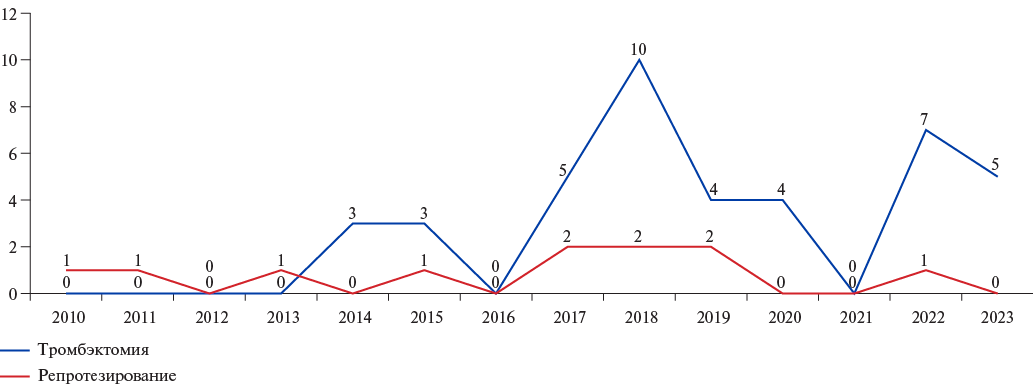
- Errors in anticoagulant therapy are the main cause of artificial heart valve thrombosis.
- The results of thrombectomy are comparable to repeat replacement.
- Thrombectomy can be considered as the intervention of choice in patients with high surgical risk.
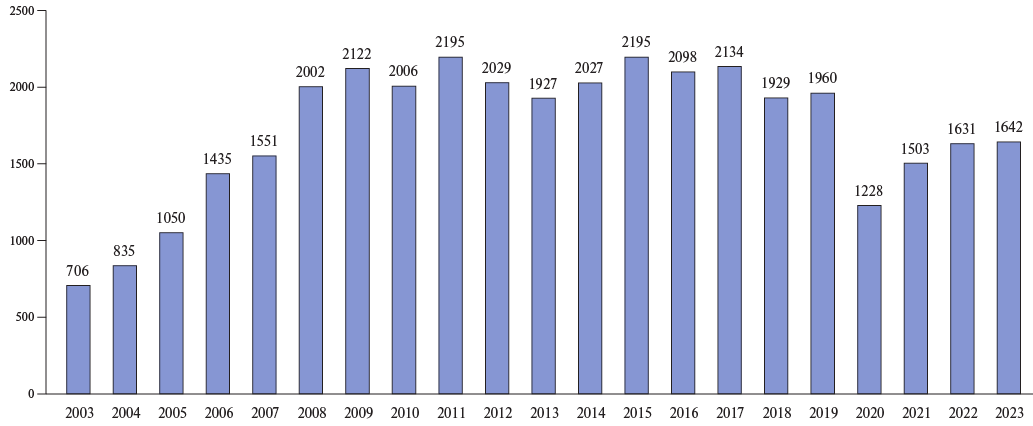
Aim. Comparative analysis of the outcomes of surgical treatment of obstructive prosthetic aortic valve thrombosis (OPVT).
Material and methods. This retrospective analysis of medical records of patients diagnosed with OPVT was performed for the period from 2010 to 2023. In the postoperative period, 49 patients were diagnosed with OPVT and underwent resurgery. Storage and calculation of all data was performed in SPSS 26 (2019) and MS Excel, Word 2016. Data are expressed as mean values, standard deviations or medians. Univariate analysis was performed using Student’s t-test for parametric data. For nonparametric data, the KruskalWallis test was used. Survival analysis was performed using the Kaplan-Meier curves.
Results. Cardiopulmonary bypass and aortic cross-clamp durations were significantly lower than in patients with repeat grafting (84,5±65,1 min, 130,6±36,3 min, P<0,05 and 37,2±14,2 min, 93,7±23,1 min, P<0,05, respectively). Mean intensive care unit stay after thrombectomy was 2,68±1,6 days, while after resurgery — 6,8±6,4 days (P>0,05). In the early and late postoperative periods, no differences were found in the maximum and mean transaortic gradients in patients in both groups. Inhospital mortality was 14,3% (n=7). Operative mortality was 4,1% (n=2). Inhospital mortality was higher in the thrombectomy group, but the differences were not significant. Five-year survival after repeated AV replacement was 82%, and in the thrombectomy group — 70% taking into account inhospital mortality.
Conclusion. The results of prosthetic AV thrombectomy in the early and late periods are comparable with repeat AV replacement data. Thrombectomy is a faster and simpler surgical method for restoring the artificial heart valve function, compared with repeat replacement. The choice of surgical strategy should be based on the intraoperative valve assessment.
GUIDELINES FOR THE PRACTITIONER
- Elderly patients aged over 75 years with ST-segment elevation myocardial infarction (STEMI) are characterized by a higher mortality and bleeding risk.
- Analysis of the FREEDOM registry data, which included more than 6 thousand patients with STEMI over 75 years old, showed that non-immunogenic staphylokinase has a high safety profile in elderly patients.
- When using non-immunogenic staphylokinase, rate of major bleeding does not exceed 1,5%, intracranial hemorrhage and blood transfusions — 1,2%, while hemorrhagic events in patients over 75 years old does not significantly differ from that in patients under 75 years old. The effectiveness of thrombolysis according to ECG data was 65%.
- Non-immunogenic staphylokinase is the preferred drug for prehospital thrombolysis due to the ease of use in a single bolus dose of 15 mg, regardless of the patient’s body weight and a high safety profile, including in elderly patients.
Aim. To assess the safety of reperfusion therapy using non-immunogenic staphylokinase in patients with acute ST-segment elevation myocardial infarction (STEMI) over 75 years old in real-world practice.
Material and methods. FREEDOM registry is a multicenter prospective non-interventional observational study. The registry included patients with an established diagnosis of STEMI who received reperfusion therapy with non-immunogenic staphylokinase (Fortelyzin®, OOO SuperGene, Russia) at a bolus or bolusinfusion dose of 15 mg. The safety criteria were all-cause inhospital mortality, major bleeding rate, and a combination of major adverse cardiovascular and cerebrovascular events (MACСE). The bleeding rate and severity were determined according to the BARC classification. The criterion for the effectiveness of reperfusion therapy was the coronary flow restoration according to electrocardiography data after 90 minutes. The study was conducted in accordance with Declaration of Helsinki and Good Clinical Practice standards.
Results. Monitoring of non-immunogenic staphylokinase use in STEMI from June 1, 2013 to June 14, 2025 covered more than 50 thousand patients; 16% of patients (n=6180) were over 75 years old. The median age in this subgroup of patients was 80 (77-83) years. A total of 91% of patients received prehospital thrombolysis. According to electrocardiography, reperfusion within 90 minutes in the subgroup of patients over 75 years old was achieved in 65% of patients, which is comparable with the subgroup of patients under 75 years old (70%) (p=0,81).
In the subgroup of patients over 75 years old, the MACСE rate was 31,9%, while in patients under 75 years old — 21,8% (p=0,001). In the subgroup of patients aged over 75 years, compared with the subgroup of patients under 75 years, there was a significantly higher prehospital mortality (1,7% vs 1,1%, p=0,03), inhospital mortality (5,6% vs 2,3%, p=0,001), rate of cardiogenic shock (6,9% vs 5,0%, p=0,01) and heart failure worsening (5,4% vs 3,2%, p=0,03).
Intracranial bleeding rate in patients over 75 years of age did not differ significantly compared to the subgroup of patients under 75 years of age (1,2% vs 1,1%, p=0,96). The rate of major bleedings in patients over 75 years of age was 1,5% compared to 1,2% in the subgroup of patients under 75 years of age (p=0,74), blood transfusions — 1,2% vs 1,0% (p=0,83), minor bleedings — 5,3% vs 5,0% (p=0,76). Thus, the safety of non-immunogenic staphylokinase in patients with STEMI over 75 years of age has been proven.
Conclusion. Given the convenience of non-immunogenic staphylokinase use in a single bolus dose of 15 mg regardless of the patient’s body weight and a high safety profile, including in elderly patients over 75 years old, non-immunogenic staphylokinase is the preferred drug for prehospital thrombolysis.
Aim. To evaluate the effectiveness of single-pill combination of indapamide/ amlodipine in outpatients over 55 years of age with uncontrolled isolated systolic hypertension (ISH) in a real-world practice.
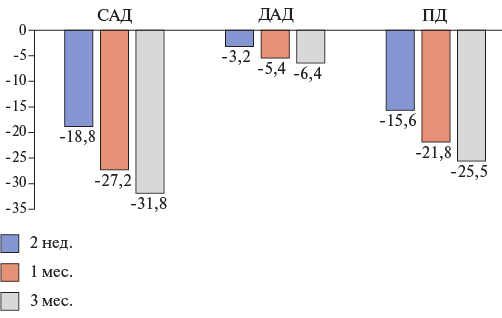
Material and methods. Retrospective analysis of data from participants in the multicenter, open-label observational ARBALET study conducted in Russia among patients with grade 1-2 hypertension without prior antihypertensive therapy or blood pressure (BP) control while taking the medications. The efficacy of indapamide/ amlodipine combination was assessed by changes in office systolic BP (SBP) and the rate of achieving the target SBP level (<140 mm Hg) after 2 weeks, 1 month, and 3 months in four following age groups: 55-59 years, 60-69 years, 70-79 years, and ≥80 years.
Results. The ARBALET study enrolled 2217 patients, of whom 626 had ISH and were included in this additional analysis (mean age 66,1±7,8 years; 165 men (26,4%)). The target SBP <140 mm Hg was achieved in 43%, 75%, and 93% of patients after 2 weeks, 1 month, and 3 months, respectively. Compared with the baseline, SBP decreased by 18,8±10,5 mm Hg, 27,2±10,6 mm Hg, and 31,8±9,9 mm Hg after 2 weeks, 1 month, and 3 months, respectively. The decrease in SBP after 3 months compared with the baseline in the subgroups 55-60 years, 60-69 years, 70-79 years, and ≥80 years was 30,3±9,4 mm Hg, 32,4±9,7 mm Hg, 32,5±10,7, and 28,9±9,6 mm Hg, respectively.
Conclusion. Administration of indapamide/amlodipine combination is associated with a significant reduction in SBP and a high rate of target BP achievement in patients with ISH over 55 years of age in a real-world practice.
- Transthyretin amyloid cardiomyopathy (ATTR-CM) is a frequently unrecognized cause of heart failure with preserved ejection fraction.
- Three or more possible features of ATTR-CM are present in >70% of patients with heart failure with preserved ejection fraction.
- In order to improve the diagnosis of ATTR-CM, awareness of practitioners about the clinical manifestations ("red flags"), existing probability calculators, modern methods of diagnosis and treatment should be increased.
Aim. To assess the prevalence of clinical manifestations of transthyretin amyloid cardiomyopathy (ATTR-CM), as well as to analyze the demographic and clinical characteristics of patients, including paraclinical investigations conducted in this sample, in patients with heart failure with preserved ejection fraction (HFpEF) in Russia according to the real-world study.
Material and methods. As part of the retrospective part, we analyzed the data of patients with HFpEF previously included in a prospective observational multicenter registry study of heart failure in research centers with ability to diagnose ATTR-CM. Symptoms and signs associated with a high probability of ATTR-CM ("red flags") were recorded based on anamnestic and paraclinical data. Based on interim analysis (n=1770, 29,5% of the planned number of patients), we decided to stop the study and not conduct a prospective phase that involved verifying the diagnosis of ATTRCM in patients with a high risk of its presence.
Results. The mean age of the included patients was 69,7±10,0 years (women, 55,8% (n=988)). Left ventricular (LV) posterior wall thickness (PWT) was measured in 1704 (96,3%) patients. It exceeded 12 mm in 287 (16,8%) cases. Possible signs of ATTR-CM were detected in 1702 (96,2%) participants. Three or more possible signs of ATTR-CM were detected in 1262 (71,3%) patients in the general population. Among patients with available LV PWT measurements, 219 (76,3%) participants with thickness >12 mm had ≥3 possible signs of ATTR-CM. Using the risk calculator, only 117 (7,33%) patients had a high probability of this disease.
Conclusion. More than two thirds of patients with HFpEF have several clinical signs associated with a high risk of ATTR-CM. About 7% of patients selected using the risk calculator may be primary candidates for examination to verify the diagnosis. However, determining the optimal algorithm for diagnosing ATTRCM requires further study.
EXPERT CONSENSUS
On December 6, 2024, an Expert Council meeting was held in St. Petersburg on the problem of diagnosis and treatment of resistant hypertension (HTN). The importance of timely detection and treatment of patients with resistant hypertension is determined by a higher risk of myocardial infarction, stroke, heart failure and cardiovascular mortality compared to patients with uncontrolled HTN. The experts discussed the existing evidence base on a new class of aldosterone synthase inhibitors, in particular the baxdrostat.
CLINICAL GUIDELINES
Russian Society of Cardiology (RSC)
With the participation of: The Eurasian Society of Internists, the Society of Specialists in Heart Failure, the Russian Scientific Medical Society of Internists (RNMOT), the Russian Society of Pathologists, the Russian Society of Radiologists and Radiologists (RORR), the National Association of Experts in Sanatorium Treatment
Approved by the Research and Practical Council of the Ministry of Health of the Russian Federation
ISSN 2618-7620 (Online)