ПРОБЛЕМНАЯ СТАТЬЯ
The article discusses the statement of the diagnosis of hypertension (HTN) with severe left ventricular systolic dysfunction and the resulting decrease in systolic blood pressure (BP) to target levels or hypotension ("decapitated hypertension").
The current Russian guidelines on HTN in adults and heart failure (HF) do not consider this situation. The used classifications of HTN by its degree in untreated patients and the achievement of the target BP level by antihypertensive therapy cannot correctly reflect the situation in this case, since HTN as such no longer exists, but the diagnosis as a chronic disease continues to exist.
The authors propose to expand the existing classification by introducing the term "history of HTN", which correctly reflects the discussed period of disease, allows HTN to be included in the diagnosis, substantiates the unacceptability of using antihypertensive therapy in this period, as well as the difficulties in prescribing maximum doses of HF medications.
ПРОГНОЗИРОВАНИЕ
- In women with newly diagnosed breast cancer
(BC), after adjuvant chemotherapy with doxorubicin and cyclophosphamide, changes in the 24-hour blood pressure profile (DBP) are recorded, depending on its initial level. - After chemotherapy with doxorubicin and cyclophosphamide, an increase in arterial stiffness is recorded in patients with BC, which was more noticeable in the comorbidity of BC with masked hypertension and primary hypertension. These changes indicate a structural and functional arterial system restructuring.
- Noninvasive arteriography and 24-hour blood pressure monitoring are informative tools for assessing signs of chemotherapy vascular toxicity in BC women.
Aim. To evaluate arterial stiffness and 24-hour blood pressure (BP) profile in breast cancer (BC) in women with normotension, masked hypertension (MH) and primary hypertension (HTN) before and after chemotherapy (CT) with a combination of doxorubicin and cyclophosphamide.
Material and methods. The study involved 158 women with newly diagnosed stage IIA-IIIA BC. Before chemotherapy, the patients were divided into 2 groups. The first group included 109 women with normal clinical BP, and the second group included 49 women with previously diagnosed stage 1-2 HTN. Before chemotherapy and 7-14 days after its completion, 24-hour ambulatory BP monitoring (ABPM) and noninvasive arteriography were performed. The mean 24-hour systolic BP (SBP) and diastolic BP (DBP), variability, time indices of SBP and DBP, their nighttime decrease and morning rise were analyzed. The pulse wave velocity (PWV) in the aorta, augmentation index (AI), central systolic BP, pulse pressure, systolic and diastolic area indices and their ratio were determined.
Results. According to ABPM conducted before the start of chemotherapy, two subgroups were identified among the examined patients with normal clinical BP. The first group included 55 (50,5%) women with normotension, while the second group — 54 (49,5%) women with newly diagnosed MH. The general trend of ABPM modification after chemotherapy was a decrease in mean 24-hour SBP and DBP, their excessive variability and a tendency towards tachycardia. Doxorubicin and cyclophosphamide-based chemotherapy is associated with an increase in PWV and AI in all groups of subjects, indicating an increase in arterial stiffness. These changes were more pronounced in the case of comorbidity of BC with MH and primary HTN.
Conclusion. In BC women, a comprehensive assessment of the 24-hour BP profile and arterial stiffness, glomerular filtration rate and left ventricular myocardial ejection fraction is an informative tool for the timely detection of chemotherapy vascular toxicity and the prevention of adverse cardiovascular events.
- In patients with ischemic stroke and elevated lipoprotein(a) (Lp(a)) levels, in addition to traditional cardiovascular risk factors, factors such as hemostasis disorders and elevated inflammatory markers are important.
- Identification of these factors and subsequent correction of therapy will help reduce the risk of life-threatening complications in these patients.
Aim. To identify the features of lipid profile, coagulation system, inflammation markers and the severity of neurological status in patients with ischemic stroke (IS) and elevated lipoprotein(a) (Lp(a)).
Material and methods. The study included 109 patients (mean age 53,7±7,76 years) with ischemic stroke, multifocal atherosclerosis (MFA) and stage 3 hypertension (HTN). Depending on the Lp(a) level, the patients were divided into 2 groups. In group 1, 85 patients (78%) had Lp(a) ≤50 mg/dL, while in group 2, 24 patients (22%) had Lp(a) >50 mg/dL. All patients were assessed for lipid profile, coagulation system, high-sensitivity C-reactive protein, and interleukin-6.
Results. The target low-density lipoprotein cholesterol level <1,4 mmol/L was not achieved in any group, while all lipid profile parameters did not differ between the groups. Global hemostasis assay parameters (clot growth rate, clot size) were significantly higher in patients with Lp(a) levels >50 mg/dL. This group also had higher interleukin-6 levels (119,9 pg/ml vs 7,4 pg/ml, p<0,01) and stroke severity according to the National Institutes of Health Stroke Scale (5,7 vs 3,3, p<0,01).
Conclusion. Elevated Lp(a) levels in patients with HTN and MFA who have had ischemic stroke are a risk factor that affects the severity of neurological manifestations of ischemic stroke and is associated with hypercoagulation and inflammation. Treatment options aimed at elevated Lp(a) levels are limited, so early detection and timely correction of modifiable risk factors are necessary.
- The development of restenosis after carotid endarterectomy is a pressing issue.
- The following most significant predictors of restenosis have been identified: dyslipidemia, increased body weight, impaired carbohydrate metabolism, decreased glomerular filtration rate, and initially elevated fibrinogen levels.
- The variety of factors causing restenosis requires a comprehensive approach to postoperative patient management, which can ensure more accurate prediction and development of prevention measures.
Aim. To determine predictors of carotid artery restenosis in patients after carotid endarterectomy (CEA).
Material and methods. The study included 100 patients with stenosing carotid atherosclerosis who underwent CEA. We performed biochemical and clinical screening tests, computed tomography angiography and carotid duplex ultrasound before and after surgery. The median follow-up was 1,9 years [1,4;2,25]. During the prospective follow-up, we selected patients with postoperative restenosis and a control group of patients without restenosis with most complete data on postoperative period, including carotid duplex ultrasound and end points. The final analysis included 76 patients as follows: 55 men (mean age, 67 years) and 21 women (mean age, 66,5 years). Depending on the degree of restenosis, patients were divided into following groups: no restenosis (0-19%), moderate restenosis (20-50%), significant restenosis (from 51%).
Results. According to multivariate regression analysis, the key predictors of restenosis were glucose level, atherogenicity coefficient and glomerular filtration rate (GFR). Significant parameters associated with the severity of restenosis were GFR, glucose level, linear blood flow velocity after surgery, body mass index and age (all laboratory parameters were assessed before surgery). In patients without restenosis, differences were observed compared to the group with moderate restenosis in such factors as atherogenicity coefficient, fibrinogen, glucose and prothrombin levels, as well as smoking. In addition, the group with severe restenosis showed significant differences from the group without restenosis in GFR. The incidence of restenosis increases 12 months after surgery, reaching its peak by two years of follow-up. We did not reveal significant associations of the type of surgery (classical/eversion CEA) with various postoperative complications, with the exception of thrombosis in the early postoperative period.
Conclusion. Thus, according to our study, the likelihood of restenosis was associated with traditional risk factors for cardiovascular diseases, such as impaired carbohydrate and lipid metabolism, inflammation, decreased GFR and obesity, and raises with an increase in the postoperative follow-up period. The data obtained suggest that the mechanisms underlying the pathogenesis of restenosis are similar to those leading to atherosclerosis.
- Comparative evaluation of data from echocardiography performed on the first day revealed that patients with myocardial infarction with non-obstructive coronary artery disease (MINOCA) have smaller values of end-systolic diameter, end-diastolic volume (EDV), end-systolic volume than patients with single-vessel disease.
- Left ventricular global function index in patients with myocardial infarction with obstructive coronary artery disease (MICAD) depends on the infarct location. Patients with low GFI in this group (in contrast to MINOCA) more often had anterior involvement.
- Evaluation of patients with low GFI in the MICAD and MINOCA revealed that patients with obstructive CAD more often have ST elevation, pathological Q wave, and higher EDV.
Aim. To assess the main parameters of transthoracic echocardiography, including the global function index in patients with myocardial infarction with obstructive (MICAD) and non-obstructive coronary artery disease (MINOCA).
Material and methods. The study included 170 patients with a diagnosis of myocardial infarction were hospitalized and underwent inpatient treatment at the Cardiology Department № 1 of the Republican Clinical and Diagnostic Center, Izhevsk. Coronary angiography was performed on a Phillips Allure Clarity system. Based on the procedure results, the patients were divided into 2 following groups: 1 — MINOCA (n=73); 2 — MICAD (n=97), who underwent stenting. Echocardiography was performed using a Siemens Acuson CV70 (Germany) for all patients on the first day of the disease (before coronary angiography). The main parameters of the left ventricle (LV) geometry were assessed. LV ejection fraction (EF) was determined using the Simpson method. The LV global function index (LVGFI) was determined using the following formula: LVGFI=stroke volume/ ((LV end-diastolic volume (EDV) + LV end-systolic volume (ESV))/2 + LV volume) × 100%. Based on the echocardiography data, the patients were divided into 2 following subgroups: 1 — low GFI (<31,2%), 2 — normal GFI (>31,2%).
Results. No differences in age were found. In the MINOCA group, there were more females — 57,6% vs 29,9%. Patients with MICAD more often had ST elevation and pathological Q wave — 70% vs 33%. Anterior wall MI was equally common. Patients with MICAD had a larger left atrium diameter and EDV. No differences were found in other echocardiographic parameters. EF was higher in patients in the MINOCA group (trend towards differences). Patients with low GFI in the MINOCA group are older, has a larger left atrium diameter, right atrium, end diastolic dimension, EDV, ESV, LV mass, and a higher rate of LV hypertrophy (40% vs 12,5%, p=0,008). LVEF in the low GFI MINOCA group was 55% (vs 64,9% in MICAD, p=0,004). In both subgroups, patients had the same frequency of ST elevation and pathological Q wave. Patients with low GFI, obstructive coronary artery disease and male sex more often had ST elevation and pathological Q wave.
Conclusion. In patients with MINOCA, LV geometry parameters on the first day of the disease are better than in patients with MICAD due to lower values of the end-systolic dimension, EDV, ESV. Patients with low GFI had higher values of the end-diastolic dimension, EDV, ESV, LV mass, and more often had LV hypertrophy, lower EF. Patients with low GFI in the MICAD group compared to low GFI in MINOCA showed differences in sex (more often men), ST elevation rate, pathological Q wave, and a higher EDV.
CARDIAC DYSRHYTHMIAS
What is already known about the subject?
- Around one third of cardiac resynchronization therapy (CRT) patients fail to respond appropriately as they cannot reach certain treatment goals within the desired period of time. There is a variety of CRT implantation strategies and none has ultimate benefits over others.
What might this study add?
- Electrocardiography-based left ventricular lead positioning approach assessed by right ventricular-left ventricular activation delay was found to be a significant predictor of QRS complex duration, mortality and rehospitalisation rates in CRT patients with NIHA class III and IV heart failure associated with ventricular dyssynchrony.
There is a variety of cardiac resynchronization therapy (CRT) strategies and none has ultimate benefits over the others.
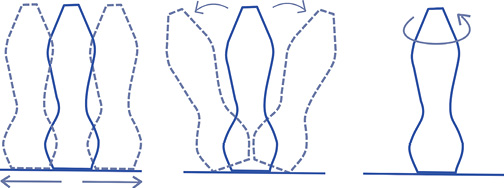
Aim. To evaluate the influence of two strategies of left ventricular (LV) electrode implantation on the development of cardiovascular events in patients with chronic cardiac failure.
Material and methods. This was a randomized controlled clinical trial designed to compare the effectiveness of traditional anatomy-guided LV lead positioning strategy towards the electrocardiography-guided implantation approach in an optimal branch of the coronary sinus vein, being the closest to the latest electrically activated myocardial region.
Results. We enrolled 63 patients with NYHA class III or IV chronic heart failure with ventricular dyssynchrony, an LV ejection fraction (LVEF) less than 35%, an LV end diastolic dimension exceeding 150 ml, a QRS interval over 130 ms. The survival time in electrocardiography-guided approach (study group) was equal to 11,22 months, which was significantly lower in the anatomy-guided approach (control group). Time to re-hospitalization in a study group was nearly two times longer as compared with that in patients from the control group (10,188 months versus 5,548 months). LVEF was significantly higher in the study group with median value equal to 39% versus that in the control group equal to 35% (р=0,002).
Conclusions. The results of the present study demonstrate that electrocardiographyguided approach has benefits over traditional anatomy-guided approach in terms of improved cardiac structure and function in patients with NYHA class III and IV heart failure associated with ventricular dyssynchrony.
- Left atrial myocardial fibrosis is an independent risk factor for arrhythmia recurrence after catheter ablation.
- Arrhythmia recurrence is more common in patients who had SARS-CoV-2 infection before surgery.
- Catheter ablation methods aimed at isolating left atrial posterior wall myocardial fibrosis do not reduce the likelihood of arrhythmia recurrence in SARS-CoV-2 convalescents.
Aim. To determine the prognostic significance of left atrial (LA) changes after SARS-CoV-2 infection on the atrial fibrillation recurrence rate after catheter ablation.
Material and methods. The study involved 40 patients. All patients were monitored after 3, 6 and 12 months, as well as when the clinical performance of the disease changed. The average follow-up time was 19±3 months. Recurrence of atrial fibrillation was observed in 18 patients (45%).
Results. The study groups were completely comparable in age (p=0,382), sex (p=0,604), arrhythmia type (p=0,842), and history of previous surgeries (p=0,949). Arrhythmia recurrence was 9,33 [2,18; 39,96] times more common in patients who had SARS-CoV-2 infection before surgery (p=0,01). Arrhythmia recurrence after catheter ablation caused by left atrial posterior wall fibrosis and without pulmonary vein reconnection is an independent risk factor for recurrence after another ablation attempt (p=0,020). Also, arrhythmia recurrence was 9 [2,09; 38,79] times more common in patients after left atrium posterior wall box isolation (p=0,002). About half of the atrial area in patients with arrhythmia recurrence is represented by myocardium with an amplitude of less than 0,25 mV. In patients without recurrence, the area with this amplitude is on average 15,9% smaller (49±18,4% and 33,1±17,5%, respectively; p=0,020). Differences in the myocardial area with an amplitude of less than 0,5 mV are more pronounced and average 21,4% (p=0,006). LA myocardial tissue with normal signal amplitude (>0,75 mV) is represented by only 17,4% of the area in patients with disease recurrence, which is 2,14 times less than in patients with remission (p=0,011).
Conclusion. LA myocardial changes after SARS-CoV-2 infection are stable over time and significantly increase the arrhythmia recurrence risk after catheter ablation. Additional left atrial posterior wall box isolation does not reduce the risk of recurrence and does not significantly affect the duration of sinus rhythm control.
Aim. Many patients with conduction system disorders have associated heart conditions, especially ischemic heart disease. This study was designed to assess the prevalence and pattern of coronary artery disease (CAD) in patients with bradyarrhythmias requiring permanent pacemaker and association with CAD risk factors.
Material and methods. This single-centre observational cohort study included 80 patients with mean age of 63±9.4 years, admitted with symptomatic bradyarrhythmias. Patients underwent coronary angiography after obtaining informed consent and prevalence and pattern of CAD were analyzed in them. CAD was defined as narrowing in major epicardial coronary arteries or their first order branches and obstructive CAD as ≥50% stenosis. CAD was further categorized as single vessel disease, double vessel disease and triple vessel disease and any association with conduction system disorders studied.
Results. CAD was present in 56% patients and obstructive CAD in 37.5% patients. 19% patients had single vessel disease, while 18% had multi-vessel CAD. Obstructive LAD disease was seen in 25% of patients, followed by right coronary artery in 21.3% patients and LCX in 15% of patients. Heart team advised revascularization in majority (75%) of patients with obstructive CAD. AV nodal artery disease was found more in patients of complete heart block (p=0.0359). Among various risk-factors, dyslipidemia (56.7% vs 22%, p=0.0016), family history of CAD (63.3% vs 18%, p<0.0001) and angina (53.3% vs 20%, p=0.0020) showed significant association with obstructive CAD. RWMA on echocardiography (50% vs 14%, p=0.0004) and lower mean left ventricular ejection fraction (52.7% vs 58.1%, p=0.0270) also showed significant association with obstructive CAD.
Conclusion. In patients requiring permanent pacemaker, coexistent obstructive CAD was noted in 37.5% of the subjects. Causal association between obstructive CAD and conduction disturbances may not be established from this data, but the increased prevalence of atherosclerotic cardiovascular disease in patients having bradyarrhythmias implies the need for larger multi-center trials to understand the causal association and plan for earlier management.
- All patients with left bundle branch block are characterized by a significant myocardial wasted work.
- Wasted work makes a significant contribution to the decrease in global myocardial work in patients with dilated cardiomyopathy.
- In patients with idiopathic left bundle branch block and patients with right ventricular pacing and normal systolic function, wasted work resulting from impaired cardiac electric propagation does not affect global myocardial work.
Aim. To evaluate myocardial function in different groups of patients with left bundle branch block (LBBB) and the LBBB "model" — right ventricular pacing (RVP).
Material and methods. Global longitudinal strain (GLS) and myocardial function parameters, such as global constructive work (GCW), global wasted work (GWW), global work index (GWI), and global work efficiency (GWE), were measured in 25 patients with dilated cardiomyopathy (DCM) and LBBB (DCM-LBBB group), 20 patients with DCM and a narrow QRS complex (DCM-nonLBBB group), 15 patients with LBBB developed after transcatheter aortic valve implantation (TAVI LBBB group), 12 patients with idiopathic LBBB (I-LBBB group), 27 patients with permanent RVP, and 10 healthy volunteers (HVs). The segments with maximum and minimum GWI were determined in all patients.
Results. The GLS, GWI and GCW values were comparable in the I-LBBB and RVP groups, and were significantly lower in the TAVI-LBBB and both DCM groups than in HVs (p=0,049, 0,006, 0,025; p<0,001, respectively). Patients in the I-LBBB, TAVI-LBBB, RVP and DCM-LBBB groups were characterized by an increased GWW value (261 [203,5; 291,5], 273 [184,8; 385,3] and 237 [149,5; 445,3] versus 108 [74,3; 137,3] mm Hg%, p=0,033, 0,006, <0,001, <0,001, respectively), while the GWW value in the DCM-LBBB group was the highest (346,5 [255,5; 437,8] mm Hg%). The GWW value was associated with the QRS width (r=0,456, p<0,001). The GWE value was reduced in the I-LBBB, TAVI-LBBB, RVP and DCM-LBBB groups compared to HVs (p=0,033, 0,007, 0,023, <0,001, respectively). The area of maximum GWI was located in the posterolateral wall, and the minimum GWI in the interventricular septum in most patients with LBBB, while in the RVP group it was very diverse.
Conclusion. Despite the fact that all patients with an electrical activation pattern corresponding to LBBB are characterized by significant wasted work, its contribution to the global myocardial work is significant only in patients with DCM. Lost work does not lead to a decrease in constructive work in patients with I-LBBB and RVP and normal left ventricular systolic function.
LIPID METABOLISM DISORDERS
- Hypertriglyceridemia is associated with an increased risk of cardiovascular events and acute and chronic pancreatitis.
- Increased triglyceride levels can be caused by primary genetic disorders, secondary factors, or a combination of both, which are widespread in the population.
- Primary and secondary hypertriglyceridemia differ in the pathogenesis of lipid disorders, the profile of triglyceride-rich lipoproteins, which requires differentiated approaches to diagnosis and treatment.
Hypertriglyceridemias are a heterogeneous group of pathologies differing in the mechanisms of triglyceride-rich lipoprotein increase, the composition of lipoproteins and related risks. This review article presents information on the profile and pathogenesis of various primary and secondary hypertriglyceridemias, as well as describes current potential of genetic diagnostics, drug and non-drug correction.
CLINIC AND PHARMACOTHERAPY
- All patients with stable coronary artery disease and a high risk of ischemic events without a high risk of bleeding are recommended to consider adding a second antiplatelet agent or the anticoagulant rivaroxaban at a dose of 2,5 mg 2 times a day to acetylsalicylic acid.
- Laboratory effects reflecting the hemostasis status and pharmacodynamics of the original rivaroxaban (Xarelto, AO Bayer, Germany) at a dose of 2,5 mg 2 times a day and generic rivaroxaban (Kruoksaban, Ozon LLC, Russia) will be studied.
The course and complications of coronary artery disease (CAD) are associated with atherosclerosis progression and a high probability of atherothrombosis. Antithrombotic therapy is the most effective strategy for preventing cardiovascular events in atherosclerotic diseases. In accordance with current clinical guidelines for the prevention of myocardial infarction and stroke, all patients with stable CAD are recommended to take acetylsalicylic acid (ASA). In patients with a high risk of ischemic events without a high risk of bleeding, addition of low dose anticoagulant rivaroxaban to ASA is possible. The article discusses the design of a clinical and laboratory prospective single-center comparative study, the purpose of which is to compare the efficacy and safety of two following bioequivalent agents: the original (Xarelto, AO Bayer, Germany) and generic (Kruoksaban, OOO Ozon LLC, Russia) rivaroxaban.
- Non-immunogenic staphylokinase has high thrombolytic activity and fibrin selectivity.
- The FORPE-2 clinical trial has a multicenter, double-blind, randomized, placebo-controlled design that examines the efficacy and safety of non-immunogenic staphylokinase in patients with intermediate-high risk pulmonary embolism.
Aim. To evaluate the efficacy and safety of single bolus administration of non-immunogenic staphylokinase in comparison with placebo in patients with intermediatehigh risk pulmonary embolism (PE) within the FORPE-2 clinical trial.
Material and methods. Non-immunogenic staphylokinase has high thrombolytic activity and fibrin selectivity. The FORPE-2 clinical trial has a multicenter, doubleblind, randomized, placebo-controlled design. In clinical sites, patients (486 in total, with a possible 10% dropout rate) with confirmed PE and evidence of right ventricular dysfunction based on computed tomography pulmonary angiography and an increased risk of hemodynamic instability (intermediate-high-risk PE) will be equally randomized into two groups to receive non-immunogenic staphylokinase or placebo. The study protocol provides inclusion and exclusion criteria, calculation of the required patient sample size, and the study plan. The primary efficacy endpoint will be a composite of all-cause mortality, hemodynamic collapse, and recurrent PE within 30 days of randomization. Safety endpoints will be hemorrhagic stroke during hospitalization and BARC type 3 and 5 bleeding types.
Results. The study will provide data on the efficacy and safety of non-immunogenic staphylokinase in patients with intermediate-high risk PE. A report will be compiled with individual data and statistical analysis of the results.
- CASCADE is the first study comparing the effect of enteric-coated and buffered acetylsalicylic acid (ASA) on platelet aggregation in patients with type 2 diabetes and coronary artery disease (CAD).
- The primary endpoint is the incidence of ASA nonresponsiveness.
- One of the factors in the development of recurrent cardiovascular events may be ASA nonresponsiveness.
- The rate of buffered ASA nonresponsiveness is lower than in enteric-coated ASA group.
- The CASCADE results may have a significant impact on clinical practice if its data are further confirmed by large interventional studies (including crossover designs) and implemented for treatment.
Background. There is a lack of data on the incidence of aspirin nonresponsiveness and the efficacy of different forms of ASA in patients with diabetes.
Aim. To evaluate the efficacy of buffered versus enteric-coated ASA based on the frequency of high residual platelet reactivity (HRPR) as measured by the VerifyNow Aspirin Test in patients with chronic coronary syndrome (CCS) and type 2 diabetes (T2D).
Material and methods. The single-center observational parallel-group comparative study (CASCADE) included patients over 18 years of age with CCS and T2D who were prescribed a buffered form of ASA (Cardiomagnyl 75 mg/day) or an entericcoated form of ASA (Thrombo ACC® 100 mg/day or Aspirin® Cardio 100 mg/day) in routine practice prior to inclusion in the study and were randomly selected from the general consultative and diagnostic department of the hospital. According to the routine prescribed therapy, patients were divided into 2 following groups: patients taking Cardiomagnyl 75 mg/day; patients taking Thrombo ACC® 100 mg/day or Aspirin® Cardio 100 mg/day. At the first visit patients signed informed consent and received a card to assess the compliance of ASA intake, while at the second visit (after 7 days with 100% compliance) patients underwent laboratory assessment of ASA efficacy by VerifyNow Aspirin Test and light transmission aggregometry according to a special protocol including arachidonic acid induction. And the third visit included a call to the patient after 90 days, according to which information was collected about all events that occurred with the patient since the signing of the informed consent. The primary endpoint of the study was the incidence of HRPR on the background of ASA administration according to the VerifyNow Aspirin Test. The primary endpoint, tolerability and safety were evaluated in all patients included in the study. This study was registered at ClinicalTrials.gov, NCT06716255, and is currently completed.
Results. Between February 28, 2024, and May 17, 2024, 200 patients were screened and 84 were successfully enrolled in the study, of which 42 patients received the enteric-coated ASA (Thrombo ACC® 100 mg/day, n=21; Aspirin® Cardio 100 mg/day, n=21) and 42 patients received the buffered ASA absorbed in the stomach (Cardiomagnyl 75 mg/day). The mean age of the study subjects was 68,9 years (standard deviation ±10,2); 34 (40,5%) patients were female and 50 (59,5%) were male. The study was terminated early because of larger than expected intergroup differences. At the time of the interim analysis (May 17, 2024), the incidence of HRPR according to the VerifyNow Aspirin Test was higher in the group of patients receiving the enteric-coated ASA (10 (23,8%) vs 3 (7,1%), p=0,035). By day 90, the incidence of composite endpoint (all-cause mortality; hospitalization for any cause; any ischemic (thrombotic) events) in the buffer ASA group was 7,1% (n=3), which was lower than in the enteric-coated ASA group, which was 16,7% (n=7), mainly due to hospitalisations. However, there were significant associations (p=0,178). One ischemic event was recorded in the enteric-coated ASA group, and there were no ischemic events in the buffered ASA group (p=0,314). There were no fatal outcomes in both groups during the follow-up period. At the same time, the rate of haemorrhagic events in patients with CCS and T2D while taking buffered and enteric-coated ASA was 3 (7,1%) and 4 (9,5%), respectively (p=0,693).
Conclusion. Administration of a buffered form of ASA absorbed in the stomach in a group of patients with T2D could potentially allow for a reduction in the number of ASA nonresponsiveness, which could further lead to a reduction in the number of significant clinical events without loss of safety.
SUPPORTING A PRACTITIONER
Inflammatory involvement of the pericardium (ranging from effusion to wall thickening), whether accompanied by chest pain or not, presents challenges not only in diagnosis and therapy, but also in examination, due to the diverse etiologies of pericardial disease.
This article reviews current approaches to the diagnosis and treatment of patients with pericardial effusion and pericarditis, which may manifest as chest pain or proceed asymptomatically. Anatomical and physiological characteristics of the pericardium, mechanisms of effusion development and tamponade are described. Diagnostic algorithms for chest pain syndrome typical for pericarditis and asymptomatic effusion are provided. The article includes recommendations for differential diagnosis of pericardial inflammation causes, an analysis of complication risks, and indications for anti-inflammatory therapy and interventional procedures. Emphasis is placed on optimizing patient management through risk stratification and clinical performance.
Russian Society of Cardiology (RSC)
With the participation of: Medical Research and Educational Center of Lomonosov Moscow State University (Moscow), Chazov National Medical Research Center of Cardiology (Moscow), Bakulev National Medical Research Center of Cardiovascular Surgery (Moscow), Almazov National Medical Research Center (St. Petersburg), Meshalkin National Medical Research Center (Novosibirsk), Cardiology Research Institute of Tomsk National Medical Research Center (Tomsk), Tyumen Cardiology Research Center of Tomsk National Medical Research Center (Tyumen), Peoples’ Friendship University of Russia (Moscow), Kazan State Medical Academy (Kazan), Federal Center for Cardiovascular Surgery (Khabarovsk)
ISSN 2618-7620 (Online)