ORIGINAL ARTICLES
Aim. To study the prevalence of myocardial infarction (MI) in the population of Russian regions and its contribution to cardiovascular events.
Material and methods. The analysis material was representative samples of the population aged 35-64 years from 11 Russian regions, examined within the multicenter study “Epidemiology of Cardiovascular Diseases and their Risk Factors in Regions of Russian Federation”. The response rate was about 80%. The study used a community-based systematic stratified multiply random sample. During the study, information on prior MI was obtained using a standard questionnaire. Anthropometry and measurement of blood pressure (BP) and heart rate (HR) with an automatic BP monitor were performed. Resting electrocardiography (ECG) was performed, followed by Minnesota coding. Major and minor QQS waves and STT segments were considered as ischemic ECG abnormalities. Biochemical parameters were determined using an Arkhitect 000 Clinical Chemistry Analyzer. The median prospective follow-up was 6,21 [5,25; 6,75] years. A composite endpoint (CE) was analyzed, including cardiovascular death and non-fatal MI. During the follow-up period, 363 all-cause deaths were detected, of which 134 were from cardiovascular diseases, while 196 — CEs. Statistical analysis was carried out in R 3.6.1 environment.
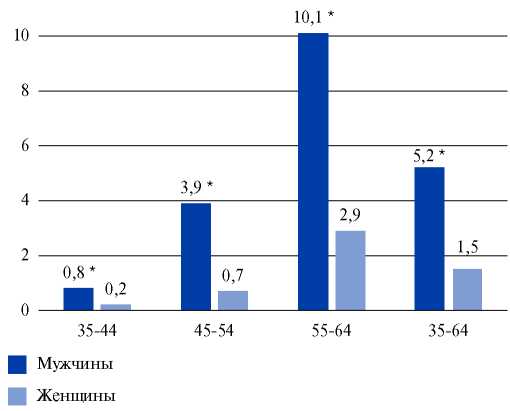
Results. The MI prevalence among the Russian population was 2,9%; 5,2% for men and 1,5% for women, increasing with age. Men with prior MI were more likely to take statins and beta-blockers than women as follows: 39,0% vs 25,6% and 29,3% vs 27,1%, respectively. MI newly diagnosed within the follow-up period was associated with the following risk factors (RFs): smoking, increased BP, HR, triglycerides and glucose. For individuals with prior MI, a significant relationship was found only with smoking. Multiple comparison of the contribution of RFs, ECG abnormalities, and prior MI showed that the inclusion of ischemic ECG abnormalities in the analysis significantly increases the risk of cardiovascular events in individuals without prior MI compared with individuals without both MI and ECG changes. A high CE risk was noted in patients with prior MI: relative risk (RR), 4,73 (2,92-7,65); the addition of ischemic ECG abnormalities increased the RR to 5,75 (3,76-8,8).
Conclusion. The RR of CEs in patients with prior MI without or with ischemic ECG changes is 4,73 and 5,75 times higher than in patients without MI and ECG abnormalities. The risk factors identified in this case cannot explain such an increase in CEs. It is obvious that people with prior MI need rehabilitation. The presence of RFs in patients with newly diagnosed MI indicates insufficient primary prevention, which suggests that strengthening preventive measures to eliminate conventional risk factors in patients with newly diagnosed MI will help reduce the risk of recurrent MI or cardiovascular mortality.
Aim. To evaluate the contribution of subclinical atherosclerosis to the stratification of patients with a SCORE risk of cardiovascular events (CVEs) <5% based on a 10-year follow-up.
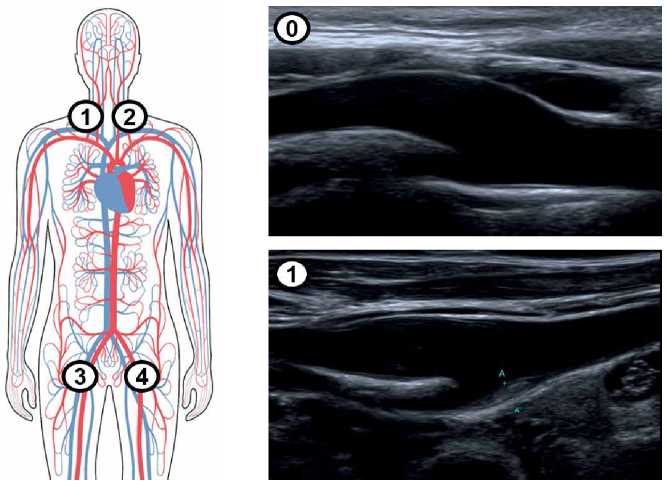
Material and methods. The study included 379 patients with SCORE risk of CVEs <5% (82 men, 297 women). In 2009, all patients underwent clinical examination, carotid artery (CA) ultrasound with the detection of plaques, total CA occlusion, intima-media thickness (IMT) of the common carotid artery (CCA). The plaque number was determined as the total number of all plaques in 6 following segments: both CCAs, both CCA bifurcations and both internal carotid arteries. The total stenosis was calculated as the sum of stenoses in 6 CA segments in %. In 2019, a telephone survey of patients was conducted with a questionnaire assessing the following CVEs: all-cause death, cardiovascular death, myocardial infarction (MI), stroke, myocardial revascularization, cardiovascular hospitalizations, and composite endpoint.
Results. The initial patients’ age ranged from 35 to 67 years (51,1±7,5 years). Plaques from 20% to 50% were detected in 303 participants (79,94%). Over the past 10 years, there have been 5 cardiovascular deaths (1,3%), 7 MIs (1,8%), 5 cases of unstable angina (1,3%), 12 cases of myocardial revascularization (3,2%), 15 strokes (4,0%), 51 cardiovascular hospitalizations (13,5%). The proportion of patients with registered endpoints (CVE+) was 22,4% (n=85). The groups of patients with and without CVEs differed in the level of systolic blood pressure (BP) and blood triglycerides, and did not differ in the level of diastolic BP, lipid profile, glucose, heart rate, smoking status, sex, and age. In the CVE+ group, there were higher values of CCA IMT (0,65 (0,64; 0,70) mm vs 0,62 (0,62; 0,66) mm, p<0,05), total CA stenosis (102,5 (88,1; 120,8)% vs 80 (72,5; 88,1)%, p=0,01), and the CA plaque amount (4,0 (2,8; 3,9) vs 3,0 (2,6; 3,1), p=0,01), respectively. Total CA stenosis was an independent predictor of CVEs when adjusted for sex, age, systolic and diastolic BP (β=0,149; p<0,05), but not for lipid profile. A ROC-analysis revealed a cut-off point for total CA stenosis of 82,5% (AUC=0,598, 95% confidence interval 0,5243-0,673, p<0,05).
Conclusion. The total CA stenosis has shown itself to be an independent predictor of CVEs in patients with a SCORE risk <5%.
Aim. To evaluate the prevalence of familial hypercholesterolemia (FH) and hyperlipoproteinemia(a) (HLP(a)) in patients with premature acute coronary syndrome (ACS).
Material and methods. The study included 120 patients with ACS up to 60 years (mean age, 53±7 years, 104 (87%) men) and 44 people from the comparison group without atherosclerotic cardiovascular diseases and dyslipidemia (mean age, 48±11 years, 19 (43%) men). All patients with ACS underwent coronary angiography. The lipid profile and lipoprotein(a) (Lp(a)) were determined in all patients.
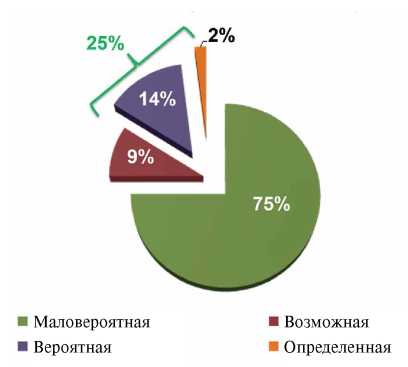
Results. The prevalence of HLP(a) in patients with premature manifestation of ACS was 41% (n=49), possible FH — 25% (n=30), combination of FH and HLP(a) — 13% (n=15). In the comparison group, an increased concentration of Lp(a) was detected in 14% (n=6). Based on the analysis of operating characteristic curves, Lp(a) ≥30 mg/dL had the maximum significance for ACS with a sensitivity of 40% and a specificity of 86% (area under the curve, 0,6; 95% confidence interval (CI), 0,5-0,7, p<0,05), and Lp(a) >15 mg/dl was associated with two or more coronary artery lesions with a sensitivity of 67% and a specificity of 65% (area under the curve, 0,7; 95% CI, 0,6-0,7, p<0,01). On logistic regression analysis, age (odds ratio (OR). 1,1; 95% CI, 1,0-1,2, p<0,05), smoking (OR, 7,5; 95% CI, 2,5-22,0, p<0,001) and Lp(a) ≥30 mg/dl (OR, 6,7; 95% CI, 1,1-39,7, p<0,05) are independently associated with premature ACS. Only Lp(a) ≥15 mg/dL was associated with multivessel coronary artery disease in these patients (OR, 3,8; 95% CI, 1,52-9,74, p<0,01).
Conclusion. Every fourth patient with premature ACS has FH, while almost every second has HLP(a), and every eighth has a combination of FH and HLP(a). HLP(a) is associated with ACS up to 60 years of age and multivessel coronary artery disease in these patients.
Aim. To assess the efficacy and safety of 6-month combined lipid-lowering therapy with a PCSK9 inhibitor in patients with very high cardiovascular risk (CVR).
Material and methods. This prospective, open-label, single-center exploratory research study with active treatment included 5 outpatients with very high CVR. So, 80% of patients had prior coronary artery disease, 20% peripheral arterial disease, and 60% old myocardial infarction. The key inclusion criterion was the failure to achieve the target low-density lipoprotein cholesterol (LDL-C) <1,4 mmol/l with high-intensity statin monotherapy at the maximal tolerated doses or combination therapy with ezetimibe. On a regular basis, all included patients took atorvastatin 40-80 mg/day or rosuvastatin 20-40 mg/day, or pitavastatin 2-4 mg/day. In addition, 2 patients received a statin in combination with ezetimibe 10 mg/day. Patients were followed up for 6 months as follows: every 2 weeks, with a lipid profile monitoring, subcutaneous injections of alirocumab at a dose of 150 mg/ml were performed. Additionally, clinical and laboratory indicators of the safety of therapy were evaluated.
Results. After 6 months, with the combined lipid-lowering therapy with alirocumab, a decrease in median LDL-C from 4,3 (4,11-4,67) to 1,27 (1,06-1,47) (p=0,001) mmol/l, total cholesterol from 6,1 (6-7) to 3,7 (3,5-3,9) (p=0,018) mmol/l, atherogenic index from 3,2 (3-3,26) to 0,8% (0,8-1,5) (p=0,001). There was no significant decrease in median triglycerides and an increase in median high-density lipoprotein cholesterol. Six-month lipid-lowering therapy with a PCSK9 inhibitor had no adverse events and made it possible to achieve a maximum decrease in LDL-C by an average of 75,4% already by 4 months of treatment in actual clinical practice.
Conclusion. Six-month combined lipid-lowering therapy with alirocumab 150 mg subcutaneously every 2 weeks in very high-risk patients allows the majority of patients to achieve target LDL-C values.
Aim. To investigate the prognostic significance of the Atherosclerosis Burden Score (ABS) in relation to the development of major adverse cardiovascular events in patients of different cardiovascular risks (CVR) aged 40 to 64 years.
Material and methods. Men and women aged 40 to 64 years were included in the study. All the patients underwent duplex scanning of the carotid arteries and lower limb arteries. The total ABS was calculated by assessing the presence of plaque in the carotid and femoral bifurcations on both sides. The combined endpoint was cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, or peripheral artery revascularization.
Results. The study included 232 patients who met the inclusion criteria, with a median age of 55,0 years. Very high CVR was established in 94 (40,5%) patients, while high CVR — in 48 (20,7%) patients, and low and intermediate CVR — in 90 (38,8%) patients. The follow-up period lasted 23,6 (15,5; 51,2) months, providing 632,6 patient-years of follow-up. Events within composite endpoint occurred in 28 (12,1%) patients. Increased cumulative risk of adverse cardiovascular events was observed for ABS ≥2, with a significant increase in relative risk (RR) for ABS ≥3. According to Cox regression analysis, ABS 3 was associated with a 3,71-fold (95% CI 1,18-11,6; p=0,025) increase in the RR of adverse cardiovascular events after adjustment for sex, age, baseline CVR, obesity, smoking, diabetes, CAD, a history of myocardial revascularization, type 2 diabetes, drug therapy, and levels of non-high density lipoprotein cholesterol, highly sensitive C-reactive protein, and glomerular filtration rate.
Conclusion. In patients of various CVR aged 40-64 years, an ABS ≥3 was associated with a 3,71-fold (95% CI, 1,18-11,6; p=0,025) increase in relative risk of adverse cardiovascular events after adjusting for potential confounders, including sex, age, baseline CVR, CAD, and type 2 diabetes.
Aim. To compare the prevalence of coronary atherosclerosis in patients after coronary stenting (CS) receiving outpatient and remote cardiology follow-up during a one-year study.
Material and methods. We enrolled 279 patients aged 61,5±9,5 years with class ≥II stable angina or silent ischemia after CS. Three groups were formed: group 1 (n=96) — outpatient visits before CS, 1, 3, 6 and 12 months after CS. Group 2 (n=95) — remote monitoring: patients were followed up by a primary care physician with the involvement of a cardiologist via remote communication (e-mail, telephone, Skype) 1, 3, 6 and 12 months after CS. Group 3 (n=88) were followed up by a primary care physician and contacted with the study coordinator before and 12 months after CS. After 12 months, all patients underwent stress-induced myocardial ischemia testing. In case of a positive or uncertain test result, coronary angiography (CA) was performed.
Results. Stress-induced myocardial ischemia 12 months after CS was verified in 58 patients (21%): 19 patients (19,8%) — group 1; 9 patients (9,5%) — group 2; 30 patients (34,1%) — group 3 (p<0,05). Repeat CA was performed in 96 patients (34,4% of the total number of patients). Restenosis was detected in 8 (2,9%) patients, coronary atherosclerosis progression — in 38 (13,6%), combination of restenosis and atherosclerosis progression — in 4 (1,4%) patients. Coronary atherosclerosis progression was significantly more frequent in group 3: 10,4%, 9,5% and 21,6% in groups 1, 2 and 3, respectively (p<0,05). The incidence of stent restenosis was comparable: 2,1%, 3,2% and 3,5% in groups 1, 2, and 3, respectively.
Conclusion. Coronary atherosclerosis progression was the main reason for repeated revascularizations 12 months after the CS. Outpatient and remote cardiology follow-up is associated with a lower incidence of coronary atherosclerosis progression and repeated CA during 12-month follow-up after CS.
Aim. To assess the relationship between premature coronary artery disease (CAD) and various lipid parameters.
Material and methods. This retrospective longitudinal study included 166 men aged 57±9 years with coronary CAD with onset before age of 55. The control group consisted of 62 men (60±8 years old) who did not have CAD and peripheral arterial disease. In all patients, data on following lipid profile parameters were collected: total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), non-high-density lipoprotein cholesterol (non-HDL-C) and lipoprotein(a) (Lp(a)) at the time of CAD onset, while in control group patients — at the first visit to the A.L. Myasnikov Institute of Clinical Cardiology. These indicators were measured in blood plasma at the time of enrollment in all patients. In addition, the concentration of LDL-C corrected for Lp(a)-cholesterol (LDL-Ccorr) was calculated. Hypercholesterolemia was diagnosed with an initial level of TC >5 mmol/l, or LDL-C ≥3,0 mmol/l, or non-HDL-C ≥3,8 mmol/l, while hyperlipoproteinemia(a) (HLP(a)) — at the level of Lp(a) ≥30 mg/dl.
Results. Lipid metabolism disorders were significantly more common in patients with premature CAD compared to the control group. Lp(a) concentration ≥30 mg/dl, along with elevated levels of non-HDL-C or LDL-Ccorr, were associated with premature CAD, regardless of heredity and smoking, in the general cohort of examined men. Kaplan-Meier survival analysis showed that any type of lipid metabolism disorder was associated with an increased risk of premature CAD. In addition, patients with isolated elevated Lp(a) concentrations lived to the CAD onset 8 years earlier — 47 vs 55 years, p<0,02. The probability of premature CAD was maximum when the elevated level of non-HDL-C and HLP(a) was combined (hazard ratio, 2,91 (95% CI 1,96-4,33), p<0,0001).
Conclusion. HLP(a) is an independent factor of premature CAD, even with normolipidemia, which confirms the need for routine measurement of Lp(a) in clinical practice.
Aim. To study the oxidative and antioxidant blood profile in young people with premature coronary artery disease (CAD) and abdominal obesity (AO).
Material and methods. The study included 169 people. The main group consisted of 47 patients diagnosed with premature (<45 years of age) CAD, while 22 of them with AO and 25 without AO. The control group included 122 people without CAD, comparable with the main group in sex, age and body mass index. Among them, there are 67 people with AO and 55 people without AO. In all examined patients, the blood levels of total cholesterol, triglycerides, high-density lipoprotein cholesterol, MDA-modified oxidized high-density lipoprotein, superoxide dismutase (SOD), glutathione peroxidase 1, and whole blood total antioxidant capacity (TAC) were determined. Statistical processing was carried out in the SPSS 13.0 program.
Results. The blood TAC was 2,3 times lower in persons with CAD than in those without CAD, and amounted to 1,58 mmol of trolox. The blood level of SOD in patients with CAD was 1,16 times higher than in the group of people without CAD. The relative odds of premature CAD were associated with decreased TAC (B=-2,855; Exp(B)=0,058; 95% confidence interval (CI), 0,008-0,392; p=0,004) and increased level of SOD (B=0,105; Exp(B)=1,076; 95% CI, 1,031-1,196; p=0,006), regardless of sex, age, risk factors. Conclusion. Thus, an increased SOD and reduced TAC can be potential biomarkers for premature CAD in people under 45 years of age.
Aim. To analyze the relationship of blood lipid profile parameters, including the level of lipoprotein(a) (Lp(a)), and the content of circulating CD4+ T-lymphocytes with premature coronary artery disease (CAD).
Material and methods. This retrospective cross-sectional study included 76 men aged 40 to 79 years. Patients were divided into following groups: main group — patients with CAD (58 [54;64] years, n=56) onset before the age of 55; control group — patients (62 [57;66] years, n=20) without CAD and obstructive CAD and peripheral arterial disease. Statins were taken by 51 (91%) and 9 (45%) patients in the main and control groups, respectively. In serum and plasma samples, lipid spectrum parameters and Lp(a) concentration were determined. Cellular phenotyping was performed by direct immunofluorescence in a culture of mononuclear leukocytes isolated from blood. To determine cytokines, cells were in vitro activated with inhibitor of intracellular transport of secretory proteins. Cell fluorescence was determined using flow cytometry.
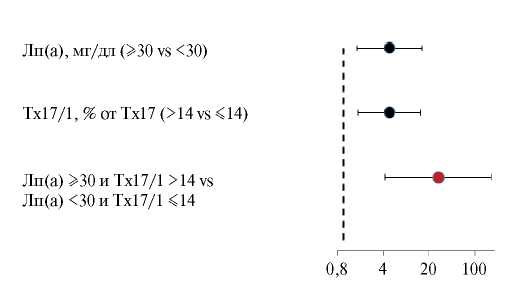
Results. Patients of both groups were comparable in age, body mass index, prevalence of hypertension and diabetes. Blood Lp(a) concentrations were higher in the CAD group than in the control group (49 [10;102] mg/dL vs 12 [4,3;32] mg/ dL, p<0,05). The content of INFγ-producing T-helpers 17 (Th17/1) was also higher in the CAD group (19 [15;24] vs 13 [11;22], % of Th17, p=0,05). Logistic regression revealed that elevated Lp(a) levels (≥30 mg/dL) and relative amounts of Th17/1 (>14% of Th17) independently of each other, atherogenic lipoprotein cholesterol levels, classical risk factors, and statin use were associated with premature CAD in the general group of patients with odds ratio (OR) of 4,6 (95% confidence interval (CI), 1,1-20,2) and 10,9 (2,1-56,7), p<0,05, respectively. The combination of Lp(a) >30 mg/dl and Th17/1 over 14% significantly increased the risk of premature CAD (OR, 28,0, 95% CI, 4,31-181,75, p=0,0005).
Conclusion. We have shown for the first time that an increased Lp(a) concentration with an increased Th17/1 content is associated with the premature CAD in men.
Aim. To assess the predictive potential of electrocardiographic (ECG), echocardiographic, and lipid parameters for predicting obstructive coronary artery disease (oCAD) in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS) prior to invasive coronary angiography (CA).
Material and methods. This prospective observational cohort study included 525 patients with NSTE-ACS with a median age of 62 years who underwent invasive coronary angiography. Two groups were distinguished, the first of which consisted of 351 (67%) patients with oCAD (stenosis 50%), and the second — 174 (33%) without oCAD (<50%). Clinical and functional status of patients before CAG was assessed by 40 indicators. Mann-Whitney, Fisher, chi-squared, univariate logistic regression (LR) methods were used for data processing and analysis, while miltivariate LR (MLR), gradient boosting (XGBoost) and artificial neural networks (ANN) were used to develop predictive models. The quality of the models was assessed using 4 following metrics: area under the ROC curve (AUC), sensitivity (Se), specificity (Sp), and accuracy (Ac).
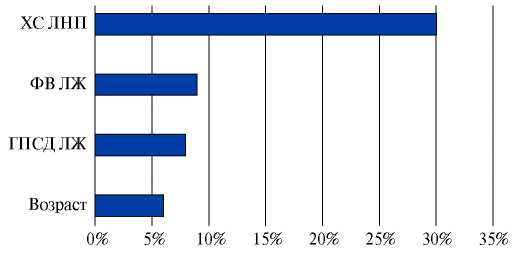
Results. A comprehensive analysis of ECG, echocardiography and lipid profile parameters made it possible to identify factors that had linear and non-linear association with oCAD. LR were used to determine their weight coefficients and threshold values with the highest predictive potential. The quality metrics of the best predictive algorithm based on MLR were 0,81 for AUC, 0,74 for Sp and Ac, and 0,75 for Se. The predictors of this model were 4 categorical parameters (left ventricular (LV) ejection fraction of 42-60%, global LV longitudinal systolic strain <19%, low-density lipoprotein cholesterol >3,5 mmol/l, age >55 years in men and >65 years for women).
Conclusion. The prognostic model developed on the basis of MLR made it possible to verify oCAD with high accuracy in patients with NSTE-ACS before invasive CA. Models based on XGBoost and ANN had less predictive value.
Aim. To assess the change in ergoreflex activity in heart failure patients with reduced left ventricular systolic function in the study of the effectiveness of physical training (PT) with original regimen, compared with PT with conventionally estimated regimen.
Material and methods. Single-center open-label study of 297 patients with class III HF. The patients were divided into two groups: main group (MG) — patients, in whom the PT intensity was estimated based on lactate threshold (LT); comparison group (CG), in whom the PT intensity was estimated based on 60% VO2peak. We analyzed ergoreflex activity, the relationship of ergoreflex with exercise tolerance (ET), routine systemic inflammation markers, clinical manifestations of HF, and ET based on VO2peak.
Results. An increase in gait velocity at the LT level after 3 months of PT was registered in 94% (n=210) of the MG patients. After 3 months, the PT regimen was recalculated according to 60% VO2реак; an increase in gait velocity at this level after 3 months of PT was registered in 70% of CG patients (n=35). The severity of HF decreased in both groups, but the dynamics was more pronounced in the MG, where class II was achieved by 75% of patients (in CG — 44%, p=0,003). In the MG, to a greater extent than in the CG, the ET increased. Ergoreflex activity (according to ΔVE) decreased by ≥15% in 230 (97%) MG patients and in 31 (63%) patients with CG. After the completion of the PT period, when in some patients the HF severity decreased to class II, we revealed a direct association of the ergoreflex value (according to ΔVE) with a greater severity of HF (r=-0,57, p=0,01) and the relationship between the decrease in ergoreflex activity (according to ΔVE), an increase in VO2LT (r=-0,55, p=0,001), VO2peak (r=0,49, p=0,001), a decrease in monocyte count (r=0,63, p=0,01).
Conclusion. In stable patients with class III HF receiving the proper disease-modifying therapy, ergoreflex activity is increased and is associated with functional class, ET, and systemic inflammation activity. In the course of physical rehabilitation, a decrease in ergoreflex activity is accompanied by a decrease in functional class, an increase in EF, which is more pronounced with personalized aerobic exercise using LT regimen assessment.
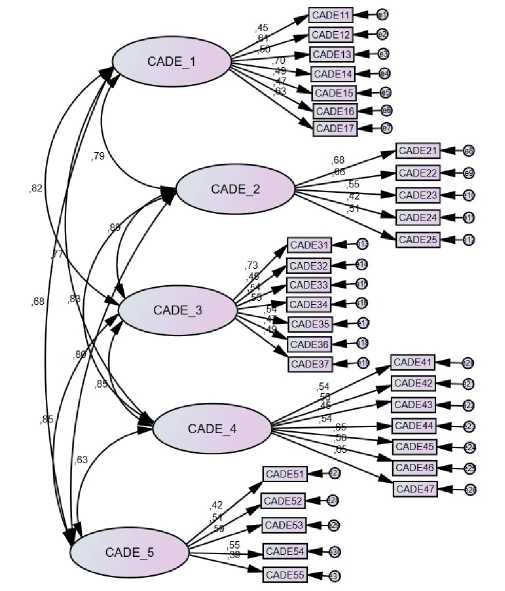
Aim. This study sought to translate, cross-culturally adapt, and psychometrically validate the Coronary Artery Disease Education Questionnaire II (CADE-Q II) in Russian.
Material and methods. Independent translations and back-translations of the CADE-Q II were conducted by bilingual health professionals and certified translators, respectively. Experts met to consider cultural relevance of the items to Russian patients. The finalized version was then pilot tested in a group of patients to assess understanding and time to complete the tool. Following these steps, 303 patients with a diagnosis of stable coronary artery disease treated in the Outpatient Cardiology Department between April and November 2021 completed the CADE-Q II. The following psychometric properties were evaluated: confirmatory factor analysis, internal consistency (assessed by Cronbach's alpha), test-retest reliability (ICC), and criterion validity (assessed through the association with CADE-Q II and The Self Care of Coronary Heart Disease Inventory and SF-36 scores, among other characteristics from the participants including educational level).
Results. After items were translated, revised, culturally adapted and finalized, 30 patients took 30 minutes to complete the CADE-Q II during pilot test and questionnaire was considered understandable by all. Factor analysis (Kaiser-Meyer-Olkin =0.692 and Bartlett's criterion of Sphericity <0.05) revealed four factors, all internally consistent and aligned with the original version of the questionnaire. Cronbach's alpha of subscales ranged from 0.61 to 0.88 and ICC was 0.81. Criterion validity was confirmed by significant differences in total CADE-Q II scores by participants' educational level and correlations between CADE-Q II and The Self Care of Coronary Heart Disease Inventory scores (r=0.251, p<0.05).
Conclusion. The Russian CADE-Q II presented sufficient validity and reliability for use to assess disease-related knowledge of chronic coronary syndrome patients in Russia.
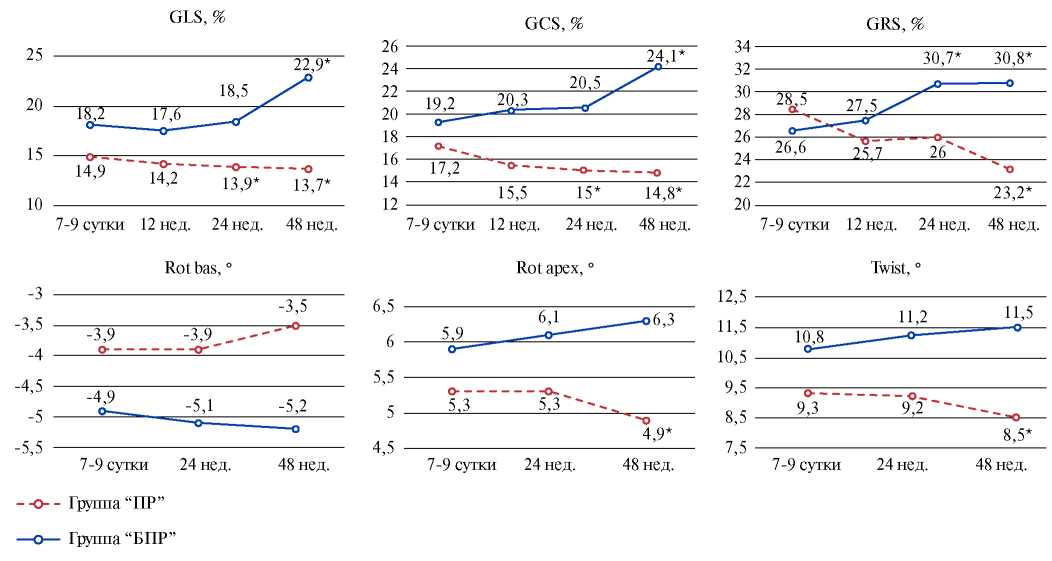
Aim. To assess early predictors of pathological remodeling in patients after ST-elevation myocardial infarction (STEMI) using speckle-tracking echocardiography (STE).
Material and methods. The study included 114 STEMI patients aged 52 (44; 58) years. A two-dimensional echocardiography was performed with the analysis of standard parameters and STE with an analysis of strain and rotational characteristics of the myocardium. In addition, brain natriuretic peptide and troponin-I concentration was determined. The development of pathological post-infarction remodeling within 12-month follow-up was assessed as an end point. Depending on the outcome, 2 groups were formed: group 1 — patients with pathological remodeling (PR), n=45 (39,5%), group 2 — patients without PR, n=69 (60,5%).
Results. Early remodeling was detected in 24 (53,3%) people, mid-term — in 15 (33,4%), and late remodeling — in 6 (13,3%). In the PR group, heart failure (HF) was detected in 100% of patients, while in non-PR group, 23 (33,3%) patients had no signs of HF.
In the early period of myocardial infarction, each of following indicators with high sensitivity and specificity predicts postinfarction pathological dilatation: global longitudinal strain (GLS) <11,7%, global circular strain (GCS) <12,4%, and a Twist decrease to 7,8o. A multivariate logistic regression model was created for the formation of pathological remodeling in patients with STEMI, which included GLS, global radial deformation (GRS), end-systolic volume index (ESVI), determined on days 7-9 of STEMI.
Conclusion. GLS, GCS, and left ventricular Twist are independent highly sensitive and specific predictors of pathological remodeling. The following early predictors of postinfarction pathological dilatation have been established: reduced GLS in combination with higher GRS and left ventricular ESVI.
LITERATURE REVIEW
Modern imaging techniques occupy an important place in the diagnosis, selection of treatment and prognosis of patients with coronary artery disease. Hybrid imaging is a combination of two sets of diagnostic data that complement and enhance each other by comparing anatomical and functional characteristics. As a rule, hybrid imaging is synergistic, that is, more powerful, since the addition of new information leads to an increase in the sensitivity and specificity of each of the modalities separately.
The review provides brief information on the diagnostic efficacy of myocardial perfusion scintigraphy (MPS), computerized tomography (CT) coronary angiography in comparison with invasive coronary angiography with fractional flow reserve. The diagnostic and prognostic significance of assessing calcium index with MPS, as well as CT coronary angiography combined with MPS in the diagnosis, risk stratification and prognosis of patients with coronary artery disease, is characterized in detail. A separate section is devoted to the importance of hybrid imaging in making decisions about myocardial revascularization.
INFORMATION
ISSN 2618-7620 (Online)