ARTERIAL HYPERTENSION
- The implementation of 2024 Russian guidelines on hypertension in adults in is associated with trends towards increasing the coverage of the population with antihypertensive therapy.
- A shift towards triple therapy, including single-pill combinations, was revealed.
- Interaction between physician and patient in the form of discussion of the need to comply with recommendations is an important factor associated with improved treatment adherence and effectiveness.
Aim. To evaluate the features of antihypertensive therapy (AHT), adherence to therapy and achievement of target blood pressure (BP) in patients with hypertension (HTN) in Russian real-world practice after the implementation of 2024 Russian clinical guidelines on hypertension in adults.
Material and methods. During May 2025, 7990 patients with HTN from 19 Russian cities and Tiraspol (Pridnestrovian Moldavian Republic) took part in the BP measurement campaign. Outpatients with HTN over the age of 18 voluntarily participated in the campaign. During the screening, BP and pulse were measured three times using an automatic or mechanical BP monitor. In addition, a questionnaire was filled out on behavioral risk factors, BP self-monitoring skills, medication adherence, AHT, comorbidities and related therapy. The effectiveness of AHT was understood as achieving the target BP level <140/90 mm Hg in patients with HTN and taking AHT, and BP control — in all hypertensive patients, regardless of taking AHT.
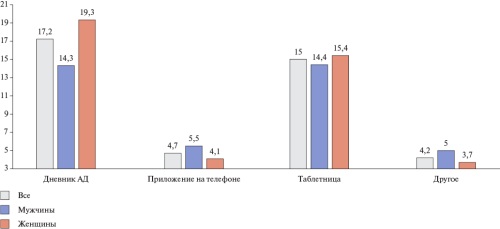
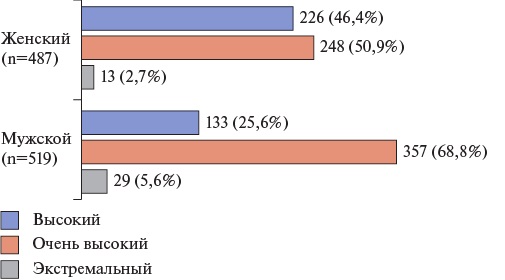
Results. The analysis included 7972 respondents aged 18 to 96 years (median age 62 years [51;71]), including 3372 men (42,3%). Among the participants, 74,4% took AHT, while 62,6% achieved target BP <140/90 mm Hg and 25,8% — target BP <130/80 mm Hg. On-demand therapy remains the leading reason for not taking AHT among patients with HTN. Approximately half of the participants (57,7%) answered that they do not use medication reminder systems. Most often, hypertensive patients use BP self-monitoring diaries and pill boxes. Every fifth patient with HTN was registered as taking antihypertensive monotherapy, every third as dual AHT, and every fourth as triple AHT. Single-pill combinations were taken by 34,5% of patients. In outpatient practice, following sex differences were revealed: significantly higher prevalence of taking AHT, using AHT reminder systems, discussions with a doctor, and the effectiveness of treatment and control of HTN were characteristic of female patients. Discussion with a doctor about the importance of following recommendations was associated with a significantly higher achievement of target BP level (odds ratio (OR) 1,43), the use of a single-pill AHT combination (OR 1,3) and statin therapy (OR 1,39), p<0,0001.
Conclusion. In outpatient practice after the implementation of 2024 Russian clinical guidelines for HTN, an increase in the coverage and efficacy of AHT, and the HTN control is observed compared to the population data of 2020-2022. AHT prescription profile indicates a decrease in the share of monotherapy and an increase in the share of triple combination. The use of single-pill antihypertensive combinations is growing, but remains insufficient. The results obtained demonstrate the importance of discussing with a physician the need to comply with recommendations in hypertensive patients to improve adherence and treatment effectiveness.
- This article presents the results of a large-scale physician survey on perceptions of adherence to antihypertensive therapy.
- Despite recognizing its importance, most physicians spend no more than 10 minutes discussing therapy with patients.
- Physicians predominantly use indirect and mostly non-validated methods to assess adherence.
- Key strategies to improve adherence include patient education, treatment simplification, and use of reminders.
- Major barriers include lack of time, limited resources, and restricted access to objective assessment tools.
Aim. To survey Russian medical professionals on compliance issues, since high adherence to antihypertensive therapy (AHT) is one of the main conditions for satisfactory control of hypertension (HTN) and reduction of cardiovascular risk. A physician plays a key role in increasing adherence, but in Russia there is insufficient data on how specialists perceive and solve the problem of low compliance.
Material and methods. Between March 4 and June 1, 2025, an anonymous online survey was conducted via the website of the Russian Society of Cardiology. The questionnaire included 11 items in different formats and was completed on a voluntary basis.
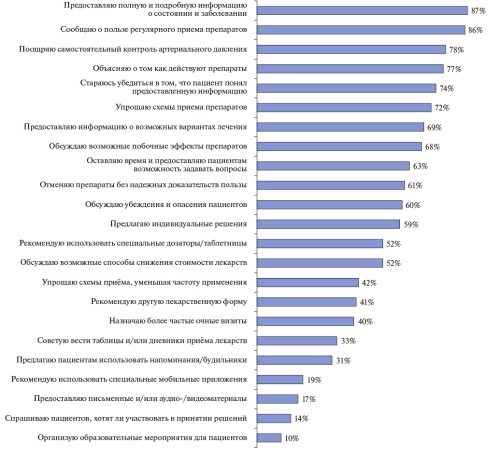
Results. A total of 344 physicians participated, mostly women (78%), cardiologists (83%), with over 10 years of experience (74%), and involved in outpatient care (86%). The average time spent discussing AHT with patients was 1-5 minutes (28%) or 6-10 minutes (38%). Most respondents (73%) believed that only 0-15% of their patients with HTN never initiate the recommended therapy, and 33% estimated that more than half continue treatment one year after initiation. A total of 41,5% of physicians agreed that nonadherence is usually a conscious decision, while most considered adherence improvement possible but doubted the existence of a universal strategy (62,2%). Unstructured patient interviews were the most common method for assessing adherence, while fewer than 25% used direct methods. Physicians primarily rely on patient education and treatment simplification to improve adherence. Shared decision-making and educational programs were less frequently used. Major barriers identified included high workload, limited consultation time, and lack of systemic support.
Conclusion. Surveyed physicians perceive low adherence in patients with HTN as a complex and multifaceted construct, but are optimistic about the potential for its improvement. The current level of implementation of modern methods for assessing and improving adherence remains low, partly due to high workload. There is a need to develop simple, easy-to-implement algorithms for identifying and addressing nonadherence, as well as to optimize the organizational conditions of outpatient care in order to provide effective support for patients with HTN.
ОБЩЕСТВЕННОЕ ЗДОРОВЬЕ И ОРГАНИЗАЦИЯ ЗДРАВООХРАНЕНИЯ
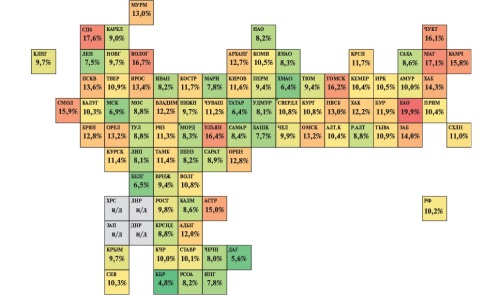
Myocardial infarction (MI) continues to retain the status of one of the key lifethreatening cardiovascular diseases with a high morbidity and mortality, including the working-age population. As part of the federal project "Control of Cardiovascular Diseases" in the Russian Federation in 2019-2024, a large-scale modernization of healthcare system for acute coronary syndrome and MI was carried out. The network of regional vascular centers was expanded and patient routing was optimized, which made it possible to increase the coverage of percutaneous coronary intervention for ST-segment elevation MI from 56% to 77%, and for NSTEMI — from 21% to 48%, and to achieve a decrease in mortality from MI per 100 thousand people by 19,6%, and inhospital mortality from MI — by 32%. However, interregional differences remain, and therefore further work is needed to improve the availability and timing of reperfusion therapy. Within the federal project "Control of Cardiovascular Diseases" of the National Project "Long and Active Life", the target indicator of reperfusion therapy coverage of patients with MI hospitalized within the first 24 hours from the disease onset will be monitored. Its level should reach 95% by 2030. Implementation of additional measures will reduce the differentiation of indicators between regions, reduce cardiovascular mortality and achieve national goals to increase life expectancy.
- Analysis of healthcare availability in acute coronary syndrome in the Kursk and Kurgan regions revealed features of the influence of various availability factors in reducing mortality.
- In the Kursk Oblast, the main contribution to reducing mortality is made by systemic thrombolytic therapy, while in the Kurgan Oblast — by reducing the duration of hospitalization.
- To improve efficiency, it is recommended to take into account time aspects in target indicators, revise the definition of specialized hospitalization and strengthen control over monitoring data.
- Digital systems, such as Cardionet, should be implemented to optimize patient routing and monitoring of indicators.
Aim. To study regional features of the impact of the availability of emergency and specialized, including high-tech, healthcare for patients with acute coronary syndrome (ACS) on mortality using the example of the Kursk and Kurgan Regions.
Material and methods. Data from the "Monitoring of Measures to Reduce Mortality from Coronary Artery Disease" for 2016-2021 were used. Cointegration of time series characterizing mortality from ACS and parameters of health care availability was used. The elasticity coefficient was used to assess the strength of factors’ influence.
Results. In Kursk Oblast, mortality in ST-segment elevation ACS (STE-ACS) was reduced by the proportion of those hospitalized in the first 12 hours (E=0,93%; R2=0,80) and in the first 2 hours (E=0,86%; R2=0,87), as well as thrombolysis (E=4,9%; R2=0,98) and percutaneous coronary interventions (PCI) in patients admitted before 12 hours (E=0,65%; R2=0,94). Mortality in non-STE-ACS (NSTE-ACS) was reduced by increasing the proportion of PCI procedures (E=0,43%; R2=0,60). In the Kurgan Oblast, mortality in STE-ACS was reduced by the proportion of those hospitalized in the first 12 hours (E=1,9%; R2=0,76) and in the first 2 hours (E=0,65%; R2=0,65), as well as prehospital thrombolysis (E=0,44%; R2=0,56) and thrombolysis in general (E=1,15%; R2=0,96). In NSTE-ACS, mortality was also reduced by the proportion of PCI (E=1,1%; R2=0,75).
Conclusion. The study demonstrates regional differences in the impact of the availability of emergency and specialized, including high-tech, healthcare for patients with ACS. In the Kursk Oblast, systemic thrombolysis plays a key role in reducing mortality, while in the Kurgan Oblast, it is a reduction in hospitalization time. In both regions, to reduce mortality in NSTE-ACS, the availability of PCI should be increased. Thus, cointegration analysis should be used to assess the effectiveness of regional healthcare systems.
ACUTE AND CHRONIC HEART FAILURE. ORIGINAL ARTICLES
- Diagnosis of heart failure with preserved ejection fraction is a complex task.
- Analysis of left atrial reservoir function during resting echocardiography in combination with additional signs of diastolic reserve decrease according to diastolic stress test constitute a multifactorial/complex approach to the diagnosis of heart failure with preserved ejection fraction.
Aim. To study the heart structural and functional state in confirmed heart failure with preserved ejection fraction (HFpEF) depending on the severity of left ventricle (LV) diastolic dysfunction.
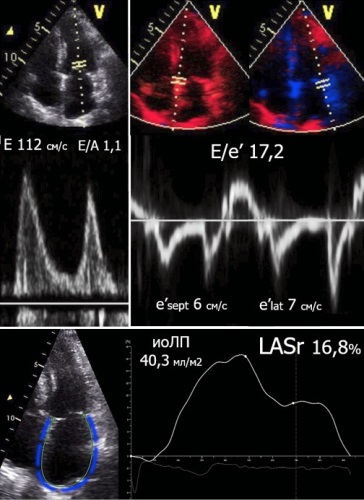
Material and methods. Data from 303 patients with LV diastolic dysfunction (men 45,2%, mean age 66,3±6,0 years) were analyzed. The diastolic stress test (DST) was performed when the criteria for HFpEF according to resting echocardiography data was insufficient (n=251). The study included 153 patients with confirmed HFpEF (men 35,3%, mean age 67,0±5,6 years). Group I (n=101) included patients with decreased LV diastolic reserve in DST (E/e’ >14), while group II (n=52) — patients with significant LV diastolic dysfunction at rest who do not require DST to verify HFpEF. The speckle-tracking echocardiography was used to assess left atrial reservoir strain (LASr).
Results. Significant differences were found in the 6-min walk test (400,0 [360,0;440,0] m in group I vs 365,5 [310,5;401,5] m in group II, respectively; p<0,001) and N-terminal pro-brain natriuretic peptide (NT-proBNP) level (257,7 [100,0;443,3] pg/ml and 412,0 [191,4;780,2] pg/ml; p=0,002). Resting echocardiography revealed significant differences in the left atrium (LA) volume index (VI) (33,5 [29,2;40,1] ml/m2 vs 40,8 [37,3; 47,6] ml/m2; p<0,001), E/e’ ratio (11,3 [10,1;12,6] and 16,3 [14,9;19,2]; p<0,001), LASr (21,3 [19,5;24,7]% and 15,0 [12,5;17,3]%; p<0,001). Following moderate correlations were found in patients with HFpEF: LASr and E/e’ (r=-0,538; p<0,001), LASr and LAVI (r=-0,443; p<0,001). There was no correlation between LASr and NT-proBNP (r=-0,157; p=0,060). When analyzing the DST, significant differences were found in all characteristics in group I.
Conclusion. Patients with confirmed HFpEF with an increase in LV filling pressure are characterized by LA reservoir dysfunction and LA dilation. Phase analysis of LA strain and DST allows for timely diagnosis of HFpEF.
- Heart failure (HF) is a risk factor for pulmonary embolism (PE).
- HF is associated with complicated PE.
- Inhospital mortality among patients included in the SIRENA registry is significantly higher in the group of patients with PE and HF.
Aim. To study the effect of heart failure (HF) on the course of pulmonary embolism (PE) according to the Russian registry SIRENA.
Material and methods. The study was conducted based on the data of an observational prospective registry SIRENA. The registry included all consecutively hospitalized patients with PE diagnosed by any available means. The enrollment duration was 12 months. The hospital period of patient management was assessed. Information on the included patients was provided by 20 hospitals from 15 Russian cities.
Results. The present study included 495 patients with PE. HF was diagnosed in 38,6% of cases (n=191). Patients with a combination of PE and HF were characterized by a significantly higher prevalence of coronary artery disease (32,5%), hypertension (83,2%), atrial fibrillation (48,7%), diabetes (42,4%), prior cerebrovascular accident (17,3%), and stage 3 chronic kidney disease (49,7%). Physical examination of patients with PE and HF revealed reliable differences in lower limb edema (p=0,001), jugular vein distention (p=0,043), moist rales in lower lungs (p=0,001), tachypnea (p=0,001), cyanosis (p=0,001). In addition, patients with PE and HF were characterized by a lower level of saturation (p=0,001), systolic (p=0,006) and diastolic (p=0,005) blood pressure. When analyzing ECG data, the only significant difference in the compared groups was ST segment depression in the group of patients with PE and HF (22,5% versus 9,9%, p=0,036). According to echocardiography, pulmonary hypertension (p=0,041), right ventricular (p=0,048) and right atrial (p=0,023) dilation were more often detected in patients with PE and HF. The prevalence of acute heart failure, as one of the complications of PE, prevailed in the group of patients with PE and HF (p=0,023). Inhospital mortality in patients with PE and HF reached 15,2% and significantly differed from that in the PE group without HF — 4,6% (p=0,047).
Conclusion. HF in patients with PE is associated with a high level of comorbidity of patients complicated by the course of PE and, as a consequence, an increase in mortality. It is necessary to be wary of possible PE in patients with manifestations of decompensated HF.
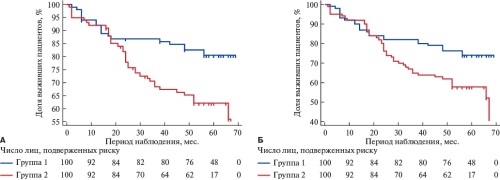
- Long-term prognosis in patients with implanted cardiac contractility modulation devices with heart failure (HF) and atrial fibrillation (AF) was analyzed.
- Cardiac contractility modulation in patients with HF with reduced ejection fraction and AF was studied.
- Cardiac contractility modulation significantly improves the long-term 5-year prognosis in patients with HF and AF.
Aim. To assess the effect of cardiac contractility modulation (CCM) in patients with heart failure with reduced ejection fraction (HFrEF) and atrial fibrillation (AF) on 5-year survival.
Material and methods. Two hundred patients with HFrEF and AF were included. Patients were consecutively included in two following groups: group 1 — patients with heart failure (HF) receiving optimal therapy in combination with implanted CCM devices (n=100); group 2 — comparison group — patients with HF receiving only optimal therapy (n=100). The mean follow-up period was 40,5±20,4 months. Cardiovascular death (CVD) was considered as the primary endpoint, and all-cause death was taken as the secondary endpoint.
Results. In the CCM group, a total of 24 deaths (24%) were registered during longterm follow-up, while in the optimal therapy group — 46 (46%). Primary endpoint rate (CVD after 5-year follow-up) was significantly higher in the optimal therapy group compared to CCM group and amounted to 38% and 19%, respectively (logrank test <0,003). In the CCM group, the secondary endpoint (all-cause death) was achieved in 26% (n=26), in the optimal therapy group — in 44%. Logrank showed significant survival differences (p=0,008). In cardiovascular mortality structure, two main causes should be highlighted — sudden cardiac death (SCD) and death due to decompensated HF. In the CCM group, SCD as a cause of CVD (n=6, 23%) was significantly less than in the optimal therapy group (n=16, 36%), p=0,039, while mortality for decompensated HF did not reach a significant difference (CCM: n=8, 30%, optimal therapy: n=17, 39%, p=0,085). CCM therapy has a significant effect on reducing the risk of both all-cause (relative risk=0,591, 95% confidence interval: 0,397-0,879, p=0,009) and cardiovascular death (relative risk=0,474, 95% confidence interval: 0,290-0,771, p=0,003) in long-term follow-up.
Conclusion. CCM significantly improves the long-term 5-year prognosis in patients with HF and AF.
ОЦЕНКА РИСКА
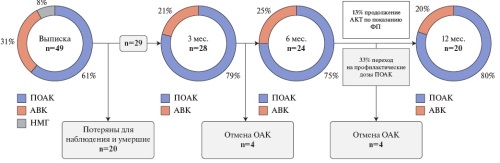
- Pulmonary embolism (PE) can lead to long-term adverse effects and be associated with long-term disability of patients.
- This study summarizes the data of inpatient and outpatient stages of management of PE patients.
- The obtained results show that patients are insufficiently committed after discharge and highlight the need to implement an algorithm for outpatient management of patients after PE, which will allow for timely detection of complications and clarification of anticoagulation duration.
Aim. To study the results of long-term follow-up of patients with pulmonary embolism (PE) of intermediate and high 30-day mortality risk.
Material and methods. This retrospective study included 53 patients (45,3% men) with intermediateand high-risk PE, hospitalized at the Almazov National Medical Research Center from 2019 to 2020. The mean follow-up period was 20,9 [4,0; 33,5] months. The data were obtained from the health information system, as well as through phone calls.
Results. Seven patients (13,2%) were classified as high, 29 (54,7%) as intermediate-high, and 17 (32,1%) as intermediate-low risk for 30-day mortality. Systemic thrombolytic therapy was performed in 11,3%, and selective transcatheter thrombolysis was performed in 24,5%. Of the 33 patients with available data, 23 (69,7%) attended in-person outpatient appointments. Another 10 (30,3%) patients were interviewed by telephone. Cancer screening was recommended to 36 (73,5%) patients, but the recommendation was followed only in a quarter of cases and papillary thyroid cancer was detected in one patient. Examination for thrombophilia was recommended for 20 (40,8%) patients, while 12 (60,0%) patients underwent it, 5 (41,6%) of whom were found to have hereditary thrombophilia. After discharge, 15 (30,6%) patients underwent control echocardiography, and 8 (16,3%) patients underwent repeat computed tomography pulmonary angiography. Chronic thromboembolic pulmonary disease was diagnosed in two cases, and chronic thromboembolic pulmonary hypertension was confirmed in one patient. Upon discharge, 30 (61,2%) patients were prescribed direct oral anticoagulants, 15 (30,5%) — vitamin K antagonists, 4 (8,2%) — low molecular weight heparin. The median duration of anticoagulant therapy was 22 [7,5; 31,5] months, with 20 (69,0%) patients receiving anticoagulants for >12 months. Outpatient bleeding was observed in 4 (13,8%) patients, all of which were recognized minor according to the International Society on Thrombosis and Haemostasis (ISTH) classification. No recurrence of deep vein thrombosis and/or PE was observed. After discharge, 3 (6,1%) deaths were recorded, the causes of which were unknown. One-year survival rate was 88%.
Conclusion. There is insufficient patient compliance with discharge recommendations and low continuity of inpatient and outpatient treatment of patients with PE. Further implementation of the algorithm for outpatient management of patients after PE is required, which will allow making decisions on anticoagulant therapy and effectively and timely identifying PE consequences.
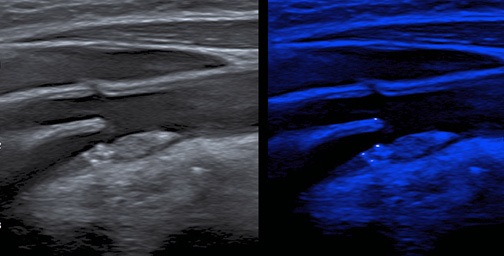
- Novel MicroPure ultrasound technology was used for the first time to detect microcalcifications in the carotid plaque in patients with acute coronary syndrome and stable coronary artery disease.
- In patients with acute coronary syndrome, carotid plaque microcalcifications are more common than in patients with coronary artery disease.
- Detection of microcalcifications using ultrasound may be an important sign of plaque instability.
Aim. To evaluate the potential of the MicroPure ultrasound technology for detecting microcalcification in carotid plaques in patients with acute coronary syndrome (ACS).
Material and methods. The study included 50 patients with cardiovascular diseases (65,62±11,12 years, 34 men), including 25 patients with ACS (64,0±11,5 years, 19 men) and 25 patients with chronic coronary artery disease (CAD) (67,2±10,7 years; 15 men). The patients underwent standard clinical and laboratory examination, as well as carotid ultrasound using a Canon Aplio a550 system (Japan) of 14,0 MHz. Scanning of the detected plaques was performed in B-mode and MicroPure mode for microcalcification analysis. Plaque microcalcification as such, the number (single or multiple) and location (cap, body, base, combined location) of microcalcifications in plaques were assessed.
Results. Plaque microcalcification was detected in all patients with ACS, whereas in the group of patients with CAD they were detected twice as rarely (100% vs 48%, p=0,0001). Microcalcifications were more often detected in the plaque cap and body in patients with ACS than in patients with CAD (43% vs 23%, p=0,0125 and 55,4% vs 14,6%, p<0,001, respectively). In both groups, both single and multiple microcalcifications were detected as follows: 26,3% and 73,7% in the ACS group and 28,12% and 71,8% in the CAD group, respectively (p>0,05).
Conclusion. Significant predominance of carotid plaque microcalcifications was detected in patients with ACS compared to patients with CAD. Detection of microcalcifications using novel ultrasound technologies may be an important sign of atherosclerotic plaque instability.
CLINIC AND PHARMACOTHERAPY
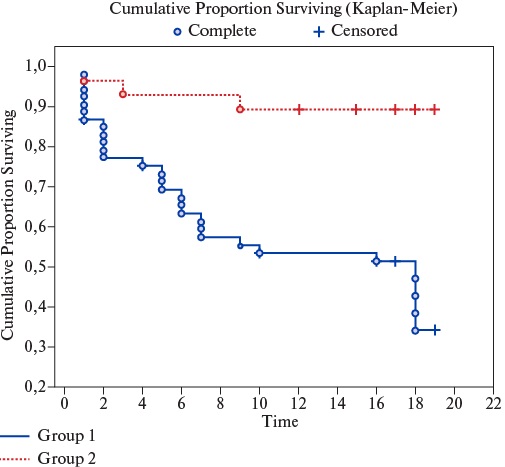
- Ineffective lipid-lowering therapy is a significant predictor of adverse outcomes in patients after acute coronary syndrome (ACS).
- The lipid center has the potential to be a basic institution for lipid-lowering therapy after ACS.
- Lipid-lowering therapy in the lipid center was characterized by earlier and more frequent use of combination therapy, including with PCSK9 inhibitors, and a high compliance with current clinical guidelines.
Aim. To evaluate the effectiveness of lipid-lowering therapy (LLT) administered in the lipid center to patients with acute coronary syndrome (ACS) and severe dyslipidemia, and to study its impact on prognosis.
Material and methods. Over 18 months, 81 patients after ACS with low-density lipoprotein cholesterol (LDL-C) >3,9 mmol/L during hospitalization were followed up. Upon discharge, all were proposed for LLT at the lipid center; 53 (Group 1) refused and 28 (Group 2) agreed. At control visits after 3, 6, and 12 months, LDL-C and LLT characteristics were assessed in both groups. After 18 months, adverse outcomes (death, rehospitalizations) were assessed.
Results. LLT in lipid center was characterized by earlier and more frequent use of combination therapy. PCSK9-targeted therapy in case of failure to achieve LLT targets by other means was initiated in lipid center 3,6 times more often (p=0,00001) and 2,2 times faster (p=0,003) than in routine outpatient practice. At the visit 3 months after ACS, the target LDL-C level was met by 14,7% of patients in the 1st group and 25% of patients in the 2nd group (p=0,24), while 6 months after ACS — 18,4% and 63% of patients (p=0,005), and after a year — 20% and 85,7% of participants, respectively (p=0,00001). The rationale of using lipid center as a basic institution for LLT was confirmed by an improved prognosis according to a 18-month followup (especially with regard to rehospitalizations, which occurred 5,8 times less frequently than in outpatient practice, p=0,00001). The time before the start of PCSK9 inhibitors directly correlated with the need for rehospitalizations during further follow-up (R=0,46; p=0,007). In the first 12-month therapy, the hypolipidemic effect of inclisiran and monoclonal antibodies (alirocumab, evolocumab) in patients after ACS was comparable.
Conclusion. Lipid center is one of the divisions of medical facilities that have great potential for qualified support of LLT in patients with ACS and severe dyslipidemia. On its basis, a high compliance of medical measures with current clinical guidelines can be ensured.
- A multicenter study was conducted in the North Caucasus Federal District to assess the lipid profile changes in patients with high, very high and extreme cardiovascular risk in clinical practice.
- Systematic monitoring allowed increasing the proportion of patients receiving lipid-lowering therapy from 69,2% to 98,8%.
- Target values of low-density lipoprotein cholesterol were achieved in only 8,9% of patients, which emphasizes the need for earlier initiation of combination therapy, including PCSK9-targeted therapy, a personalized approach, and the introduction of modern guidelines in primary care practice.
Aim. To assess lipid metabolism parameters, their changes with lipid-lowering therapy and the achievement rate of low-density lipoprotein cholesterol (LDL-C) target levels in patients with high, very high and extreme cardiovascular risk who are outpatiently monitored in real-world practice.
Material and methods. A multicenter retrospective-prospective observational study was conducted in health facilities of the North Caucasus Federal District. The study included 1006 patients over 18 years of age with high (n=357), very high (n=601) and extreme (n=42) cardiovascular risk. Electronic individual registration cards were used, including demographic and clinical characteristics, lipid profile dynamics, treatment regimens and tolerability. Lipid parameters were monitored at least twice with an interval of 8±4 weeks. Descriptive and comparative statistics methods were used using SPSS Statistics 25 and R. Differences were considered significant at p<0,05.
Results. At the time of inclusion in the study, 84% of patients had dyslipidemia, but only 69,2% received lipid-lowering therapy. After inclusion, the proportion of those receiving treatment increased to 98,8%. MLDL-C level decreased from 3,7 to 2,7 mmol/l, and total cholesterol — from 5,7 to 4,8 mmol/l. Target LDL-C values were achieved in 8,9% of patients. The most pronounced reduction was observed in very high-risk patients and with the use of combination therapy (statins + ezetimibe). High individual variability in treatment response was established. In some cases, a paradoxical increase in LDL-C levels was recorded, requiring further analysis.
Conclusion. Systemic monitoring and treatment of lipid-lowering therapy allows achieving a significant reduction in atherogenic lipids, especially in the very high-risk group. However, achieving target LDL-C levels remains difficult. Early and broader initiation of combination therapy, regular assessment of adherence and personalized approach are necessary, especially in extreme-risk patients. The data obtained emphasize the importance of implementing modern clinical guidelines in primary health care practice.
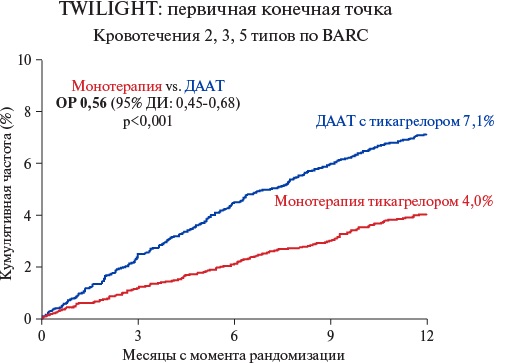
- Dual antiplatelet therapy (DAPT) after myocardial infarction significantly prevents thrombotic events, primarily recurrent myocardial infarction.
- There is convincing evidence that switching from DAPT to ticagrelor mototherapy 1-3 months after the event leads to a significant reduction in the bleeding risk without increasing the incidence of thrombotic events compared to 12-month DAPT.
It is known that the risk of thrombotic events in patients with acute coronary syndrome (ACS) is highest in the first year after the event. Regardless of the treatment tactics, dual antiplatelet therapy (DAPT) is prescribed for a year after. DAPT significantly prevents thrombotic events, primarily recurrent myocardial infarction. At the same time, the bleeding risk naturally increases. In recent years, convincing data have been obtained that the transition from DAPT to ticagrelor monotherapy 1-3 months after the event leads to a significant reduction in the bleeding risk without increasing the rate of thrombotic events compared to 12-month DAPT. The review analyzes data from randomized clinical trials comparing DAPT and ticagrelor monotherapy in patients with ACS and presents the provisions of Russian and international clinical guidelines for the treatment of ACS regarding ticagrelor monotherapy. The review aim is to rationale the advantage of ticagrelor monotherapy compared to standard DAPT in patients with ACS and percutaneous coronary intervention using a detailed analysis of randomized controlled trials and meta-analyses. The practical part presents the relevant sections of the clinical guidelines.
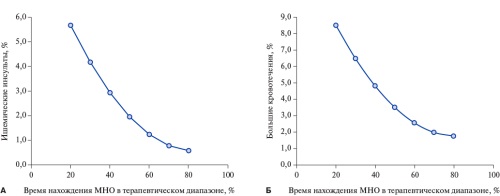
EXPERT CONSENSUS
The leading problem in the use of vitamin K antagonist (VKA) therapy is the complexity and the need to maintain the international normalized ratio (INR) within therapeutic window of at least 60% of the treatment time. Obviously, the optimal solution to this problem in the context of modern technological capabilities is its self-monitoring by a patient and understanding the need to adjust the VKA (warfarin) dose to achieve the target INR values (independently or with the help of a physician’s consultation). Portable devices and a model of self-monitoring of anticoagulant therapy (coagulometers) has reduced the rates of thromboembolism, major bleeding, and all-cause mortality, and confirmed its high cost-effectiveness.
An important aspect for successful INR self-monitoring is comprehensive patient education, implemented within the specialized schools. Such educational programs provide patients with the necessary knowledge about warfarin, the importance of regular INR monitoring, the aspects of self-monitoring, possible complications and actions in emergency situations. The combination of structured training and subsequent INR self-monitoring contributes to a significant increase in therapy adherence and improved clinical outcomes. The results of systematic reviews and randomized trials confirm that patient participation in educational programs reduces the risk of thromboembolic and hemorrhagic events and increases the overall effectiveness of treatment. The aim of the work was to formulate the key aspects of managing an education school for patients taking VKA.
The combination of educational programs, active follow-up, coagulometers, and remote monitoring forms a holistic model for managing patients receiving VKA that meets modern requirements for clinical efficacy, safety, and cost-effectiveness.
ISSN 2618-7620 (Online)