CLINICAL CASES
- Ogden syndrome is a very rare disease, previously undescribed in Russia, which is associated with NAA10gene pathology and is characterized by a combination of psychoneurological and skeletal disorders and various cardiovascular changes, including congenital heart defects, cardiomyopathy, and arrhythmias.
- In some cases, Ogden syndrome may be combined with long QT syndrome and cardiac arrest.
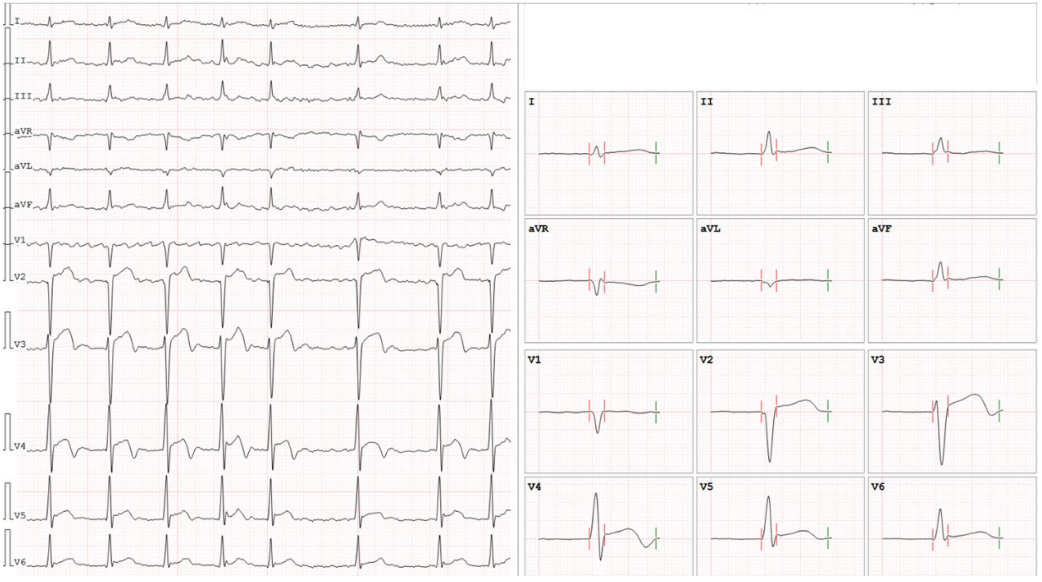
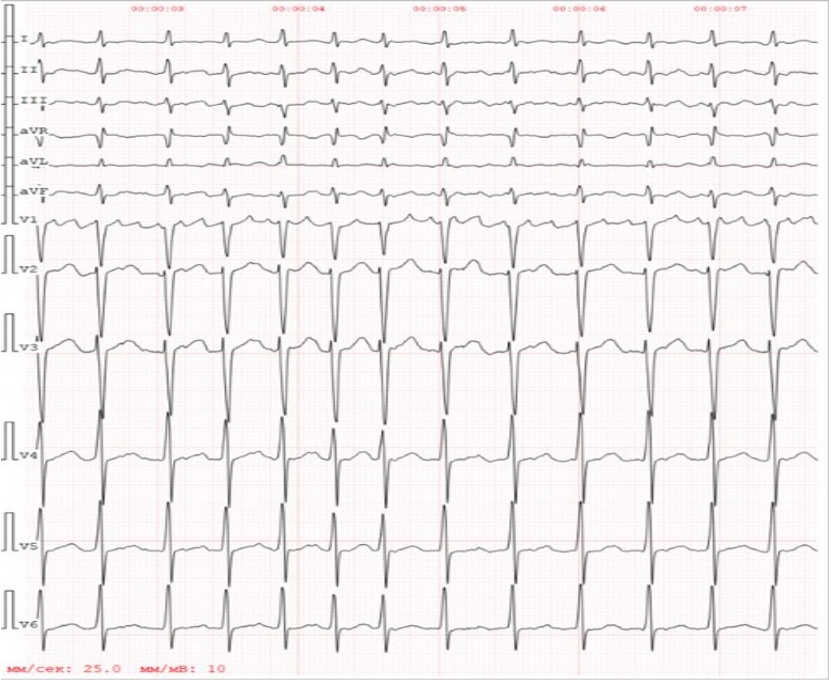
Introduction. The article presents a case of a child with long QT syndrome, skeletal and facial abnormalities, and mental deficiency. This symptom complex was a manifestation of an Ogden syndrome, previously undescribed in Russia X-linked disease associated with a NAA10 gene mutation.
Brief description. Molecular genetic testing confirmed a mutation (p.Tyr43Ser) in this gene, which was also found in the child’s sister and mother. During anesthesia, the boy suffered cardiac arrest due to severe bradycardia and asystole, due to which a cardioverter-defibrillator was implanted.
Discussion. Ogden syndrome is a disease associated with NAA10 gene mutations, which may remain unrecognized. Severe psychoneurological symptoms can mask the cardiac manifestations of the disease for a long time, including long QT syndrome and arrhythmias, which can manifest as dangerous life-threatening arrhythmias and sudden death.
- Metastatic cardiac involvement should be considered as a possible cause of acute coronary syndrome, especially in patients with a history of cancer.
- Cardiac magnetic resonance imaging is a key method in the differential diagnosis of myocardial injury in patients with acute coronary syndrome with non-obstructive coronary arteries.
- Modern immunotherapy is effective in reducing melanoma metastases to the heart and has improved the prognosis of patients with progressive melanoma.
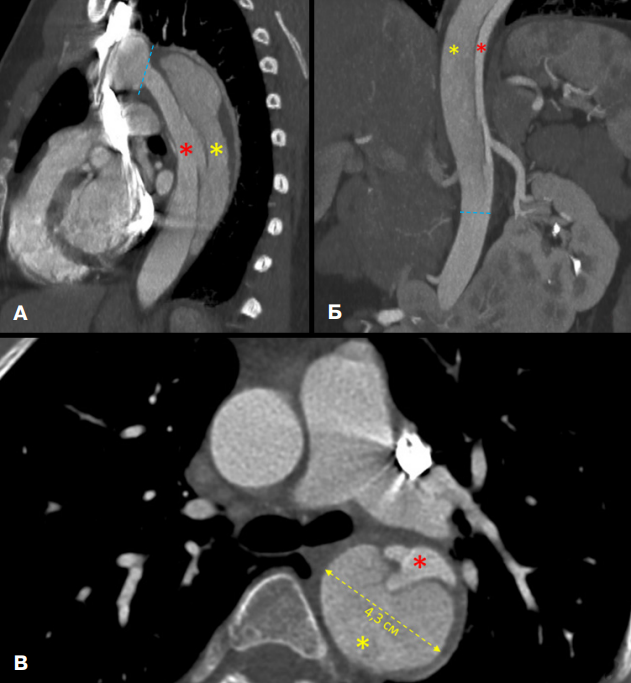
Introduction. Clinical manifestations of cardiac tumors are nonspecific and can be similar to various cardiovascular diseases. One of the most common sources of secondary cardiac tumors is melanoma. Diagnosis of melanoma with cardiac metastasis is difficult due to the predominantly asymptomatic course.
Case description. A case report describes a rare clinical manifestation of melanoma under the guise of acute myocardial infarction in a 51-year-old patient who underwent excision of upper limb melanoma, lymphadenectomy and immunotherapy 5 years ago. The patient was prescribed combination immunotherapy with nivolumab and ipilimumab. Control examination (cardiac magnetic resonance imaging, combined positron emission-computed tomography) after 3 months demonstrated significant regression of the size and metabolic activity of tumor foci both in the heart and in other organs.
Discussion. Despite the predominantly asymptomatic course, cardiac metastasis of melanoma can manifest with chest pain, ischemic abnormalities in the ECG and increased cardiac biomarkers, which creates a picture of acute coronary syndrome. The presented case demonstrates the high efficiency of combination immunotherapy in achieving regression of melanoma metastases in the heart and other organs.
- Turner syndrome is a genetic disorder characterized by polymorphism of congenital abnormalities with predominant involvement of the endocrine and cardiovascular systems, which necessitates comprehensive interdisciplinary management of patients.
- A case of a 32-year-old patient with verified Turner syndrome and DeBakey type III aortic dissection, confirmed by paraclinical investigations, is presented.
- Sustaining high clinical vigilance among physicians across all specialties regarding syndrome-specific risks and potential triggers of acute vascular events is critical for early detection of life-threatening conditions, prompt initiation of emergency interventions, and reduction of mortality.
Introduction. Turner syndrome is a genetic disorder caused by complete or partial monosomy of the X chromosome. This disease is characterized by polymorphism of congenital malformations, with predominant involvement of the endocrine and cardiovascular systems. Patients with Turner syndrome demonstrate higher morbidity and mortality rates compared to the general population, which requires comprehensive interdisciplinary approach to their management.
Brief description. The article presents a case of a patient with verified Turner syndrome (45,X karyotype), who was diagnosed with intravital aortic dissection (DeBakey type III), which became possible due to a comprehensive examination. The work describes in detail the characteristic phenotypic manifestations, clinical performance and course, analysis of risk factors, applied diagnostic and treatment methods.
Discussion. The key task of managing patients with hereditary connective tissue disorders is to maintain a high level of clinical alertness among physicians of all specialties. It is critically important not only to recognize the specific risks associated with the genetic syndrome, but also to carefully assess potential trigger factors that can provoke vascular events. Expedited clinical suspicion and verification of life-threatening emergencies, including aortic dissection, require the selection of emergent therapeutic interventions and could reduce mortality.
- The venom of some snake species has a procoagulant effect and can give an atypical picture of poisoning, including leading to cardiac complications.
- Specific anginal complaints of patients in non-standard clinical situations should immediately initiate diagnosis and care according to the standards of management of patients with myocardial infarction.
- The exact pathogenesis of coronary thrombosis following a snake bite remains open to debate.
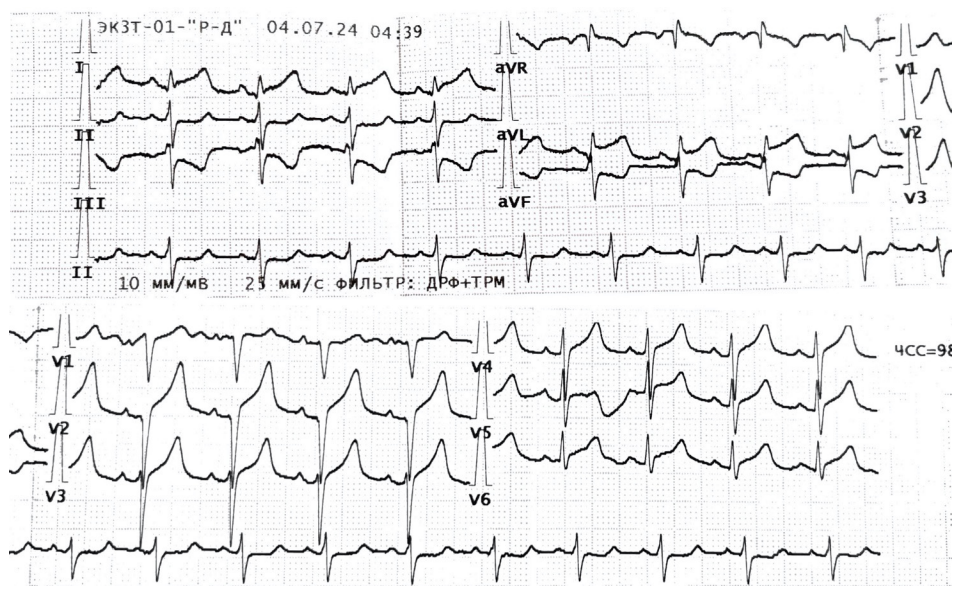
Introduction. Venomous snakes are a rare phenomenon in European Russia, and, nevertheless, bite cases are registered every year. This article presents a case of coronary thrombosis and myocardial infarction due to a bite of a venomous snake (Vipera berus) in a patient without prior coronary atherosclerosis.
Brief description. A 42-year-old patient was delivered to the emergency department of the vascular center by an ambulance team with typical anginal complaints after a bite of an unknown snake. The electrocardiogram showed ST segment elevation with corresponding reciprocal abnormalities. The patient was admitted to the X-ray operating room, where coronary artery thrombosis was detected without underlying atherosclerosis. Attempts at thrombus aspiration were ineffective and the intervention was stopped. Subsequently, the diagnosis of myocardial infarction was confirmed by paraclinical investigations. The patient’s condition remained stable, and conservative therapy complied with modern guidelines on myocardial infarction. The further course of the disease was uneventful. The patient was discharged in satisfactory condition on the 10th day of disease.
Discussion. This case is rare for Russia, but not the only one in world practice. The search query "myocardial infarction after snakebite", "myocardial infraction associated with snakebite" in the Pubmed database yields 24 case reports, most of which were described in endemic areas, mainly in Asia. The venom of some snakes has proven procoagulant activity, which is confirmed by individual studies and similar case reports. However, it is not possible to definitively rule out Kounis syndrome in these circumstances, which leaves the exact pathogenesis of coronary thrombosis after a snakebite open to discussion.
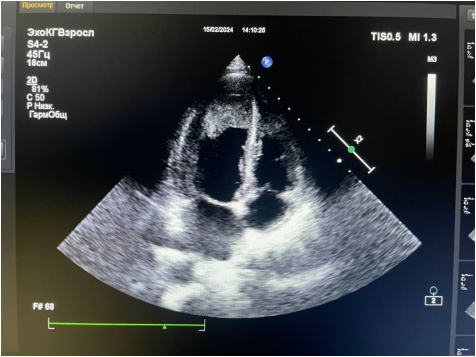
- A case of Loeffler endomyocarditis with biventricular involvement against the background of hypereosinophilic syndrome in a 20-year-old patient without obvious etiologic factors is presented.
- A diagnostic feature was the accidental detection of ventricular thrombosis during a pleural ultrasound performed on the 8thday after the primary echocardiography.
- The need to create a registry of patients with LE, route patients to specialized centers and manage follow-up monitoring by a multidisciplinary team is noted.
- The purpose of the presented case report is to increase physicians’ awareness of this rare pathology, since timely diagnosis and early initiation of therapy determine the long-term prognosis of patients with LE.
Introduction. Loeffler endocarditis (LE) is a rare restrictive cardiomyopathy characterized by endocardial and myocardial eosinophil infiltration followed by degranulation, intracardiac thrombus formation, and fibrosis. Fibrosis leads to progressive heart failure (HF), requiring heart transplantation in the end stage.
Brief description. A case report of a 20-year-old female patient with LE is presented. The patient presented chest pain, dyspnea, weakness, low-grade fever, and severe eosinophilia (eosinophil count up to 50%, white blood cell count up to 48×109/l). Diagnostic search for eosinophilia causes (eosinophilic leukemia, hematological malignancies, parasitic infections, systemic diseases) did not yield any results. Against the background of progressive heart failure and a decrease in the left ventricular ejection fraction to 35%, the patient was transferred to a federal center. Conservative therapy compensated heart failure, and there were no indications for heart transplantation. Over the next year, there were rehospitalizations to federal centers. Weakness, shortness of breath, grade III mitral regurgitation and eosinophilia persisted.
The absence of a permanent attending physician and supervising medical facility made follow-up difficult.
Discussion. It seems beneficial to create a registry of LE patients, route patients to specialized centers and manage outpatient follow-up by a multidisciplinary team. This case emphasizes the importance of early diagnosis and timely treatment of LE to improve the prognosis, as well as the need to increase physician awareness of this pathology.
- Fabry disease (FD) cardiomyopathy may mimic
hypertrophic cardiomyopathy and be associated with outflow tract obstruction and even midventricular obstruction. - Worldwide experience with septal reduction in patients with FD is limited to case reports and small case series.
- To our knowledge, we present the first case of alcohol septal ablation in a patient with FD and multilevel obstruction.
- Safety and efficacy of alcohol septal ablation in a patient with FD are demonstrated.
- Accumulating experience with similar procedures will contribute to the accumulation of knowledge regarding their effects on clinical and multimodality imaging parameters, and possibly improve outcomes in this population.
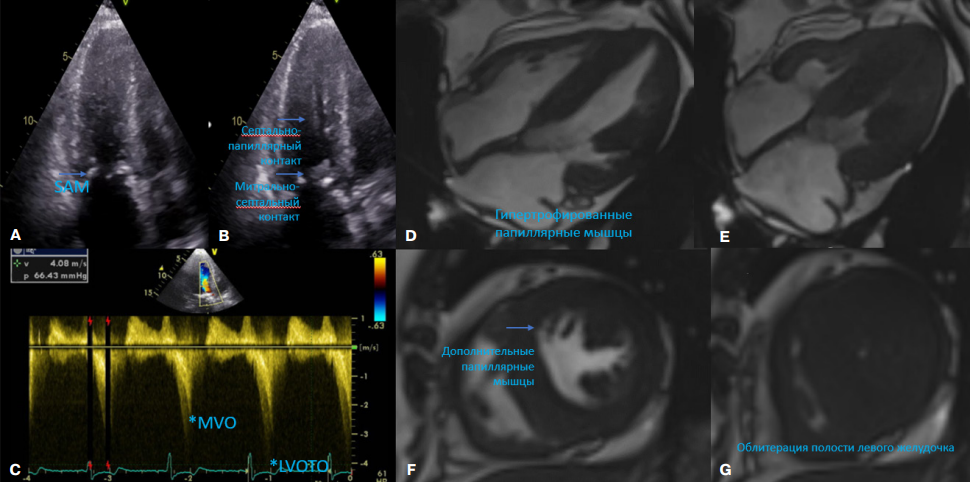
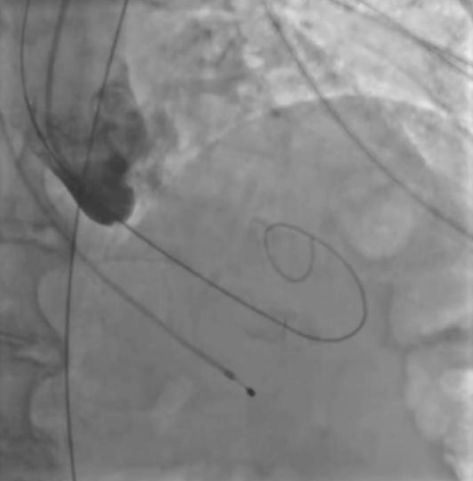
Introduction. Fabry disease (FD) can mimic hypertrophic cardiomyopathy and be accompanied by left ventricular outflow tract obstruction or midventricular obstruction. In the case of intraventricular obstruction and refractory heart failure, septal reduction may be considered.
Brief description. We present a case of alcohol septal ablation (ASA) in a female patient with genetically confirmed FD and symptomatic multilevel intraventricular obstruction. She underwent transcatheter ASA with subsequent elimination of midventricular obstruction and left ventricular outflow tract obstruction. The hemodynamic effect was maintained during the next 3-month follow-up.
Discussion. Our case shows the fact that ASA can be effective and safe in eliminating obstruction in patients with FD, provided that intracardiac hemodynamics are further monitored.
- Various strategies for transcatheter aortic valve implantation (TAVI) in patients with small left ventricular volume are presented.
- A change in the order and degree of balloon valvuloplasty is proposed to prevent left ventricular volume overload.
- Various patient management strategies can be used as guidelines for TAVI modification.
Modern treatment of severe aortic valve stenosis includes not only open surgery, but also minimally invasive transcatheter aortic valve implantation (TAVI). However, despite the reduction of periprocedural complications of TAVI with increasing experience of operators, the problem of interventions in patients with small left ventricular volume remains unclear.
It is known that with the progression of aortic stenosis, the left ventricle can undergo concentric remodeling with myocardial hypertrophy, which leads not only to a decrease in stroke volume, but also diastolic dysfunction due to increased wall stiffness. As a result, such a left ventricular phenotype, especially in combination with high pulmonary hypertension, is poorly resistant to hemodynamic overload, which carries an increased risk of intraoperative mortality. In our work, we present 3 cases of TAVI in similar patients with a small left ventricular volume, in which various modifications of the intervention algorithms were used.
- In the first case, the patient had suggested bacterial myocarditis, complicated by atrial fibrillation, cardiogenic shock, and circulatory arrest.
- In the second case, the patient’s myocarditis simulated acute coronary syndrome.
- In both cases, endomyocardial biopsy was not performed, and the diagnosis and appropriate treatment were made based on clinical data and ruling out other cardiomyopathy causes.
Myocarditis, due to the heterogeneity of manifestations and, quite often, the course unpredictability, is one of the most difficult for timely diagnosis of disease groups in modern cardiology. At the same time, myocardial inflammatory diseases often have a severe course, requiring hospitalization, monitoring and treatment in the intensive care unit, mechanical circulatory support, temporary cardiac pacing, artificial ventilation, renal replacement therapy, etc. The paper presents the experience of treating patients admitted to the Kommunarka Multidisciplinary Clinical Center with acute left ventricular failure and arrhythmias caused by myocarditis of various origin. The approach to initial therapy and differential diagnosis is described.
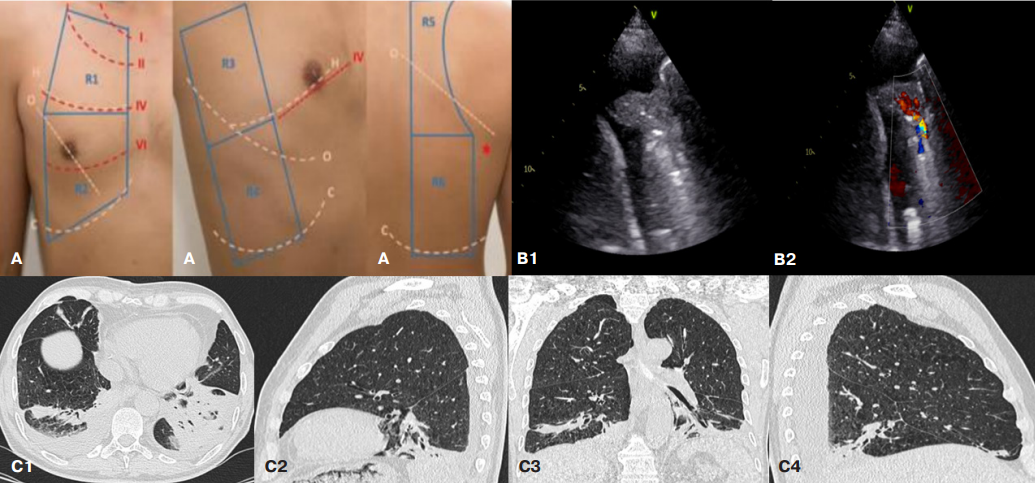
- The presented cases demonstrate the potential of lung ultrasound with color Doppler mapping for diagnosing nosocomial pneumonia after coronary artery bypass grafting.
- Lung consolidation >20 mm with increased pulmonary blood flow along with manifestations of systemic inflammatory response syndrome is promising as a criterion for postoperative nosocomial pneumonia.
Introduction. To date, diagnostic criteria for nosocomial pneumonia after open heart surgery have not been developed. The sensitivity and specificity of generally accepted criteria have not been studied, the presence of which may be due to a number of other reasons associated with surgical injury. Chest X-ray does not always reveal this complication due to postoperative chest changes. Focused lung ultrasound with color Doppler mapping seems to be a promising method for verifying pneumonia in this category of patients, not inferior to computed tomography.
Brief description. Three cases of ultrasound examination are presented, demonstrating lung parenchyma changes that are characteristic and uncharacteristic for nosocomial pneumonia.
Discussion. Focused lung ultrasound with color Doppler mapping is an informative and safe method for diagnosing pneumonia after open heart surgery.
КЛИНИЧЕСКОЕ НАБЛЮДЕНИЕ
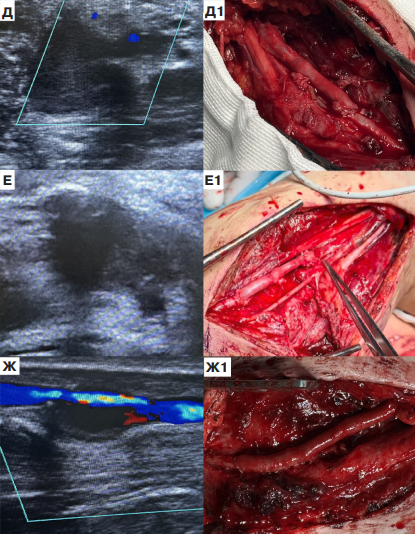
Aim. To analyze the results of surgical treatment of patients with peripheral artery pseudoaneurysmf after shrapnel wounds in a field hospital within Special Military Operation. Material and methods. From February 1, 2025 to July 1, 2025, 15 reconstructive surgeries for post-traumatic peripheral artery aneurysms were performed. All patients were men under 44 years of age. The time of aneurysm diagnostics always exceeded 21 days due to the absence of its specific symptoms. In 73,3% of cases, bleeding developed during injury, which was stopped by applying a compression bandage or tourniquet. In 19,5±3,5 days after injury, as a result of aneurysm growth, progression of perivascular edema and inflammation, symptoms of peripheral neuropathy appeared in 80% of cases.
Results. In 80%, the pseudoaneurysm diameter reached 3-5 cm. In all cases, mural thrombosis of its cavity was determined. In 1 patient, arteriovenous fistula was detected. There were following pseudoaneurysm locations: axillary artery — 26,7%, brachial artery — 20%, popliteal artery — 13,3%, posterior tibial artery — 13,3%, superficial femoral artery — 13,3%, radial artery — 6,7%, deep femoral artery — 6,7%. In 53,3%, autovenous grafting with reversed great saphenous vein was performed, while in 46,7% — artery section resection with end-to-end anastomosis. In all cases, no complications were recorded. After 19,5±2,5 days after the intervention, neuropathy regressed in 7 out of 12 patients. Patients with remaining neurological symptoms were evacuated to the next stages of rehabilitation. The rest returned to military service.
Conclusion. In a shrapnel wound of the extremities, vessel ultrasound should be routinely performed in order to search for signs of an asymptomatic pseudoaneurysm. The choice of surgical technique should always be individualized, taking into account the lesion topography. A pronounced cicatrization and close location of peripheral nerves create technical difficulties in isolating arteries and removing an aneurysm.
ISSN 2618-7620 (Online)