МИОКАРДИТ, ЭНДОКАРДИТ И КАРДИОМИОПАТИИ
- A third of patients with primary myocardial hypertrophy are diagnosed with concomitant myocarditis;
- The frequency of concomitant myocarditis is maximum with AL amyloidosis (50%) and HCM in combination with left ventricular non-compaction (40%);
- Concomitant myocarditis leads to heart failure progression, worsening ventricular arrhythmias and increasing the sudden cardiac death risk;
- Prescribing immunosuppressive therapy for myocarditis allows stabilizing the condition of patients with primary myocardial hypertrophy.
Aim. To assess the incidence of myocarditis in patients with primary myocardial hypertrophy and to study its contribution to the disease course.
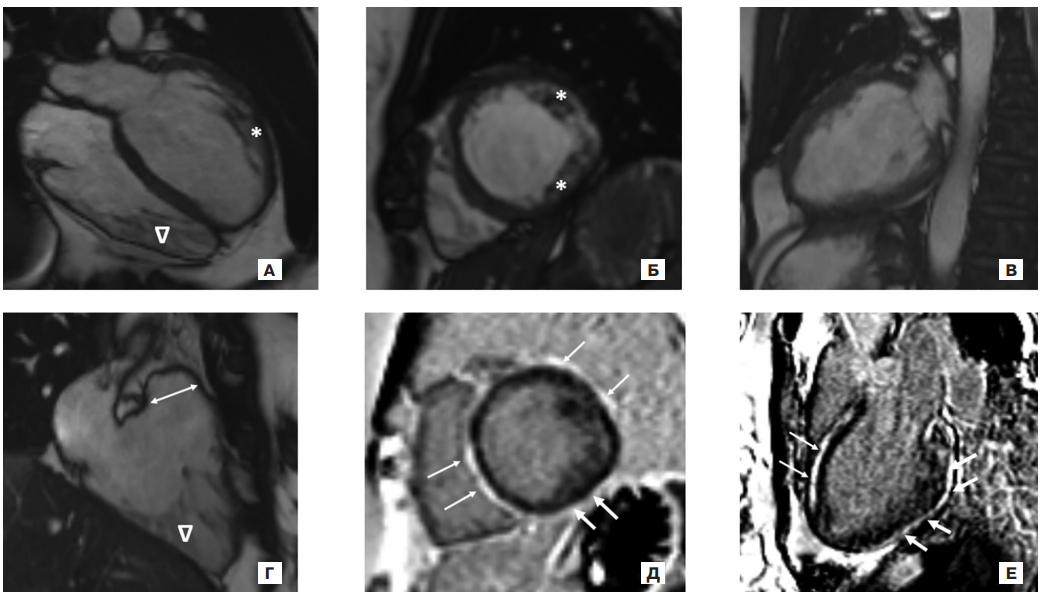
Material and methods. The study included 100 patients with primary left ventricular myocardial hypertrophy, 52 men and 48 women (mean age, 51,5±15,7 years; followup period 10,4 [2,1; 36,1] months). All patients underwent electrocardiography, 24-hour electrocardiographic monitoring, echocardiography, as well as DNA analysis (n=96), myocardium pathological study (n=29), cardiac magnetic resonance imaging (n=31), cardiac multislice computed tomography (n=26), assessment of anti-cardiac antibodies (n=43), free light chain level in serum and urine by immunofixation method (n=10); 99mTc-pyrophosphate myocardial scintigraphy (n=5); biopsy of the rectal mucosa and/or subcutaneous fat for amyloid (n=9).
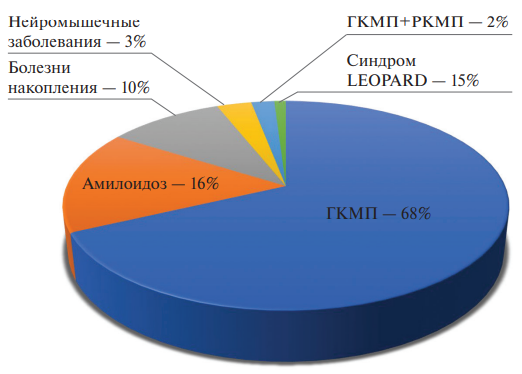
Results. In 68%, true (sarcomeric) hypertrophic cardiomyopathy (HCM) was diagnosed, in 16% — amyloidosis with cardiac involvement, in 10% — storage diseases, in 3% — neuromuscular diseases, in 2% — myocardial hypertrophy was combined with severe restriction (mixed phenotype), and in 1% — LEOPARD syndrome. Concomitant myocarditis was diagnosed in 30% of patients. In HCM, myocarditis was detected in 31% of cases. These patients had a significantly higher heart failure class (heart failure class 3 [2; 3] vs 2 [1; 3], p=0,026) and mortality (33,3% vs 6,4%, p=0,01). In amyloidosis, the incidence of myocarditis was 31,3%. In these patients, ventricular tachycardia was observed significantly more often: 80,0% vs 18,2% (p=0,036). The prevalence of concomitant myocarditis in the subgroup of storage diseases was 30%: 2 patients with Fabry disease and 1 patient with Danon disease. Of the three patients with neuromuscular diseases, myocarditis was diagnosed in 1. In the subgroups with the restrictive phenotype and LEOPARD syndrome, no cases of myocarditis were recorded. Treatment of myocarditis made it possible to stabilize the patients' condition.
Conclusion. Concomitant myocarditis led to heart failure progression, worsening ventricular arrhythmias and, as a consequence, an increased risk of sudden cardiac death. It is necessary to actively diagnose and treat myocarditis in patients with primary myocardial hypertrophy.
- Significant variability in alcoholic cardiomyopathy (code I42.6) mortality rates may be due to controversial issues in diagnosis and determining the underlying cause of death.
- The article presents factual data and problems of their interpretation.
- Creating an interdisciplinary consensus on the completion of medical death certificates is proposed.
Alcoholic cardiomyopathy (ACM) is considered an independent disease, the diagnosis of which is based largely on prior alcohol abuse and the exclusion of other cardiomyopathy causes.
Aim. To discuss the accounting and accuracy of the analysis of ACM mortality, including assessing the variability and changes of regional standardized mortality rates (SMR) for 2013-2021, as well as to conduct an analysis of Medical Certificate of Cause of Death (MCCD) and discuss the criteria for ACM as the underlying cause of death (UCD).
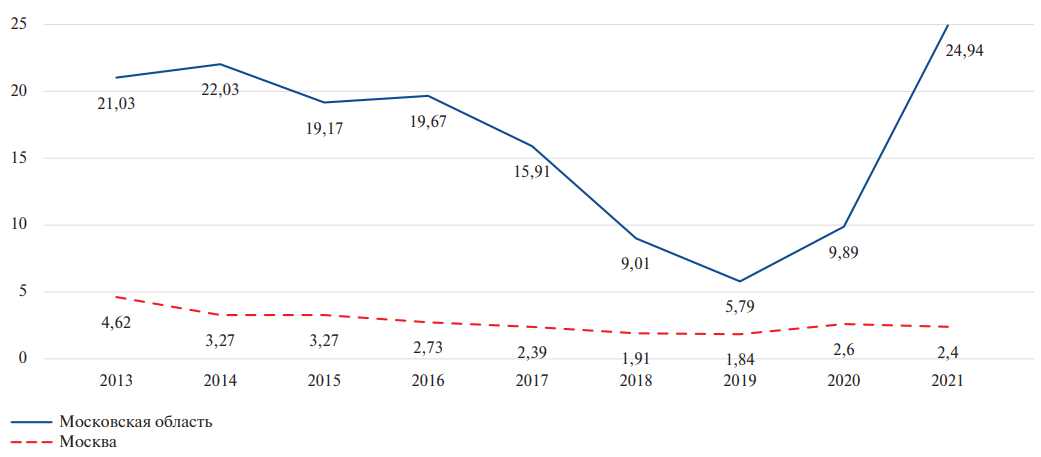
Material and methods. Rosstat data on the average annual population and ACM death rate (I42.6) in 2013-2021 by region were analyzed. SMRs were calculated using software. To analyze MCCDs, anonymized data from the Department of Civil Registration of the Moscow Oblast (3538 MCCDs in total) were used.
Results. In 2013, the regional average SMR from ACM was 14,0±13,9 per 100 thousand population, in 2021 — 13,2±13,6. The only region with annual SMR decrease was the Tyumen Oblast. Zero values were registered in the republics of Ingushetia and Chechnya. In other regions, “wave-like” changes were noted — a decrease or increase in SMR. The coefficient of variation of the SMR was minimal in 2016 (73%) and maximum in 2021 (103%). The contribution to mortality varied from 0 to 6%. Heart failure group codes (I50) were indicated as the immediate cause of death in 93,3% of MCCDs. Part II of the MCCDs was completed in 39,1%. The most common cause of death is group F10 (mental and behavioural disorders due to use of alcohol) and group K70 (alcoholic liver disease). In the literature and guidelines there are no clear criteria for ACM as UCD. The indication of alcohol-related codes in Part II of the MCCD is contrary to the ICD rules.
Conclusion. Significant regional variability in SMR from ACM may be due to problems in UCD determination. And despite the small contribution of ACM to allcause mortality, a consensus statement is required on the criteria for diagnosing and completing the MCCD.
- The development of COVID-19-associated myocarditis has not been confirmed in any patient in the post-acute period. Cardiac symptoms of postCOVID-19 syndrome may be a consequence of myocardial remodeling.
- Immunohistochemical study revealed the SARSCoV-2 spike protein expression on the inflammatory infiltrate cells in the myocardium and endothelium of single vessels, but was not confirmed using PCR.
- According to endomyocardial biopsy, the morphological manifestations of post-COVID-19 syndrome are associated with an increase in the number of CD68+ macrophages in the myocardium. An increase in M2 macrophages may indicate myocardial repair after tissue damage during the acute period of coronavirus infection.
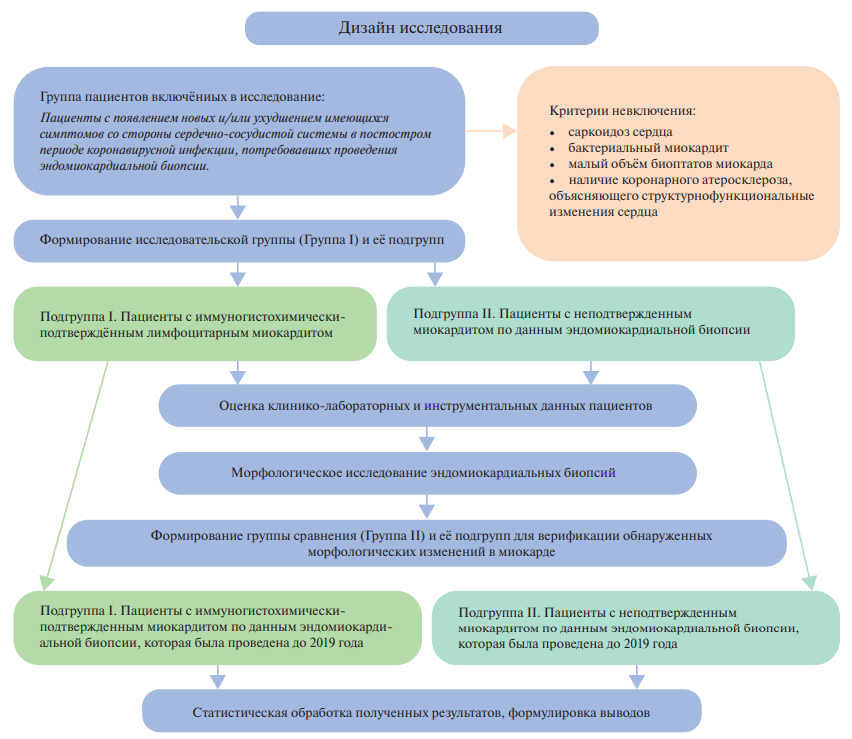
Aim. To characterize the clinical manifestations and myocardial morphological changes in patients with cardiovascular complications of post-Covid syndrome.
Material and methods. A total of 38 patients (Group I) with cardiac symptoms in the post-COVID-19 period underwent endomyocardial biopsy (EMB). Patients from group I were divided into 2 subgroups depending on the presence of morphologically verified myocarditis. For morphological comparison, group II was formed (41 patients without COVID-19 and with EMB performed before 2019). Group II was also divided into two subgroups with and without morphologically verified myocarditis. In addition to the analysis of clinical and paraclinical data, a histological and immunohistochemical study of myocardial tissue was carried out with anti-CD3, CD68, CD16, HLA-DR, MHC1, C1q, enterovirus VP1, SARS-CoV-2 spike protein, ACE2, Ang1, von Willebrand factor, VEGF antibodies, as well as a PCR of myocardial tissue after reverse transcription. Additionally, an immunofluorescent study of myocardial tissue was performed using antibody cocktails to SARS-CoV-2/ CD16 spike protein, SARS-CoV-2/CD68 spike protein, CD80/CD163. Statistical processing was performed using the NumPy, SciPy, Pandas and Matplotlib libraries in the Python programming language.
Results. Among patients in group I, 65% had morphologically verified lymphocytic myocarditis (subgroup 1, n=29). Other 35% of patients had no signs of myocardial inflammation (subgroup 2, n=9). The comparison group (group II) included 33 patients with myocarditis (80%) and 8 patients (20%) without it. There was a pronounced expression of CD68+ macrophages in the myocardial tissue in patients with postCOVID-19 syndrome in comparison with group II, both with morphological criteria for myocarditis (p=0,014) and without it (p=0,007), mainly due to M2 macrophages. More pronounced expression of CD68+ macrophages was observed when EMB was performed at earlier stages. If SARS-CoV-2 spike protein was detected in group I on the endothelium and inflammatory infiltrate by the immunohistochemistry, PCR of myocardial tissue for SARS-CoV-2 (n=5) was performed, which did not reveal SARS-CoV-2 particles in any of the analyzed samples.
Conclusion. Cardiac symptoms of post-COVID-19 syndrome are caused by myocardial remodeling, including in patients without morphologically verified myocarditis. The direct involvement of SARS-CoV-2 in the development of myocarditis in the post-acute period of COVID-19 has not been proven.
- Atrial fibrillation (AF), as one of the most common sustained atrial tachyarrhythmias in the population, has demonstrated a relatively low prevalence in patients with dilated cardiomyopathy (DCM) at long term follow-up compared with the incidence of ventricular tachyarrhythmias (27,8% vs 60,4%; p=0,0001).
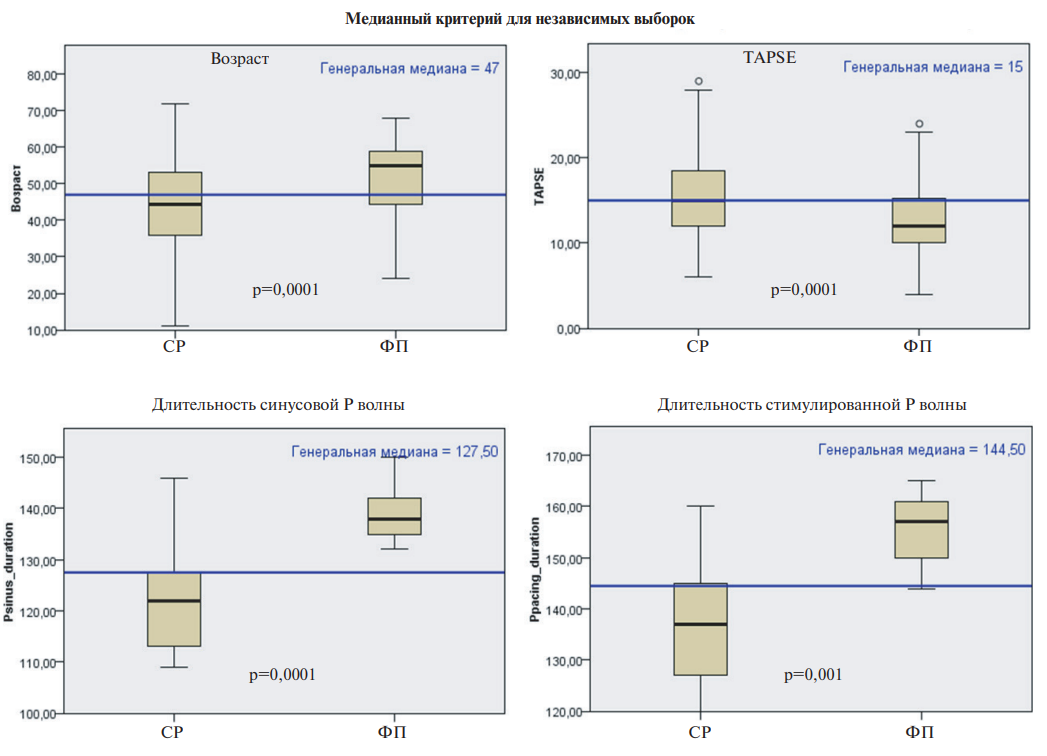
- Among the risk factors of unfavorable cardiac remodeling in patients with DCM, independent predictors of AF have been identified: atrial dromotropic dysfunction (interatrial block), right ventricular contractile dysfunction (decreased TAPSE) and increased heart rate during therapy.
- The development of persistent AF in patients with DCM is associated with a 4-fold increase in the risk of cardiovascular death; the 6-year probability of death is 80%.
Aim. To study the epidemiological profile and long-term prognostic significance of atrial fibrillation (AF) as a risk factor for adverse clinical outcomes in patients with dilated cardiomyopathy (DCM).
Material and methods. The study included 270 patients with DCM (206/76,3% men, age 47 [37; 56] years, left ventricular (LV) ejection fraction 29 [21; 35]%). The observation period was 6 years (Me 76 [57; 119] months). To assess the effect of AF on DCM prognosis, Kaplan-Meier curves and Cox regression of clinical outcomes, including cardiovascular death, heart transplantation, and ventricular assist device implantation, were analyzed.
Results. Of 270 patients with DCM, paroxysmal AF was detected in 10 (3,7%) patients (initial, 5/1,85%; during the first follow-up year, 5/1,85%). After 5 years, another 65 (24,1%) individuals had AF (paroxysmal, persistent or permanent). Ventricular tachyarrhythmias were registered in 163 (60,4%) patients. Compared with patients maintaining sinus rhythm, patients with AF were older (51,4±10 vs 43,6±13 years, p=0,001) and had lower exercise tolerance (6-minute walk test: 379±45 vs 445±43 meters; p=0,0002) and a higher heart failure functional class (NYHA class III-IV: 38/50,7% vs 52/26,7%; χ2=13,6; p=0 ,0003). In patients with AF, initially more pronounced manifestations of right ventricular contractile dysfunction (TAPSE: 13,1±3,4 vs 15,5±4,6 mm; p=0,0001) and LV diastolic dysfunction (E/A: 2,9±1,5 vs 2,1±1,3; p=0,006; E/e' 15,6±6,9 vs 11,8±7,2; p=0,019), more dilated left atrium (left atrial volume index: 63,3±19 vs 50±18,7 ml/m2; p=0,006). During the 6-year median follow-up, AF was observed in 75 patients (0,46 new cases/100 patients/year). As a result of Cox regression analysis, AF as a time-dependent factor was identified as an independent predictor of cardiovascular death (hazard ratio 3,99; 95% confidence interval, 1,67-8,59; p=0,0001).
Conclusion. AF, as one of the most common sustained atrial tachyarrhythmias in the population, demonstrated a lower prevalence (27,8%) in the DCM cohort compared to ventricular tachyarrhythmias (60,4%), but a high prognostic significance of the negative impact on the risk of fatal outcomes. The development of AF in patients with DCM is associated with a 4-fold increase in cardiovascular death risk over a 6-year period.
- Cardiac amyloidosis performance is in many ways similar to hypertrophic cardiomyopathy.
- Symmetrical left ventricular wall thickening, granular and sparkling appearance of the myocardium and thickened heart valves were the best cardiac predictors of cardiac amyloidosis.
- Age above 63 years, decreased glomerular filtration rate, and proteinuria are the best noncardiac predictors of cardiac amyloidosis.
Cardiac amyloidosis performance is in many ways similar to hypertrophic cardiomyopathy (HCM), and therefore it is extremely difficult to distinguish these two diseases in practice. The present study was performed to identify features that aid in the differential diagnosis by analyzing clinical, electrocardiographic, echocardiographic and laboratory data in patients with systemic amyloidosis and HCM. In the study, 38 patients with cardiac amyloidosis and 80 patients with HCM were examined. It was found that symmetrical left ventricular (LV) wall thickening, granular and sparkling appearance of the myocardium and thickened heart valves were the best cardiac predictors, and age above 63 years, decreased glomerular filtration rate and proteinuria were the best non-cardiac predictors of cardiac amyloidosis, whereas low QRS voltage and pericardial effusion were of less clinical significance. Systolic anterior motion of the anterior mitral leaflet, asymmetric LV wall thickening, and electrocardiographic signs of LV hypertrophy were highly suggestive of HCM. Thus, standard noninvasive methods may be useful for identifying myocardial infiltrative processes and differentiating cardiac amyloidosis from HCM.
- Desmoplakin cardiomyopathy (CMP) is a unique CMP characterized by predominant LV involvement with extensive subepicardial fibrosis, life-threatening ventricular arrhythmias, and episodes of myocardial inflammation. However, given the recent identification of desmoplakin CMP as a separate clinical entity, the management of such patients, including the prevention of sudden cardiac death (SCD), remains controversial.
- The article presents a case of a family with desmoplakin CMP, as well as a review of current literature data on this disease.
- The need to use a genotype-specific diagnosis, choice of management tactics and prevention of SCD in patients with desmoplakin CMP is em - phasized.
Inherited cardiomyopathies (CMP) are a group of heterogeneous diseases characterized by myocardial disorders that is not caused by coronary artery disease, hypertension, valvular and congenital defects. With the development of imaging methods and molecular genetic diagnostics, it has become clear that many CMPs are characterized by phenotypic and genotypic "crossover". And although the genetic component does not always determine the specific phenotype of the disease, genetic testing plays a significant role in risk stratification, determining the prognosis and management of patients, as well as conducting family screening. Considering the high diagnostic and prognostic value of genotype, novel genotype-based strategies for classifying CMP have been proposed in recent years. One example of such a genotype-specific approach is the identification of desmoplakin CMP as a separate independent clinical entity. The article presents a case of a family with a pathogenic DSP gene variant (p.Gln948LysfsTer29) identified in three generations, leading to the development of a specific CMP phenotype. A comprehensive examination was carried out. We demonstrated the stages of natural disease course, as well as management strategy for patients with desmoplakin CMP were proposed.
- Secondary infective endocarditis is more common with a bicuspid aortic valve.
- Among patients with native valve endocarditis, according to histological examination, subactive disease forms are often found.
- Patients with prosthetic valve endocarditis have higher pathological activity
Aim. To evaluate clinical and morphological data of infective endocarditis (IE) of native and prosthetic heart valves.
Material and methods. This retrospective cohort study included 354 patients that had signs of IE according to pathological study of surgical material from native valves and prosthetic heart valves. The patients were divided into two groups: the first group included patients with native valve IE (n=328), while the second group — with prosthetic valve IE (n=26).
Results. Among patients with native valve IE, aortic (AV) and mitral valve (MV) IE was recorded in 67,6% and 20,7%, respectively. In the group of patients with prosthetic IE, AV IE also predominated — 57,7% vs 26,9% in MV IE. In the majority of patients in the first group, secondary IE was detected (68,9%). The development of IE in the presence of bicuspid AV (BAV), degenerative AV disease, and rheumatic valve disease was revealed in 40,7%, 31,4% and 6,7%, respectively. In the group of patients with native valve IE, subactive IE was most often detected — in 38,4%, while in 7,1% — signs of process remission were detected. In the group of patients with prosthetic valve IE, IE with moderate activity was detected more often than in the group of patients with native valve IE (42,3% vs 26,8%, p=0,042). In the group of patients with prosthetic valve IE, the presence of colonies of microorganisms and neutrophilic infiltration in the histological material was somewhat more common, while in patients with native valve IE there was a tendency towards a higher percentage of necrosis in the studied material (42,4% vs 38,5%, p>0,05).
Conclusion. This work confirms changes in the epidemiological characteristics of patients with IE. A high frequency of subactive forms of IE was noted according in patients with native valve IE, which requires individual approach to antibacterial therapy depending on the pathomorphological IE activity.
МАРКЕРЫ ДИАГНОСТИКИ И ФАКТОРЫ РИСКА
What is already known about the subject?
- Apoptosis is considered one of the morphological features characteristics of various types of regulated cell death.
- Apoptosis of cardiomyocytes is the leading process in ischemia development.
- As a result of exposure to trigger factors, morphological signs of apoptosis are found in all atheroma cells, which can subsequently lead to plaque instability with an increased risk of thrombosis and rupture.
What might this study add?
- Studying the relationship between apoptosis markers Bax, Bcl-2, Bcl-2/Bax, p53, TRAIL with the severity of coronary atherosclerosis and clinical and paraclinical characteristics demonstrates the predominance of apoptosis processes in patients with coronary artery disease and may create prospects for the creation of novel treatment and diagnostic strategies.
Aim. To assess markers of serum apoptosis markers depending on the severity of coronary atherosclerosis, as well as to study their relationship with clinical and paraclinical characteristics of patients with coronary artery disease (CAD).
Material and methods. The study included 176 people (105 men and 71 women), of which 150 were patients with an established diagnosis of CAD, 26 — healthy volunteers (control group). The patients were divided into the following groups: group 1 — with coronary atherosclerosis without stenosis (n=17); group 2 — with hemodynamically insignificant (stenosis <50%) coronary atherosclerosis (n=21); group 3 — with hemodynamically significant (stenosis >50%) coronary atherosclerosis (n=112). Group 4 was represented by healthy volunteers (n=26). Patients underwent coronary angiography using the SYNTAX score, echocardiography, extracranial artery duplex ultrasound. All subjects were studied for the serum level of apoptosis markers Bcl-2, Bax, Bcl-2/Bax, TRAIL and p53. Statistical processing was carried out using the Statistica 10.0 software. Differences were considered significant at p<0,05.
Results. There was a very high correlation between the Bcl-2 (r=-0,84; p<0,001), Bax (r=0,83; p<0,001), Bcl-2/Bax (r=-0,86; p<0,001), p53 (r=0,80; p<0,001), TRAIL (r=-0,78; p<0,001) and the severity of coronary atherosclerosis. A correlation of varying strength and significance was revealed between the values of these apoptosis markers and a number of clinical and paraclinical characteristics of patients. In addition, there were significant differences (p<0,001) in Bcl-2, Bax, Bcl2/Bax, p53 and TRAIL between groups of patients with multifocal atherosclerosis, restenosis after previous revascularization and a history of myocardial infarction in comparison with patients without these signs.
Conclusion. The correlations we have identified between laboratory signs of apoptosis and coronary lesions, clinical and paraclinical characteristics of patients, as well as the detected reliability of differences between groups with multifocal atherosclerosis, coronary artery restenosis and myocardial infarction in history, make it possible to consider these biomarkers as indicators of atherosclerosis severity. This can also be the basis for the development of novel treatment and diagnostic strategies.
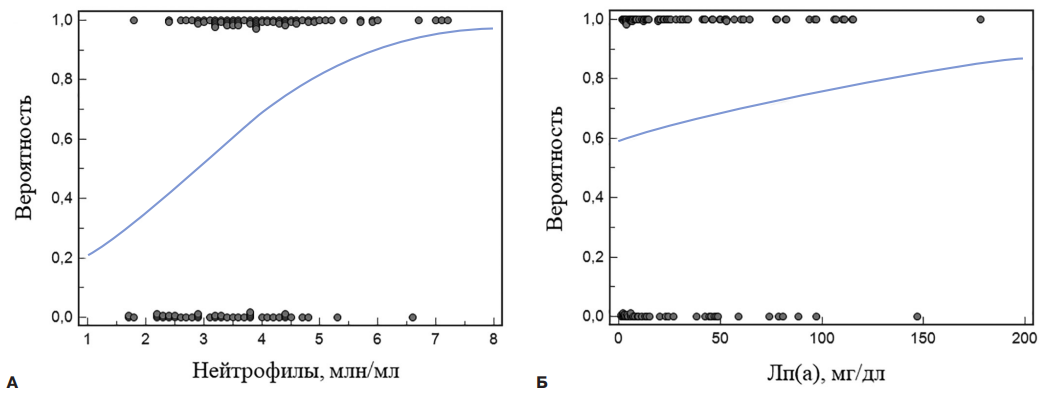
- The combination of high neutrophil count and Lp(a) levels increases the risk of diffuse coronary atherosclerosis in patients over 60 years of age.
- Lipoprotein(s) is capable of causing activation of neutrophils in whole blood, as well as the formation of neutrophil extracellular traps in primary cell culture.
Aim. To assess the level of lipoprotein (a) (Lp(a)) and other lipid profile parameters, the composition of blood leukocytes in patients with focal and diffuse coronary atherosclerosis who underwent coronary artery bypass surgery (CABG), as well as to study the effect of Lp(a) on the activation of leukocytes in vitro.
Material and methods. The study included 120 male patients (mean age, 67±5 years) with multivessel coronary artery disease after elective CABG surgery. According to the type of coronary artery involvement, patients were divided into groups of diffuse (n=77) and focal (n=43) atherosclerosis. In peripheral blood samples, the content of the main fractions of lipoproteins, including Lp(a), was determined. Activation of neutrophil granulocytes upon addition of Lp(a) was assessed in whole blood and in primary cell culture.
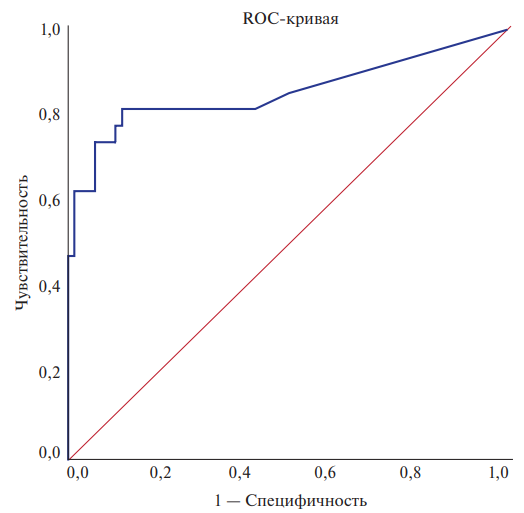
Results. In patients with diffuse coronary stenosis, there was a tendency to higher Lp(a) levels; no changes in other lipid profile parameters were detected. In this group of patients, an increase in the absolute leukocyte count was noted due to neutrophilic granulocytes. An absolute neutrophil count >2,9 million/mL was associated with diffuse disease (AUC, 0,69 (95% confidence interval (CI) 0,600,77), p=0,0002, sensitivity 85%, specificity 42%). In patients with Lp(a) ³30 mg/dL, the diagnostic value of a neutrophil count >2,9 million/mL for diffuse stenosis was higher (AUC, 0,74 (95% CI 0,60-0,86), p= 0,005, sensitivity 90%, specificity 48%). According to logistic regression analysis with the introduction of neutrophils and conventional risk factors (age, body mass index, hypertension and smoking) into the model, only the number of neutrophils above the threshold level remained an independent factor in diffuse coronary stenosis. Lp(a) can induce neutrophil activation, detected by increased CD66b overexpression in whole blood, as well as the formation of neutrophil extracellular traps in primary cell culture.
Conclusion. Neutrophil granulocytes can participate in the formation of diffuse atherosclerotic coronary lesions. One of the neutrophil activators may be Lp(a). The combination of high neutrophil count and Lp(a) level in the blood increases the risk of diffuse coronary atherosclerosis.
What is already known about the subject?
- Anthropometry is a method widely used in sports to evaluate physical characteristics and select athletes that can improve performance.
What might this study add?
- Anthropometric characteristics are important components and criteria for assessing the cardiovascular system function in qualified athletes.
- The relationships between characteristic anthropometric parameters and cardiac hemodynamics established by correlation analysis are determined by the type of sport and the duration of training.
How might this impact on clinical practice?
- Dynamic monitoring of anthropometric data and cardiac hemodynamics is necessary in the process of training qualified athletes and in predicting sports results.
Aim. To assess the anthropometric characteristics and functional state of the cardiovascular system in qualified athletes of various sports.
Material and methods. A total of 136 male athletes were examined. Qualified athletes (n=116) (age, 22,07±4,10 years, sports experience 9,56±3,08 years) were divided into groups: I (n=30) — wrestling, judo, II (n=27) — cross-country skiing, biathlon, III (n=33) — powerlifting, IV (n=26) — volleyball. Control group (n=20) consisted of those training less than 3 years. We performed anthropometry with assessment of body height and weight, chest circumference, body surface area, body mass index (BMI), Pignet index, Erisman index, grip and back strength test. Echocardiography, cycle ergometry with assessment of physical working capacity (PWC170) and maximum oxygen consumption (MOC). The relationship between traits was assessed using the Spearman rank correlation coefficient (rs). Critical significance level was p=0,05.
Results. According to echocardiography, qualified athletes had significant differences in structural parameters. Group II was characterized by an increase in left ventricular (LV) volumetric dimensions and identified correlations of BMI and body surface area with end-diastolic dimension (r=0,602), end-diastolic volume (r=0,591), end-systolic volume (ESV) (r=0,429), stroke volume (r=0,597), PWC170 (r=0,550). Groups I and III were characterized by an increase in LV posterior wall (LVPWT) and interventricular septal (IVST) thickness. In group I, there was a relationship between body surface area and LVPWT (r=0,413); Pignet index with MOC (r=0,623); PWC170 with Erisman index (r=0,573), strength of the right (r=0,610) and left hand (r=0,515), back muscles (r=0,445). Group III had the highest BMI and body surface area, while relationships were identified with LVPWT (r=0,426), IVST (r=0,409), LV mass (LVM) (r=0,453), and back muscle strength (r=0,464); the Erisman index correlated with LVM index (r=0,359). In group IV, the parameters of height, body weight and body surface area are interrelated with LVM (r=0,731), LVPWT (r=0,523), IVST (r=0,399), ESV (r=0,504), end-systolic dimension (r=0,467), right hand strength (r=0,583).
Conclusion. The relationships established by correlation analysis showed that anthropometric features are important components and criteria for assessing cardiac hemodynamics function in qualified athletes, depending on the type of sport and the duration of training, which must be taken into account when achieving sports results.
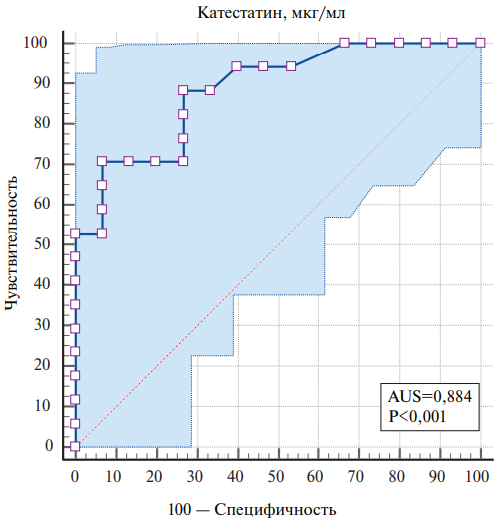
- Catestatin levels were inversely associated with the severity of heart failure with preserved ejection fraction (HFpEF).
- Catestatin values were inversely correlated with left ventricular remodeling, as well as with levels of N-terminal pro-brain natriuretic peptide and high-sensitivity C-reactive protein.
- Decreased catestatin ≤132,83 µg/ml (AUC=0,884; sensitivity, 70,59%; specificity, 93,33%; p<0,001) was associated with HFpEF in patients with nonobstructive coronary artery disease.
Aim. In patients with non-obstructive coronary artery disease (CAD), to evaluate the pathophysiological significance and diagnostic effectiveness of catestatin in detecting heart failure with preserved ejection fraction (HFpEF), as well as to assess the relationship of the levels of this biomarker with heart rate variability (HRV) parameters and the severity of diastolic dysfunction.
Material and methods. The study included 83 patients (44 men, mean age, 62,0 [57,0; 68,5] years) with non-obstructive CAD and preserved left ventricular (LV) ejection fraction of 63 [60; 64]%). Echocardiography was performed according to a standard protocol. HRV was assessed using 24-hour electrocardiographic monitoring. Serum biomarker levels were determined using enzyme-linked immunosorbent assay.
Results. Patients were divided into groups depending on HFpEF presence: group 1 (n=63) included patients with newly diagnosed HFpEF, and group 2 included patients without heart failure (n=20). Serum catestatin concentrations were 43,1% lower (p<0,001) in patients with HFpEF than in patients without it. Catestatin had a negative correlation with levels of N-terminal pro-brain natriuretic peptide and C-reactive protein. Moreover, serum catestatin values were inversely correlated with LV remodeling parameters, whereas no relationship was found with HRV values. According to ROC analysis, catestatin £132,83 μg/ml (AUC=0,884; p<0,001) were defined as threshold values associated with HFpEF.
Conclusion. Decreased serum catestatin concentrations were associated with HFpEF and overexpression of heart failure and inflammation biomarkers. Moreover, serum catestatin values had a negative relationship with LV remodeling parameters, while no relationship was found with HRV values.
What is already known about the subject?
- Surrogate markers of the intestinal wall and microbiota (calprotectin and zonulin) are considered as novel non-conventional cardiovascular risk factors, but studies have been carried out mainly in patients with inflammatory bowel and rheumatic diseases.
What might this study add?
- A high prevalence of elevated calprotectin and zonulin levels was shown in a population sample of St.Petersburg residents with metabolic disorders, which is associated with carotid atherosclerosis.
- We demonstrated association of calprotectin and zonulin levels with dietary patterns, dyslipidemia, obesity, circulating biomarkers and comorbidities.
How might this impact on clinical practice?
- Elevated levels of calprotectin and zonulin in patients with initial metabolic disorders will allow the doctor to focus on priority prevention areas — searching for atherosclerotic changes in the arteries and changing dietary patterns.
Surrogate markers quantifying the severity of intestinal inflammation (fecal calprotectin) and permeability (fecal zonulin) are currently considered nontraditional cardiovascular risk factors.
Aim. To study the associations of fecal zonulin and calprotectin levels with cardiovascular risk factors and target organ damage among participants with metabolic disorders from a population sample of St. Petersburg residents aged 35-75 years.
Material and methods. In-depth phenotyping was performed on patients from a cohort of St. Petersburg residents metabolic disorders (overweight, hyperglycemia) invited for reexamination as part of the ESSE-RF epidemiological study. All patients underwent a questionnaire examination (physical activity, smoking, alcohol consumption, sleep, stress, anxiety and depression, assessment of digestive system complaints, frequency of food consumption). In addition, blood pressure and pulse measurements, anthropometry, biochemical and hormonal blood tests, echocardiography, applanation tonometry, volume sphygmography, duplex carotid scanning, and determination of fecal zonulin and calprotectin levels were carried out.
Results. The examined cohort (n=86; mean age, 56 [44,7;63,5] years; men, 49,5%) was characterized by a high prevalence of abdominal obesity (80,2%), dyslipidemia (low-density lipoproteins >3 mmol/l — 76,7%, triglycerides ³1,7 mmol/l — 43%, total cholesterol >4,9 mmol/l — 77,9%) and insulin resistance (64%) with slight sex differences. An increase in calprotectin occurs in 23,3% of patients, zonulin — in 30,3%, while an increase in calprotectin and/or zonulin occurs in almost half of those examined (47,7%). Fecal calprotectin levels are associated with indicators of dyslipidemia, obesity, inflammation and atherosclerotic vascular disease, as well as dietary patterns and socioeconomic indicators. Zonulin levels are associated with N-terminal probrain natriuretic peptide levels and the presence of vitamin D deficiency, gallbladder disease, and dietary patterns.
Conclusion. Increase of at least one marker of intestinal permeability and inflammation occur in approximately half of the participants with metabolic disorders from a population sample of St. Petersburg residents. In addition to the association of calprotectin and zonulin with metabolic risk factors and dietary patterns, calprotectin levels were associated with atherosclerotic changes in the carotid arteries.
- Arrhythmias are common in patients with undifferentiated connective tissue disease and are often the cause of sudden cardiac death.
- The association of N-terminal pro-brain natriuretic peptide with premature ventricular contractions and mitral regurgitation in young patients with undifferentiated connective tissue disease suggests its diagnostic role in this cohort of patients.
- The study results in the future may contribute to the development of individual programs for the management of patients with connective tissue disease.
Aim. To study the relationship between the level of N-terminal pro-brain natriuretic peptide (NT-proBNP) and myocardial abnormalities in patients with cardiac arrhythmias due to undifferentiated connective tissue disease (UCTD).
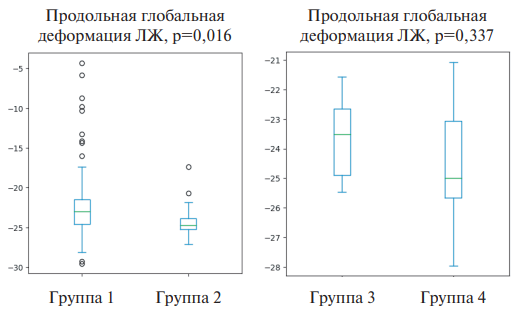
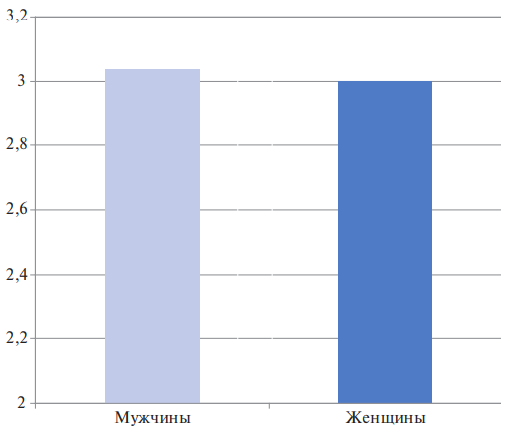
Material and methods. This cross-sectional comparative study included young and middle-aged patients with arrhythmias due to UCTD: group 1 (18-44 years old, n=127), group 3 (45-59 years old, n=10). The control groups (n=30, group 2; n=8, group 4) included volunteers with single phenotypic signs of UCTD, comparable in age and sex. A standard clinical examination, 72-hour electrocardiographic monitoring, Speckletracking echocardiography, and NT-proBNP level assessment were performed.
Results. In patients of groups 1 and 3, a significant increase in the concentration of NT-proBNP was noted compared to the control groups. At the same time, the average NT-proBNP level in the study groups did not exceed the reference values. Significant correlations were revealed between NT-proBNP and heart rate (r1=0,462, p=0,010; r3=0,397, p=0,034), UCTD diagnostic cut-off level (r1=0,496, p=0,001; r3=0,401, p=0,043), the presence of mitral valve prolapse (r1=0,469, p=0,002) and mitral regurgitation (r1=0,53, p=0,008), premature ventricular contractions (PVCs) of class III (r1=0,582, p=0,045), IVa (r1= 0,39, p=0,042) and V (r1=0,397, p=0,037); cardiac index (r1=-0,329, p=0,037) and ejection fraction (r1=-0,407, p=0,044). However, no significant correlation was found between the left ventricular global longitudinal strain and NT-proBNP level.
Conclusion. The study demonstrated the association of NT-proBNP level with UCTD diagnostic cut-off level, mitral valve prolapse, mitral regurgitation, and PVCs, which makes possible the use of this biomarker as an additional diagnostic criterion for myocardial changes in against the background of UCTD.
STRESS IN THE POPULATION
- In working-age population, a high level of chronic stress is detected on average in every tenth person.
- In some cities, sex differences in the incidence of high chronic stress are identified.
- At the same time, the average level of chronic stress was determined in 43% of the working-age population.
Aim. To assess the prevalence of chronic stress in the adult population in the Vladimir region, taking into account sex characteristics.
Material and methods. This cross-sectional population study was performed in five cities of the Vladimir Oblast (Vladimir, Kovrov, Murom, Yuryev-Polsky and Vyazniki) from May 2018 to March 2020. From six health care facilities, 9 therapeutic areas were selected. Then, from the assigned population aged 30-69 years, respondents from each area were invited to the study. To identify chronic stress, the Reeder questionnaire was used, which makes it possible to identify three types of disorders: low, moderate and severe stress. The study analyzed fully completed Reeder L. chronic stress questionnaires from 1081 respondents (393 men and 688 women).
Results. Among men, every second person has a low chronic stress, 42% — moderate stress, while high chronic stress was found in 6.4% of cases. A similar trend is observed among women. High levels of chronic stress were detected in 8% of women, and the gap between the prevalence of low and moderate chronic stress was minimal. In general, the prevalence of various levels of chronic stress between men and women was comparable, without significant differences. Sex variability in the prevalence of chronic stress was revealed in various cities of the Vladimir Oblast. In Vladimir, the prevalence of high stress among men was three times higher than in women, while in Vyazniki and Kovrov the opposite pattern was observed. In the other two cities (Murom and Yuryev Polsky), the prevalence of high chronic stress between men and women was comparable.
Conclusion. In the working-age population, a high chronic stress level is detected in up to 10%. In some cities, there are sex differences between men and women. The mean level of chronic stress is determined in 42-43% of cases. The results obtained indicate the need for large-scale preventive measures to combat chronic stress among working-age men and women of in the Vladimir Oblast.
- Clinical interaction as a genre of interpersonal communication is a full-fledged factor influencing the pathogenesis and salutogenesis through psychosomatic relationships.
- The biographical side of medical problems is associated with a unique system of meanings for each person that has developed throughout life and determines the experience of each new event and new information.
- In contrast to the biomedical approach to disease, the biographical approach requires developed humanitarian and communication competencies.
- Legal and ethical imperatives of medical practice can only be realized with full consideration in practice of biosocial pathogenesis and biographical (narrative) component of health and disease.
The modern idea of a disease as a situation, an event, increasingly includes the social side along with the biological one. Although the biomedical side of the problem still dominates, factors such as adherence, decision-making and informed consent or refusal, psychosocial aspects of etiology and pathogenesis and other non-biological disease components become part of care provision. Of course, the social side was predominant before the development of evidencebased medicine. But in the modern context, the development of the humanities and social sciences, as well as neuroscience and psychology, makes it possible to take into account the biographical narrative of the patient’s personality as an integral part of the doctor-patient relationship. At the intersection of "biological" and "biographical" in the disease nature there are a number of factors, such as loneliness, stress, emotions, that reify, enact a person’s social self into somatic pathology or somatic health. The problem of combining humanities and natural science knowledge is very complex due to the fundamental difference in the methods of study, but for modern medicine such a connection is absolutely necessary.
MODERN SCIENTIFIC TECHNOLOGIES
- Models of relationships between the ascending aorta parameters and other signs, built using machine learning, can be used for choosing a treatment method and the scope of intervention for ascending aortic aneurysm.
- In aortic regurgitation, a more aggressive approach to surgical correction of ascending aortic dilation is warranted.
- To predict the aortopathy course, thoracic aorta diameters indexed to body surface area should not be used.
- Aortic wall sampling (circular section), followed by a continuous pathological examination and subsequent prospective follow-up, may be promising.
Aim. To assess the association between pathological ascending aortic (AA) wall changes and its planimetric characteristics in non-syndromic non-familial (sporadic) aneurysm and dilation of the AA.
Material and methods. The study included 174 patients with sporadic aneurysms and dilation of the AA, who underwent elective surgery between January 2010 and July 2015 and were divided into 2 groups: patients with AA aneurysm (AAA) (AA diameter >50 mm) and tricuspid aortic valve (AV) with significant aortic stenosis (AS) or regurgitation (AR) (AAA group, n=120), and persons with borderline AA dilatation (AA diameter 45-50 mm), associated with a bicuspid aortic valve (BAV) and significant AS (BD group, n=54). Standard paraclinical investigations and pathological examination of the VA wall were used. Statistical processing was carried out in the SPYDER 4.1.5 environment (Python 3.8), and included univariate correlation analysis, logistic regression analysis, as well as supervised machine learning (ML) methods (support vector machine, k-nearest neighbor method, random forest).
Results. Logistic regression revealed positive associations between AA atherosclerosis and age, cystic medial necrosis (CMN) and sinus of Valsalva (SV) diameters. The support vector machine method demonstrated a tendency towards AA expansion at the SV level in individuals with CMN (accuracy, 60,5%), as well as towards expansion of the tubular AA in atherosclerosis (accuracy, 79,2%). During the random forest analysis, the first stage was to construct decision trees to predict three following outcomes: the presence of CMN, atherosclerosis, or normal aortic structure. The model accuracy was 64,2%. Next, the variables "CMN" and "atherosclerosis" were combined, and prediction was made for the outcomes "normal AA wall structure" and "pathological AA wall structure". The model accuracy was 73,5%.
Conclusion. The use of ML opens up new opportunities for predicting aortopathy and a patient-centered approach to treatment. In AR, a more aggressive AA intervention is warranted. To predict aortopathies, thoracic aorta diameters indexed to body surface area should not be used. Aortic wall sampling (circular section) followed by a continuous pathological examination may be promising.
GUIDELINES FOR THE PRACTITIONER
- Patients with hypertension and multiple risk factors are more difficult to respond to antihypertensive therapy (AHT), even in the form of a triple freedose combination.
- Increasing the AHT effectiveness by prescribing a triple fixed-dose combination of amlodipine/ indapamide/perindopril (Triplixam) after 3 months of treatment ensures achievement of the target blood pressure in the vast majority of patients and an improvement in 24-hour blood pressure monitoring.
- Triple fixed-dose combination of amlodipine/ indapamide/perindopril has pronounced cardioand vasoprotective effects, which are ref lected in the regression of left ventricular hypertrophy, improvement of its diastolic function and reduction of arterial stiffness.
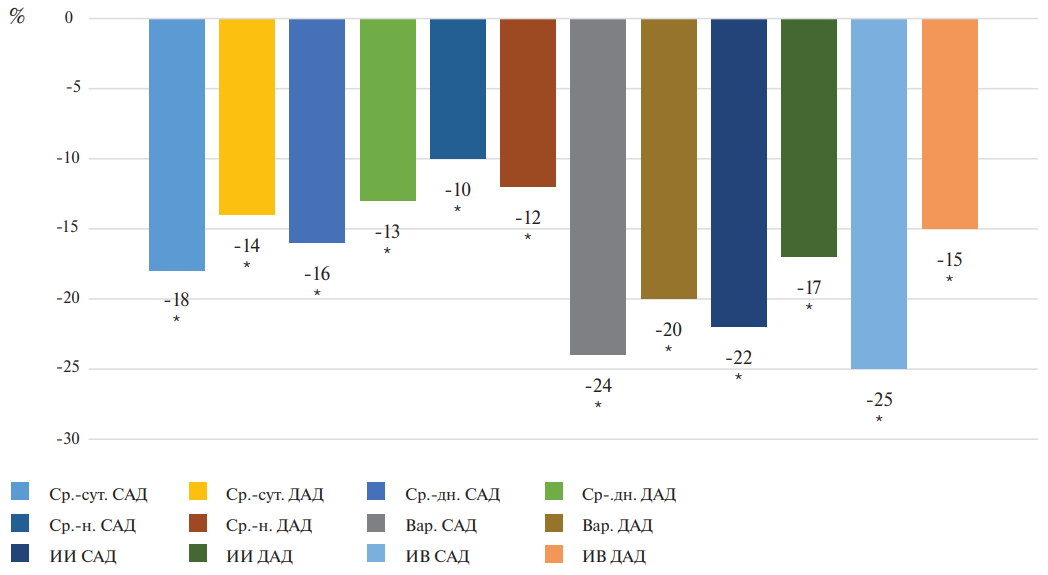
Aim. To evaluate the antihypertensive and organ protective efficacy of the triple fixed-dose combination of amlodipine/indapamide/perindopril in patients with hypertension (HTN) who did not achieve target blood pressure (BP) on previous antihypertensive therapy (AHT).
Material and methods. The study included 47 patients with HTN and multiple risk factors who did not achieve target blood pressure during previous AHT. They were prescribed triple fixed-dose combination of amlodipine/indapamide/perindopril with preliminary prescription of amlodipine, indapamide and perindopril in the free-dose combination. At baseline and after 3 months of AHT, 24-hour ambulatory blood pressure monitoring (ABPM), echocardiography and arterial stiffness were analyzed.
Results. Initially, in patients included in the study, the main ABPM parameters were increased, while non dipper and reduced dipper (66% of patients) patterns prevailed. The results of echocardiography indicated left ventricular (LV) hypertrophy (LVH) by left ventricular mass index (LVMI), left ventricular posterior wall thickness (LVPWT), interventricular septum (IVS) and its diastolic dysfunction by E/A, while an increase in CAVI and biological vascular age reflected an increase in arterial stiffness. After 3 months of AHT, significant (p£0,05) ABPM changes and a predominance of the dipper-type 24-hour BP pattern were recorded in more than half of the patients (53%). A decrease in LVMI, LVPWT and IVS by 7%, 12% and 8%, respectively (p£0,05), while an E/A increase by 12% reflected LVH regression and LV diastolic function improvement. A decrease in arterial stiffness was evidenced by a decrease (p£0,05) in CAVI by an average of 10% and biological vascular age by 4 years.
Conclusion. Triple fixed-dose therapy of amlodipine/indapamide/perindopril after 3-month treatment made it possible to achieve target blood pressure in 78% of patients, improved ABPM parameters and ensured pronounced cardioand vasoprotective effects, reflected in LVH regression, improvement of LV diastolic function and reduction of arterial stiffness.
ISSN 2618-7620 (Online)