МЕТАБОЛИЧЕСКОЕ ЗДОРОВЬЕ
- The global overweight and obesity pandemic has led to a significant increase in related metabolic diseases, such as glucose metabolism disorders and type 2 diabetes, dyslipidemia and atherosclerotic cardiovascular diseases, hypertension, metabolic-associated fatty liver disease, renal diseases and many other.
- The metabolic health of the population is determined by the prevalence of overweight, obesity and related diseases.
- Treatment of patients with obesity and metabolic diseases presents management and professional difficulties, as it requires trained specialists in the field of cardiometabolic medicine, which goes beyond the scope of traditional training.
- Training of cardiometabolic medicine specialists and the opening of specialized centers/offices should become one of the priorities of modern medicine.
Studying the metabolic health of population around the world is becoming a priority area of modern medicine. This is associated with an increase in the prevalence of overweight and obesity, which leads to a significant increase in related metabolic diseases, which are actually complications of obesity, primarily visceral. According to 2019 data, overweight and obesity are associated with 5 million deaths and 160 million disability-adjusted life years, more than half of which are due to cardiovascular diseases. This challenge requires the development of cardiometabolic medicine and the training of new specialists.
- Metabolic syndrome increases the risk of recurrent atrial fibrillation after elective electrical cardioversion.
- Among the indicators characterizing obesity, high epicardial fat thickness is the most significant predictor of failure to maintain sinus rhythm after cardioversion.
- Threshold values for galectin-3 and interleukin-6 have been established to predict atrial fibrillation recurrence in patients with metabolic syndrome within 6 months.
Aim. To evaluate the effect of blood concentrations of biomarkers of inflammation and fibrosis, obesity parameters, and parameters characterizing cardiac remodeling on the risk of recurrent atrial fibrillation (AF) within 6 months after elective electrical cardioversion (ECV) in patients with metabolic syndrome (MS).
Materials and methods. The study included patients with AF and MS (n=60) and with AF without MS (n=41), who underwent elective ECV. Prospective observation was carried out for 6 months.
Results. Arrhythmia recurrence within 6 months after ECV in patients with AF in combination with MS is higher than without MS (34/60 and 9/41, p = 0.003). Among echocardiographic parameters, left atrial volume and volume index, and epicardial adipose tissue thickness (EAT) are associated with arrhythmia resumption in patients with MS and AF. Blood concentrations of galectin-3 (17.4 (12.8-19.6) and 13.3 (5.1-14.9), p=0.0001), connective tissue growth factor (CTGF) (163, 1 (134.1-232.2) and 156.7 (104.7 - 189.1), p=0.002), growth differentiation factor 15 (GDF-15) (2343.9 (1206.1-3254.2 ) and 986.1 (812.5-1775.5), p=0.0001) and interleukin-6 (IL-6) (3.8 (2.3-7.3) and 2.3 (1, 3-3.4), p=0001) in patients with MS with recurrent arrhythmia is higher than without arrhythmia. According to the ROC analysis of EAT, the concentration of galectin-3 and IL-6 in the blood was most predictive of relapse of AF in MS; threshold values of the predictors were established: EAT more than 6.1 mm, IL-6 more than 2.8 pg/ml, galectin-3 more than 15.9 ng/ml.
Conclusion. In patients with AF combined with MS, the frequency of maintaining sinus rhythm after effective ECV for 6 months is lower than in patients without MS. Epicardial adipose tissue thickness, high concentrations of galectin-3 and IL-6 are associated with relapse of AF in patients with MS.
- In patients with gout, an unfavorable obesity phenotype is characterized by a more severe clinical course of the disease, hyperinsulinemia, increased serum levels of retinol-binding protein 4 (RBP4), visfatin, and atherogenic dyslipidemia.
- In men with gout, regardless of obesity phenotype, omentin-1 deficiency may contribute to insulin resistance and dyslipidemia progression.
- Liraglutide therapy in gout patients with a metabolically unhealthy obesity promotes weight loss by 11,0±5,7%, an improvement in the adipocytokine profile with an omentin-1 increase, a decrease in the of RBP4 and uric acid serum level.
Aim. To study the serum level of retinol-binding protein 4 (RBP4), visfatin, omentin-1 and vaspin in gout patients with different obesity phenotypes, as well as to assess the dynamics of studied parameters against the background of weight loss using an analog of glucagon-like peptide-1 (GLP-1) liraglutide.
Material and methods. A total of 117 men with gout during the attack-free interval were examined. The patients were divided into 2 following groups: the 1st group consisted of 43 patients with a metabolically healthy obesity (MHO) and body mass index (BMI) ≥30 kg/m2; the second group consisted of 74 people with an metabolically unhealthy obesity (MUO) (carbohydrate metabolism disorders, hypertension (HTN) and BMI ≥30 kg/m2). The control group was represented by 38 respondents with a class 1 MHO. The blood concentrations of RBP4, omentin-1, visfatin, vaspin, serum uric acid, high-sensitivity C-reactive protein (hsCRP), HOMA-IR, anthropometric parameters were studied at the enrollment and 12 weeks later on the background of liraglutide therapy.
Results. In gout patients with obesity, an increase in RBP4 and visfatin levels was revealed with a simultaneous decrease in omentin-1 and vaspin compared with patients in the control group and patients with gout with no metabolic disorders. The interrelationships of RBP4 and omentin-1 with the following metabolic syndrome components were established: BMI, increased triglycerides (TGs), increased total cholesterol, hsCRP, HOMA-IR and hyperinsulinemia, and reduced vaspin levels showed only a positive relationship with the HDL-C concentration (p<0,05). Visfatin positively correlates with diastolic blood pressure (r=0,29, p<0,01), the number of involved joints (r=0,577, p<0,01), the number of gout attacks (r=0,63, p<0,001).
Conclusion. RBP4 and omentin-1 correlate with BMI and increased insulin sensitivity, whereas visfatin demonstrates an association with hyperuricemia and severity of gouty arthritis. Liraglutide therapy contributes to weight loss by 11,0±5,7%, improves the metabolic profile of patients with gout, increasing the content of omentin-1, lowering the RBP4 and uric acid serum concentration.
- Non-alcoholic fatty liver disease (NAFLD) is not a traditional risk factor for the progression of cardiovascular diseases, but recent studies demonstrate its role in the cardiovascular disease progression.
- NAFLD is associated with factors influencing the coronary artery disease course — hyperglycemia, lipid metabolism disorders, as well as ultrasound markers of obesity.
- The study showed that 52,5% of people with a normal body mass index had NAFLD, which once again indicates its ineffectiveness for stratifying the risk of development and progression of cardiovascular disease and the need for routine screening of NAFLD in people with cardiovascular diseases, regardless of body mass index.
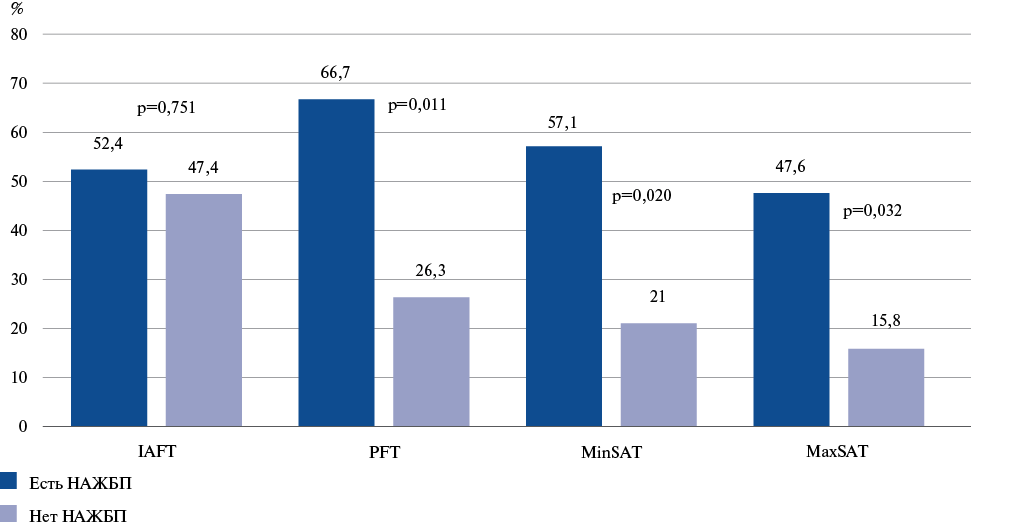
Aim. To evaluate the association of non-alcoholic fatty liver disease (NAFLD) with markers of visceral obesity in patients with coronary artery disease (CAD).
Material and methods. We examined 125 patients hospitalized in the emergency cardiology department with CAD (female — 41,6%, male — 58,4%) and body mass index of 18,5-35,0 kg/m2. The median age of the subjects was 68 [61,0;74,0] years. We assessed following ultrasound parameters of visceral obesity: intraabdominal fat thickness (IAFT), abdominal wall fat index (WFI), preperitoneal fat thickness (PFT), subcutaneous adipose tissue (SAT), represented by MinSAT and MaxSAT. The following liver parameters were assessed: anteroposterior dimension of the left lobe and oblique-vertical dimension of the right lobe. Statistical data processing was carried out using the Statistica 6.0 program. Quantitative variables are presented as median (Me). Percentiles (25%; 75%) were used as dispersion measures. The influence of several predictors was assessed using linear regression analysis.
Results. In patients without echographic signs of hepatic steatosis, the IAFT was 50,5 [30,7;65,0] mm and significantly increased with increasing hepatosis degree: from 45,0 [24,0;63,0] mm in respondents with grade 1 to 67,5 [34,0;76,0] mm with grade 3 (p=0,010). PFT also significantly increased from 11,5 [8,9;13,3] mm in individuals without hepatic steatosis to 13,8 [10,7;15,6] mm in those with grade 1, 18,5 [13,0;22,4] mm in those with grade 2 and 23,5 [13,0;29,4] mm in those with grade 3 hepatic steatosis (p=0,001). MinSAT and MaxSAT also increased, but not significantly (from 11,5 [8,8;15,9] to 20,4 [10,1;27,3] mm, p=0,151 and from 14,0 [11,4;25,4] mm to 22,4 [15,0;25,0] mm, p=0,576, respectively). The increase in WFI was also not significant. Linear regression analysis confirmed that hepatic steatosis was associated with IAFT increase (b=9,3, p=0,012).
Conclusion. NAFLD is associated with factors influencing the CAD course — hyperglycemia, lipid metabolism disorders, as well as ultrasound markers of obesity. An increase in liver size was associated with an increase in BMI, glucose, triglycerides, high-density lipoproteins and ultrasound markers of obesity — IAFT and PFT. NAFLD in patients with CAD was associated with increased IAFT and PFT. In addition, 52,5% of people with normal body weight had NAFLD, which once again indicates the ineffectiveness of this indicator for stratifying the risk of development and progression of cardiovascular disease and the need for routine screening of NAFLD in people with cardiovascular diseases, regardless of BMI.
- Cardio-ankle vascular index decrease in young people, combined with normal ankle-brachial index, with an increase in body weight, indicates the need for a differentiated approach at this age to assess the status of the inner and middle arterial wall layer under the influence of cardiovascular risk factors.
- Novel diagnostic approaches based on angiological screening allowing simultaneous assessment of the status of different vascular wall structures should be introduced into youth preventive measures.
Aim. To assess functional parameters of the middle and inner arterial wall layers in relation to body mass index (BMI) in young people from the perspective of their vascular aging phenotype and sex.
Material and methods. A total of 264 young people (93 boys) aged from 18 to 25 years (21,4±1,3) were examined. In three groups formed according to BMI, cardio-ankle vascular index (CAVI) and ankle-brachial index (ABI), as well as the main parameters of hemodynamic and metabolic status were determined. Angiological screening aimed at assessing vascular stiffness (VS) and blood pressure (BP) in the vascular beds was performed using a VaSera VS-1500 system ("Fukuda Denshi", Japan). The subjects were divided into tertile CAVI groups based on sex to identify carriers of early, normal and favorable vascular aging phenotypes.
Results. As body weight increases in young people, a tendency towards a CAVI decrease was revealed without significant changes in the ABI. In boys, CAVI-R decreased on average by 26,4% (p=0,000) and CAVI-L — by 25,9% (p=0,000). In girls, the decrease was less pronounced. But the latter showed a significant positive relationship between BMI and systolic BP, diastolic BP, low-density lipoproteins, triglycerides, atherogenicity coefficient, as well as a significant negative relationship with high-density lipoproteins. In young men, no significant relationship was found between BMI and any hemodynamic and metabolic parameters. More than half of the overweight boys and girls were carriers of favorable vascular aging phenotype, and among them, the majority noted problems with excess weight either in middle and high school or during student years. In addition, 12,0% of overweight boys and 26,3% of the same girls were characterized by early vascular aging. The vast majority of them were distinguished by excess body weight starting from early childhood.
Conclusion. In young people aged 18 to 25 years (21,4±1,3), a VS decrease was revealed against the background of BMI increase. This phenomenon is more typical for carriers of recent obesity. The identified phenomenon, caused by an adaptive mechanism, may be called the youth obesity paradox and it should be taken into account when carrying out preventive measures among young people.
- We established that masked uncontrolled hypertension (HTN) occurs in 18,4% of patients with impaired carbohydrate metabolism.
- The comparability of 24-hour peripheral and aortic pressure values in individuals with masked uncontrolled and resistant uncontrolled hypertension has been demonstrated.
- A higher incidence of target organ damage has been established in patients with masked uncontrolled HTN compared with controlled HTN, which determines the prognostic significance of this phenotype.
Aim. To establish the prevalence of masked uncontrolled hypertension (HTN) (MUH) in patients with diabetes or impaired glucose tolerance (IGT) and determine its clinical and hemodynamic characteristics.
Material and methods. The study involved 87 patients who received regular antihypertensive therapy for hypertension and had established diabetes or IGT. The mean age of patients was 62,6±9,9 years, of which 51,7% were women, 48,3% — men. Type 2 diabetes was revealed in 77,7%, IGT — 22,8% of patients. For 24-hour blood pressure monitoring, BpLAB system (OOO Petr Telegin) was used; blood pressure (BP) was determined in the brachial artery, central blood pressure — in the aorta. We analyzed risk factors and target organ damage. The results were processed using the Excel Microsoft Office 2007 package and the Statistica 6.0 and 10.0 package from StatSoft, Inc (USA).
Results. Uncontrolled hypertension was revealed in 59,8%, MUH — in 18,4%, controlled HTN — 21,8% of patients. Mean daytime and mean nighttime systolic BP in patients with MUH and uncontrolled HTN were comparable. Patients with controlled hypertension compared with MUH had lower mean day- and nighttime aortic BP by 27,1% (p<0,01) and 16,8% (p<0,01), respectively. Aortic BP was comparable in individuals with MUH and uncontrolled HTN. Asymptomatic hyperuricemia was more common in patients with uncontrolled HTN compared with MUH and controlled hypertension by 29,3% and 41,8%, respectively. With MUH, compared with controlled HTN, we revealed a higher incidence of stroke by 18,8%, a decrease in glomerular filtration rate <60 ml/min by 17,5%, albuminuria by 18,8%, left ventricular hypertrophy by 2,6 times.
Conclusion. Only 41,2% of patients with diabetes and prediabetes achieve the target office BP level, while every second of these patients has MUH. MUH, compared with controlled HTN, is characterized by a higher incidence of stroke, kidney (decrease in glomerular filtration rate <60 ml/min and albuminuria) and heart damage (left ventricular hypertrophy).
- An increase in body mass index (BMI) is associated with an increase in the incidence of atrial fibrillation (AF). Visceral adipose tissue (VAT) is associated with a higher cardiovascular risk profile compared with BMI.
- In hypertensive patients with and without AF at comparable levels of BMI and VAT, differences in epicardial adipose tissue (EAT) thickness were identified. EAT thickness was significantly higher in patients with AF compared to patients without AF. In addition, univariate model of the AF risk revealed that the EAT depot is more significant than the VAT depot and BMI in predicting the AF risk.
- EAT determination can be useful in identifying individuals in whom AF is associated with obesity, as well as groups at risk of AF and timely initiation of AF prevention, including through weight loss using non-pharmacological and pharmacological approaches.
Aim. To evaluate the value of body mass index (BMI), visceral adipose tissue (VAT) and epicardial adipose tissue (EAT) depots in the development of atrial fibrillation (AF).
Material and methods. The study included 24 people with isolated hypertension (HTN) and 28 people with HTN in combination with AF. The median age of patients was 61,5 [53,8;69,0] years. The observational study assessed height, weight, BMI, proportion of VAT, EAT thickness, and cardiac chamber sizes. Height was measured using a metal height meter Rm-1 "Diakoms"; the results were expressed in centimeters. Weight, BMI, and VAT proportion were measured using an Omron BF-508 body composition monitor (Omron, Japan). EAT thickness and cardiac chamber sizes were assessed using two-dimensional echocardiography. Univariate logistic regression models were used to assess the independent contribution of the identified factors associated with the disease presence.
Results. Hypertensive patients with and without AF were comparable in terms of BMI and VAT content. At the same time, the EAT content was significantly higher in the group of patients with HTN and AF and amounted to 7,0 [5,0;8,2] mm and 6,0 [4,5;7,0] mm (p=0,027) in the group HTN with and without AF, respectively.
Left atrial (LA) volume was 70 [55,2;83,0] ml and 52 [45,5;59,0] ml (p=0,003) in the hypertensive group with and without AF, respectively. Univariate analysis revealed the greatest significance of EAT and LA volume in terms of AF prediction. Logistic regression models did not reveal significant effect of VAT.
Conclusion. In hypertensive patients with and without AF at comparable levels of BMI and VAT, differences in EAT thickness and LA volume were identified. Univariate analysis showed that these factors have an advantage in the development of AF. However, even despite the limited sample, the EAT depot was found to be more significant than the VAT depot and BMI in predicting the AF risk.
The data that EAT depot and LA volume have the same effect on the arrhythmia risk indicates that patients with AF should be treated not only for hypertension, but also hidden obesity, which we can judge by EAT thickness.
- Patients with stable CAD with borderline stenosis and increased epicardial fat thickness (EFT) have a higher incidence of early vascular aging compared with patients without increased EFT.
Aim. To evaluate the incidence of early vascular aging (EVA) and epicardial fat thickness (EFT) in patients with stable coronary artery disease (CAD) with borderline stenosis.
Material and methods. The study involved 201 patients with class 1-3 stable CAD with borderline (50-70%) stenosis. The first group consisted of 57 (28,4%) patients with increased EFT, the second (n=144 (71,6%)) — without increased EFT. EFT was determined by cardiac ultrasound. Vascular wall stiffness was assessed using a VaSera VS-1500N sphygmomanometer manufactured by FUKUDA DENSHI (Japan). Relative telomere length was determined by real-time PCR. All patients underwent coronary angiography.
Results. The mean EFT in group 1 was 6,00 [5,00; 6,50] mm, in group 2 — 3,00 [2,30; 4,00] mm (p<0,001). In patients of group 1, hypertension (p<0,001), CAD (p<0,001) in general and myocardial infarction (p=0,003) in particular debuted at a younger age. In both groups, the incidence of obesity, type 2 diabetes, angina, and the intake rate of all four main groups of antianginal drugs did not differ significantly. Early vascular aging was significantly more often detected in the group of patients with stable CAD with borderline coronary artery stenosis and visceral obesity (p<0,001). Relative telomere length was shorter and pulse wave velocity was higher in this group (p<0,001).
Conclusion. Patients with stable CAD with borderline stenosis and increased EFT have a higher incidence of EVA, despite the same incidence of obesity, diabetes, and functional class of angina as the group of patients without increased EFT.
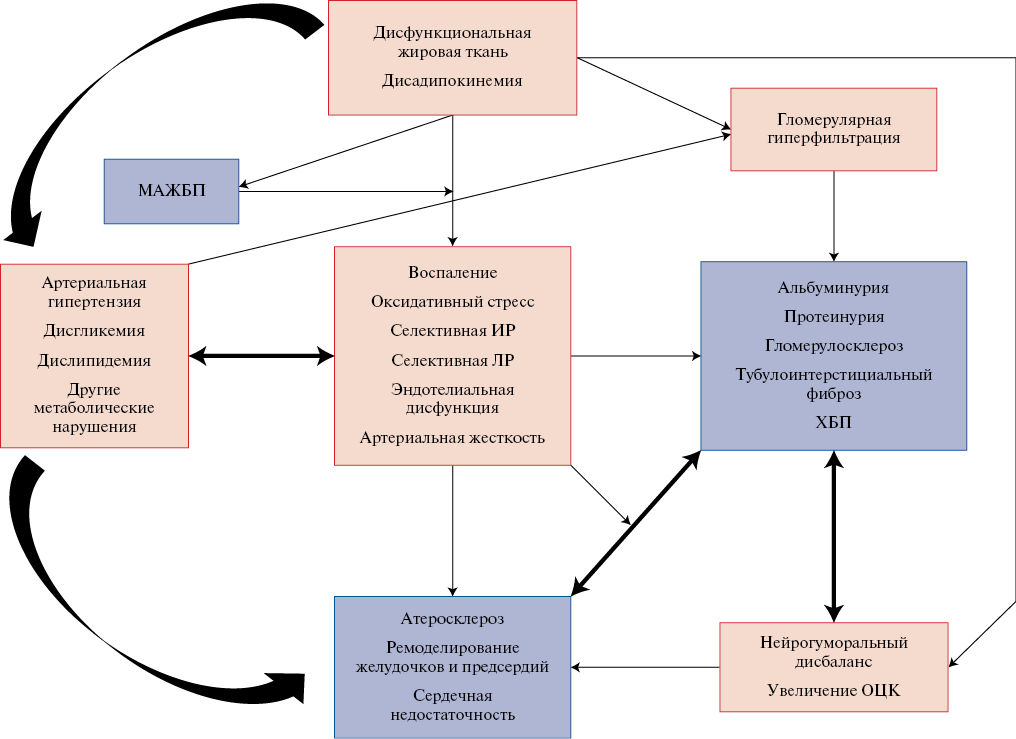
- The combination of metabolic risk factors and chronic kidney disease within the cardiovascular-kidney-metabolic syndrome has been shown to be closely associated with the risk of adverse cardiovascular and renal outcomes.
- The pathogenesis of this syndrome is presented and its clinical and laboratory classification is proposed, highlighting the development stages and an effective approach to therapy.
- Risk algorithms that reflect the multiple adverse cardiovascular and renal outcomes that are common in patients with cardiovascular-kidney-metabolic syndrome can help better target therapy to proper subpopulations.
In 2023, the American Heart Association for the first time formally defined cardiovascular-kidney-metabolic (CKM) syndrome as a systemic disease characterized by pathophysiological interactions between metabolic risk factors, chronic kidney disease (CKD), and cardiovascular system, leading to multiple organ dysfunction and a common adverse cardiovascular outcomes. Data are presented based on the pathophysiological mechanisms and clinical manifestations that made it possible to define this syndrome through the interaction between metabolic risk factors, CKD and the cardiovascular system, leading to multiple organ dysfunction and a high level of adverse cardiovascular outcomes. A classification of this syndrome into stages has been determined, for each of which approaches to the diagnosis and management of patients have been defined. CKM syndrome reflects the influence of multisystem pathophysiological relationships embedded in a multi-level socially and clinically determined community of manifestations, the fusion of which specifies clinical outcomes.
ARTERIAL HYPERTENSION
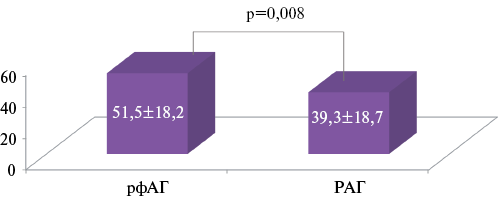
- The role of the sympathetic nervous system in increasing the level of β-adrenergic reactivity of erythrocyte membranes (EM) in patients with various uncontrolled hypertension phenotypes is considered.
- Patients with refractory hypertension (rfHTN) have higher levels of β-adrenergic reactivity compared to patients with resistant hypertension (rHTN).
- Increased EM β-adrenergic reactivity levels are associated with increased pulse pressure in patients with rfHTN, which may explain the higher incidence of left ventricular hypertrophy compared with patients with rHTN.
Aim. To assess the functional state of the sympathetic nervous system according to β-adrenergic reactivity of erythrocyte membranes (EM) in patients with refractory (rfHTN) and resistant hypertension (rHTN) in relation to target organ damage.
Material and methods. The cross-sectional comparative study included 78 patients with uncontrolled hypertension (mean age, 57,4±9,3 years (33 men)) with 24-hour blood pressure (BP) (systolic/diastolic) of 160,0±18,8/88,1±17,3 mm Hg. Thirty-nine (50%) patients had type 2 diabetes (T2D). At baseline, patients were divided into 2 groups depending on the phenotype of uncontrolled hypertension. The first group consisted of patients with rfHTN (n=26 (33,3%)), the second — with rHTN (uncontrolled BP with 3-4 agent therapy) (n=52 (66,7%)). In all patients, office and mean 24-hour blood pressure, EM β-adrenergic reactivity and target organ damage were assessed.
Results. The compared groups did not differ in sex and age composition, prevalence of T2D and basic clinical data. However, despite comparable levels of office and mean 24-hour blood pressure, the incidence of left ventricular (LV) hypertrophy according to echocardiography in rfHTN was significantly higher than in rHTN (96,2% vs 76,9%, p=0,027, respectively). An increase in EM β-adrenergic reactivity (>20 conventional units) was documented in 87,1% of patients in the general group. Moreover, the mean EM β-adrenergic reactivity in the rfHTN group was significantly higher than in the rHTN group (51,5±18,7 vs 39,3±18,2, p=0,008). According to ROC analysis, the threshold value of EM β-adrenergic reactivity corresponding to rfHTN was ≥44,8 conventional units (sensitivity — 69,2%, specificity — 64,5%, area under the ROC curve — 0,687). The mean EM β-adrenergic reactivity in the rfHTN group did not have a direct relationship with the LV mass index, but correlated with increased pulse pressure.
Conclusion. RfHTN is associated with higher EM β-adrenergic reactivity values than in patients with rHTN, which may indirectly confirm more pronounced sympathetic activity and explain the higher prevalence of LVH, realized through an increase in vascular stiffness and load on the LV.
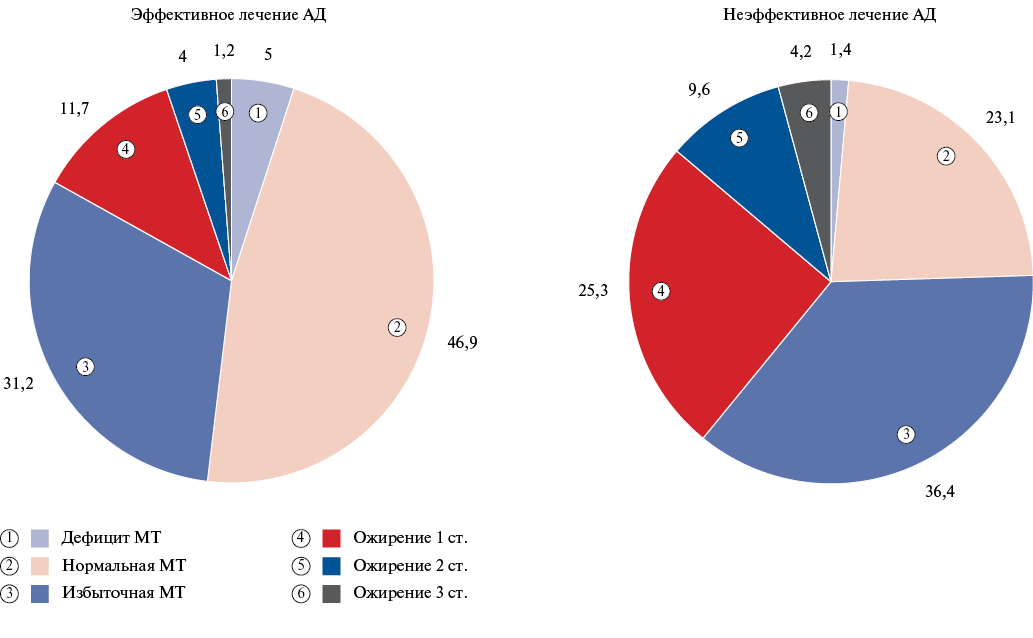
Aim. To assess awareness of blood pressure (BP) level, adherence to therapy and achievement of target BP in residents of Russian regions as part of the 2023 hypertension (HTN) screening campaign.
Material and methods. During May 2023, 4613 participants from 23 cities of Russia took part in the screening. Participation was voluntary without restrictions on sex. All patients aged over 18 years. During screening, BP and pulse were measured three times using automatic or mechanical BP monitors, and a questionnaire about behavioral risk factors, concomitant diseases and therapy was filled out. HTN was diagnosed with systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg and/or taking antihypertensive therapy (AHT).
Results. The analysis included data from 4585 respondents aged 18 to 95 years with an average age of 45 [28;59] years, of which 1729 were men (37,7%). The proportion of hypertensive patients was 49,6%. Among them, 62,8% took AHT and achieved target BP in 76,6% and 45,7% with the target BP criterion <140/90 mm Hg and <130/80 mm Hg, respectively. Most patients took dual AHT (37,4%), while monotherapy and triple therapy was registered in 27,5% and 23,4%, respectively. Initiation of therapy was performed with combination AHT in 43,7% of patients with HTN and 41,4% are currently using fixed-dose combination therapy. On-demand therapy was the most common reason for skipping medications and was more common in women, while men more often cited the high drug cost and a history of adverse reactions. Among patients with HTN, home BP measurement was associated with a higher prevalence of achieving target BP as follows: 1000 (60%) vs 100 (17%), p<0,001.
Conclusion. The data obtained indicate, on the one hand, a continuing insufficient level of awareness about high BP and the use of antihypertensive drugs among the population, but there is a tendency to improve the effectiveness of the treatment of hypertension, including the use of fixed-dose combinations of antihypertensive drugs.
- The cardioprotective effect of renal denervation has been shown in patients with resistant hypertension in the form of left ventricular hypertrophy regression.
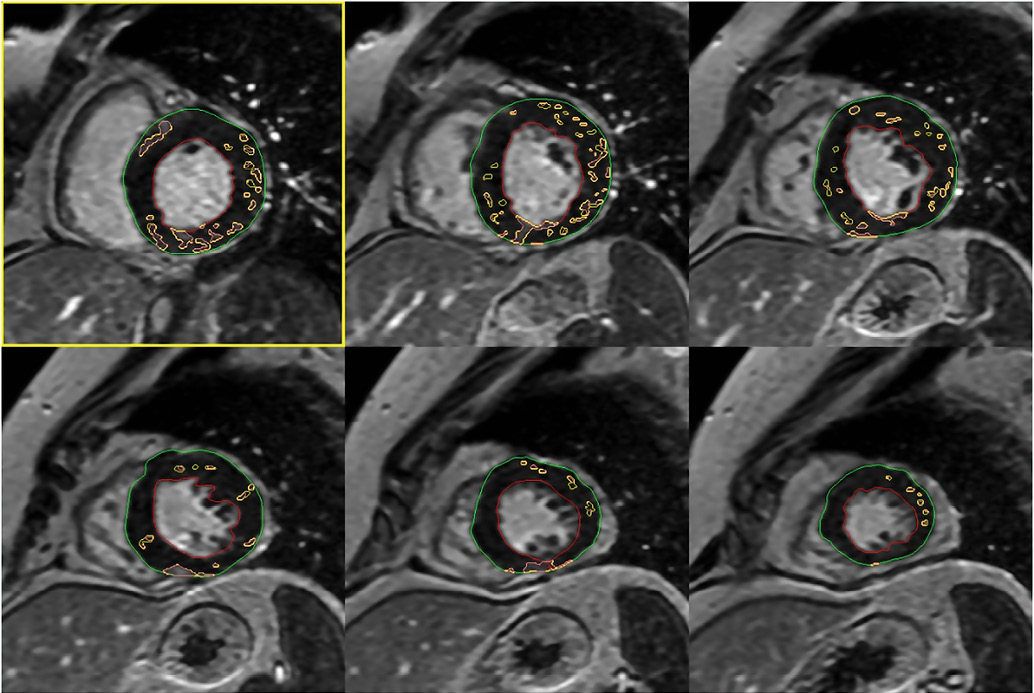
- No progression of cardiac fibrosis was revealed according to cardiac magnetic resonance imaging, associated with a decrease in blood pressure and a decrease in collagen production.
Aim. To study the features of regression of left ventricular hypertrophy and magnetic resonance changes of cardiac fibrosis in patients with resistant hypertension (RH) 1 year after renal denervation (RDN) in relation to changes in blood pressure (BP), the level of high-sensitivity C-reactive protein (hsCRP), matrix metalloproteinases 2, 9 (MMP-2, MMP-9), tissue inhibitor of metalloproteinase type 1 (TIMP-1).
Material and methods. The study included 42 patients with true RH. The mean age of the patients was 59 (51; 62) years, while half were men. All patients took 3 or more antihypertensive drugs. At baseline and after 12 months, creatinine, hsCRP, MMP-2, MMP-9, TIMP-1 were determined, as well as 24-hour blood pressure monitoring, assessment of left ventricular mass (LVM) and contrast agent accumulation according to cardiac MRI. RDN was performed using Symplicity Fleх (n=18) and Symplicity Spyral (n=24) catheters in accordance with the manufacturer's instructions.
Results. A year after RDN, a significant antihypertensive effect and a decrease in heart rate were noted. Sixteen patients (38,1%) reached the target office BP level. After 1 year, a significant decrease in the levels of hsCRP from 2,05 (1,04; 3,28) to 1,64 (0,96; 2,25) mg/l (p=0,045) and MMP-2 from 278,2 (240,9; 353,4) to 265,2 (221,2; 293,2) ng/ml (p=0,018) was detected. There was a trend towards an increase in TIMP-1 and a decrease in MMP-9. According to MRI 1 year after RDN, there was a tendency to increase the contrast agent volume, and there was a pronounced LVM decrease from 228 (180; 295,2) to 204 (169,8; 277) g (p=0,029). Correlation analysis revealed a direct connection between a decrease in LVM and a decrease in SBP and DBP levels, MMP-2 and MMP-9 levels. There was a relationship between a decrease in the contrast agent volume and an increase in TIMP-1 level (r=-0,64; p=0,04).
Conclusion. A year after RDN, patients with RH show regression of left ventricular hypertrophy with a pronounced antihypertensive effect and a decrease in collagen production, which could also be significant for suppressing the myocardial fibrosis.
Arterial stiffness, as a marker of subclinical target organ damage in patients with hypertension (HTN), is an important and independent predictor of mortality and cardiovascular morbidity. The review examines factors contributing to increased vascular wall stiffness with a focus on smoking, pathogenesis of increased arterial stiffness with aging, and the effect of arterial stiffness on increased systolic and pulse pressure. Particular attention is paid to the effect of pulse pressure on the risk of cardiovascular events, primarily on the incidence of stroke and cognitive impairment. Thiazide-like diuretics and calcium antagonists have the greatest evidence base in HTN treatment in the elderly due to their ability to reduce systolic and pulse pressure, reduce arterial stiffness and have a positive effect on prognosis. The use of amlodipine/indapamide retard combination promotes more effective treatment of elderly patients with HTN.
ISSN 2618-7620 (Online)