OPINION ON THE ISSUE
An increased concentration of lipoprotein(a) (Lp(a)) is one of the main genetic residual risk factors for atherosclerotic cardiovascular diseases, as well as their complications. Lp(a) is a complex supramolecular complex in which the unique glycosylated apo(a) protein, which has a wide polymorphism, is linked by a disulfide bond to the apoB100 molecule (protein component of the low-density lipoprotein (LDL) particle). Therefore, Lp(a) is often called LDL-like particle. Unlike all other lipoproteins, Lp(a) concentration is determined genetically, almost constant throughout the life, and has wide individual and interethnic variability. As an independent risk factor, elevated Lp(a) concentrations can significantly increase global cardiovascular risk, especially in patients with other risk factors. Modern international and national guidelines recommend measuring Lp(a) concentration not only in certain categories of patients, but also in every person at least once in their life for a correct assessment of cardiovascular risk.
The article presents the up-to-date information on the effect of lipoprotein apheresis (LA) on atherosclerotic lesions. Some studies using modern diagnostic imaging techniques (such as intravascular ultrasound or magnetic resonance imaging) have clearly demonstrated plaque regression. Coronary angiography has also seen reversal or at least slow plaque progression. Plaque regression likely leads to a decrease in the incidence of atherosclerotic cardiovascular events (CVEs). However, this has not yet been fully proven. Recent data indicate that reduction in low-density lipoprotein cholesterol and lipoprotein(a) levels is not a major factor in reducing the incidence of atherosclerotic CVEs in patients undergoing extracorporeal treatment. The most significant risk factors in this case are older age and a greater CVE rate observed before the start of LA, as well as smoking. New studies using modern diagnostic imaging methods in patients receiving LA are necessary.
PROGNOSIS AND DIAGNOSTICS
- Special aspects of LEPRisoform expression in cardiac local fat depots in patients with coronary and non-coronary pathologies were revealed.
- Patients with coronary artery disease show a marked reduction in the expression of six LEPRisoforms in epicardial adipose tissue (EAT).
- Changes in LEPRexpression in EAT in patients with coronary pathology are associated with impaired adipogenesis, adipocyte hypertrophy, insulin resistance, increased proinflammatory factors, hyperleptinemia, and progression of atherosclerosis.
Aim. To evaluate the expression of leptin receptor isoforms in local fat depots in patients with coronary artery disease (CAD) and acquired heart defects (AHDs).
Material and methods. The study included 120 patients with CAD. The comparison group consisted of 96 patients with degenerative aortic stenosis (AS). Expression of six leptin receptor isoforms (LEPR1, LEPR2, LEPR2/2, LEPR3, LEPR3/2, LEPR4) was assessed using quantitative real-time polymerase chain reaction in subcutaneous (SAT), epicardial (EAT) and perivascular (PVAT) adipose tissue. Statistical processing was carried out using the Statistica 10.0 and SPSS 17.0 for Windows software package.
Results. In EAT, minimal expression of LEPR1, LEPR2, LEPR2/2, LEPR3, LEPR3/2, LEPR4 was detected relative to SAT and PVAT in the group of CAD patients. In patients with CAD, mRNA levels of six LEPR isoforms were lower than in patients with AS. In individuals with AHDs, a decrease in the expression of LEPR1, LEPR2, LEPR2/2, LEPR3, LEPR3/2, LEPR4 in SAT relative to EAT and PVAT was recorded. However, only the LEPR1 and LEPR2 isoforms were significantly lower in SAT in patients with AS when compared with patients with CAD. In PVAT, the maximum mRNA levels of six LEPR isoforms were found in both groups. There were no significant differences in LEPR1, LEPR2, LEPR2/2, LEPR3, LEPR3/2, LEPR4 expression between patients with CAD and AHDs.
Conclusion. Patients with CAD are characterized by a marked decrease in the expression of six LEPR isoforms in EAT. A decrease in the expression of studied LEPR isoforms in EAT is associated with impaired adipogenesis, adipocyte hypertrophy, insulin resistance, increased proinflammatory factors, hyperleptinemia, and progression of atherosclerosis. The identified features of EAT in patients with СФВ can probably have both local and systemic negative effects on the cardiovascular system.
- Patients with coronary atherosclerosis and insulin resistance (IR) have higher levels of GIP, GLP-1, IL-6, leptin and pancreatic polypeptide (PP).
- Patients with stable plaques and IR have higher levels of leptin and PP compared to patients without IR.
- Patients with IR and stable plaques have higher PYY compared to patients with IR and unstable plaques.
- PP is associated with IR in patients with unstable plaques.
Aim. To study the association of adipocytokine levels with insulin resistance (IR) and stable/unstable plaques in patients with coronary atherosclerosis.
Material and methods. This cross-sectional observational study included 109 men aged 38-79 years with class II-III stable angina pectoris without acute coronary syndrome (ACS), with coronary atherosclerosis verified by coronary angiography. Biochemical tests were carried out using the enzymatic method on a Konelab 30i analyzer at the Laboratory of Clinical Biochemical and Hormonal Studies of Internal Diseases of the Research Institute of Internal and Preventive Medicine — branch of the Federal Research Center Institute of Cytology and Genetics. All patients also underwent anthropometric examination.
Results. Patients with coronary atherosclerosis and IR had higher levels of GIP by 1,4 times (p=0,005), GLP-1 by 1,7 times (p=0,032), IL-6 by 3,2 times (p=0,017), leptin by 2,3 times (p=0,001) and pancreatic polypeptide (PP) by 1,9 times (p=0,006). In patients with stable plaques and IR, leptin was 2 times higher, and PP was 1,7 times higher, compared to patients without IR. In patients with unstable plaques and IR, leptin and PP levels are 5,1 and 1,7 times higher, respectively, compared to the group of patients without IR. In patients with IR and stable plaques, PYY was 1,5 times higher than in patients with IR and unstable plaques, while the adiponectin level was 1,9 times higher. Logistic regression analysis demonstrated that PP is associated with IR in patients with unstable plaques.
Conclusion. Patients with coronary atherosclerosis and IR had higher levels of GIP, GLP-1, IL-6, leptin and PP. Leptin and PP levels are higher in patients with both stable and unstable plaques and IR, and PYY and adiponectin levels are higher in patients with stable plaques and IR compared with patients without IR. PP is associated with IR in patients with unstable plaques.
- The concentration of cell-free DNA (cfDNA) in patients with ST-segment elevation acute coronary syndrome (STE-ACS) compared to healthy volunteers was higher and significantly different.
- Percutaneous coronary intervention did not significantly affect serum cfDNA values.
- CfDNA level was independently associated with ulcerated plaque length in the infarct-related artery and myocardial infarct size in patients with STE-ACS.
Aim. To evaluate the changes of cell-free DNA (cfDNA) levels before and after percutaneous coronary intervention (PCI) in patients with ST-segment elevation acute coronary syndrome (STE-ACS). To identify associations of cfDNA concentration before and after PCI with complications and length of ulcerated plaque in patients with STE-ACS.
Material and methods. This prospective single-center observational pilot study included 44 patients with STE-ACS admitted to the cardiac intensive care unit during the period of May-August 2023. In all patients, along with standard laboratory tests, cfDNA level was measured upon admission and 24 hours after PCI. Assessment of cfDNA associations before and after PCI was carried out in relation to following significant complications and conditions in STE-ACS patients: death, acute left ventricular failure (ALVF), acute heart failure (AHF), arrhythmia, number of stents implanted, number of segments with impaired local contractility, total stent length.
Results. The mean age of the patients was 60,6±9,6 years, of which 74,6% were men. TIMI 0-1 flow was recorded in 93,2% of the subjects. The most common complications were cardiogenic shock (18,4%), arrhythmia (16,9%), AHF (13,6%), ALV (11,9%). Death was recorded in 8,5%. Implantation of 1 stent in PCI was performed in 75% of cases, while in the rest, 2 or more stents were implanted. The proportion of patients with impaired local contractility was 90%, the median stent length was 24,0 (20,0-50,0) mm. CfDNA level on admission did not differ from level after PCI 94,5 (78,3-155,5) ng/ml vs 115,0 (71,0-152,0), p=0,46. However, it significantly exceeded the cfDNA concentration from a group of healthy volunteers (78,0 (59,7-106,0), p=0,017). Characteristic curve showed significant relationships both for the concentration of cfDNA before (with implantation of 2 or more stents (AUC 0,71 with 95% confidence interval (CI) 0,56-0,86, p=0,039), stent length >24 mm (AUC 0,73 with 95% CI 0,58-0,89, p=0,009)) and after PCI (with the number of impaired local contractility segments (AUC 0,73 with 95% CI 0,57-0,89, p=0,014)). If the cfDNA level before PCI was >90 ng/ml, the risk of implantation of 2 or more stents per procedure increased by 5,4 times (odds ratio (OR) 5,4, 95% CI 1,11-28,93, p=0,044). The risk of a stent length >24 mm with pre-PCI cfDNA >107 ng/ml increased 9-fold (OR 9,0 with 95% CI 2,2-36,9, p=0,001), and the cfDNA level after PCI >105 ng/ml increased the risk of impaired local left ventricular (LV) contractility in 2 or more segments by 5 times (OR 5,0, 95% CI 1,23-20,3).
Conclusion. In the studied group of patients with STE-ACS subject to intervention, the cfDNA concentration before PCI was associated with the implantation of ≥2 stents and the stent length (>24 mm). CfDNA level before PCI was associated with the number of segments of impaired local LV contractility (≥2).
What is already known about the subject?
- Proprotein convertase subtilisin/kexin type 9 (PCSK9) is involved in the regulation of lipid metabolism by acting on low-density lipoprotein receptors.
- PCSK9 enhances the expression of interleukins, modulating inflammatory mechanisms in atherosclerosis.
What might this study add?
- PCSK9 and inflammatory markers (interleukins -8, -10) are associated with cardiovascular risk and are associated with carotid atherosclerosis.
How might this impact on clinical practice?
- A personalized approach given biomarker levels for cardiovascular risk prediction in hypertensive patients.
Proprotein convertase subtilisin/kexin type 9 (PCSK9) is involved in lipid metabolism, has local and systemic effects in immunoregulation and atherogenesis in hypertensive patients.
Aim. To personalize cardiovascular risk (CVR) stratification taking into account the diagnostic value of PCSK9 and inflammatory markers in men with hypertension and carotid atherosclerosis.
Material and methods. The study included 162 males with stage I-III hypertension of various CVR. All patients underwent collection of complaints and medical history, physical examination with anthropometry. The following laboratory test were performed: complete blood count with white blood cell differential and erythrocyte sedimentation rate, assessment of fibrinogen, C-reactive protein (CRP), total cholesterol, low-density lipoprotein cholesterol, triglycerides, blood glucose, serum creatinine level. Glomerular filtration rate and microalbuminuria were also evaluated. Serum PCSK9, interleukins-8, 10 (IL-8, 10) were determined by enzyme immunoassay. In addition, 24-hour blood pressure monitoring, extracranial artery ultrasound with determination of intima-media thickness and carotid stenosis severity were performed. Patients were divided into 3 groups according to PCSK9 level.
Results. Analysis of conventional cardiovascular factors and cytokine status (IL-8 and IL-10) in patients showed an inverse relationship between age and IL-8 (r=-0,230; p=0,036), IL-8/IL-10 (r=-0,309; p=0,005); heredity and IL-8/IL-10 (r=-0,423; p=0,001). There were following relationships between CVR factors and PCSK9: direct relationship between men's age (r=0,220, p=0,032), systolic and diastolic blood pressure (r=0,230, p=0,033; r=0,260, p=0,015) and PCSK9; inverse relationship between PCSK9 and heredity (r=-0,286, p=0,011). C-reactive protein and erythrocyte sedimentation rate were associated with IL-10 levels, which are associated with anti-inflammatory activity (r=0,78; p=0,02; r=0,78; p=0,02, respectively). The IL-8/IL-10 cytokine imbalance was most pronounced in patients with a night-peaker 24-hour systolic blood pressure profile (p=0,02). Patients with intima-media thickening and plaques had a highest level of PCSK9 (p=0,006). IL-8 levels were significantly higher with unchanged intima-media thickness (p=0,01).
Conclusion. In patients with high levels of PCSK9, there is a close relationship between risk factors for hypertension and cytokine imbalance. The severity of extracranial artery atherosclerosis significantly depends on the increase in the levels of PCSK9 (p=0,006) and inflammatory markers (IL-10) (p=0,044).
- Carotid artery ultrasound in rheumatoid arthritis (RA) has been identified as a screening method for asymptomatic plaques or cardiovascular risk reclassification.
- Parameters of plaque burden demonstrate a pronounced prognostic significance for cardiovascular events.
- The work shows for the first time that peripheral plaque burden in RA in combination with coronary artery disease (CAD) is higher than in patients with RA without CAD, which can be considered as a stage in the non-invasive diagnosis of CAD in RA.
Aim. To assess plaque burden according to peripheral artery ultrasound examination in patients with rheumatoid arthritis (RA) with low and moderate disease activity in comparison with the coronary artery condition.
Material and methods. The study included 64 patients, of which 43 patients with an established diagnosis of RA and 21 patients with coronary artery disease (CAD) without RA (comparison group). All patients underwent a clinical and paraclinical examination to verify myocardial ischemia and/or CAD according to the 2020 national guidelines, as well as a carotid and femoral artery ultrasound (the latter, only for patients with RA) with determination of plaque burden.
Results. In patients with RA in combination with CAD, plaque burden is higher than in patients with RA without coronary artery disease regarding the carotid plaque number 4,0 [4,0; 5,0]/2,0 [1,0; 3,5], proportion of maximum stenosis 35,0 [35,0; 45,0]/30,0 [25,0; 35,0] and the proportion of total stenosis 120,0 [110,0; 152,5]/85,0 [40,0; 110,0]. Three or more carotid plaques determine significant coronary atherosclerosis in RA. In RA patients with CAD, the combination of carotid and femoral plaques is associated with significant coronary atherosclerosis in 75% of cases. In a comparative analysis of patients with RA CAD+/RA CAD-, no significant differences were found in the main cardiovascular risk factors, lipid, and inflammatory parameters. When comparing the plaque burden indicators, the severity of coronary atherosclerosis was not revealed between RA patients with CAD+ and the comparison group.
Conclusion. Determining the peripheral plaque burden parameters increases the clinical significance of ultrasound as a stage of non-invasive CAD diagnosis in RA.
What is already known about the subject?
- The recent novel inflammatory biomarkers based on white blood cell count and subtypes (systemic immune-inflammation index, systemic inflammation response index, aggregate index of systemic inflammation) potentially demonstrate an important role in the course of cardiovascular diseases.
What might this study add?
- These novel markers of systemic inflammation are significantly higher in patients with confirmed atherosclerosis than in patients without it.
How might this impact on clinical practice?
- Novel inflammatory markers are an easy-to-use and affordable method for determining chronic inflammatory status in patients with coronary artery disease in routine clinical practice.
Aim. To compare the levels of novel biomarkers of systemic inflammation in patients with and without atherosclerosis, as well as between groups of patients with atherosclerosis of different severity.
Material and methods. Patients with suspected coronary artery disease after selective coronary angiography were included. The analysis included 901 patients with mean age of 61±10 years (men, 60% (n=549)). The patients were divided into two following groups: with and without atherosclerosis. The Propensity Score Matching method was used to adjust for baseline clinical differences.
Results. In the group with atherosclerosis, the values of the systemic inflammation response index (SIRI), systemic immune-inflammation index (SII) and aggregate index of systemic inflammation (AISI) were significantly higher than in patients without atherosclerosis: 0,906 (0,632; 1,36) vs 0,745 (0,519; 1,02), p<0,001; 457 (350; 641) vs 425 (313; 547), p=0,005 and 233 (148; 346) vs 179 (121; 263), p<0,001, respectively. ROC analysis showed the following threshold values of the studied parameters: for SIRI >1,05, area under the curve (AUC) confidence interval (CI) — 0,615 (0,571-0,658), p<0,001, sensitivity — 42,6%, specificity — 77,3%; for SII >368, AUC CI — 0,572 (0,528-0,616), p=0,004, sensitivity — 72,1%, specificity — 43,4%; for AISI >248, AUC CI — 0,604 (0,560-0,647), p<0,001, sensitivity 47,4%, specificity 71,1%. SIRI had the highest AUC. When comparing 6 groups according to the Coronary Artery Surgery Study (CASS) classification, significant differences were found in SIRI and AISI, p<0,001 and p=0,0016, respectively. However, these differences did not have a logical pattern.
Conclusion. Novel markers of systemic inflammation (SIRI, SII and AISI) were significantly higher in patients with confirmed atherosclerosis than in patients without it. There are following threshold levels associated with atherosclerosis: for SIRI >1,05, for SII >368, for AISI >248.
- During the COVID-19 epidemic in 2020, there was a significant decrease in population levels of low-density lipoprotein cholesterol and high-density lipoprotein cholesterol compared to the previous 5-year observation in the summer and spring periods, respectively.
- Decreased high-density lipoprotein cholesterol levels are associated with an increased immune response to SARS-CoV-2 S1/S2 infection, with a more pronounced effect in women.
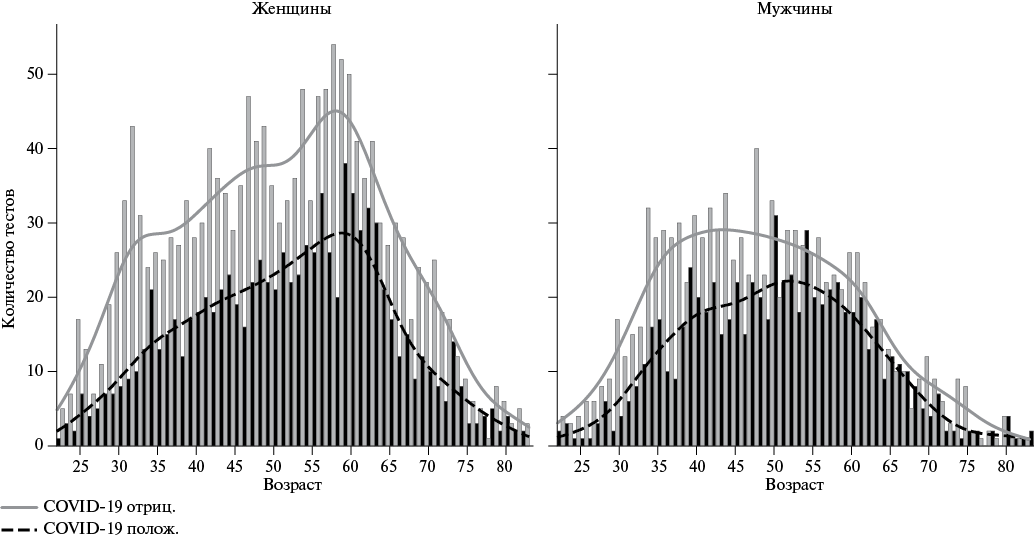
Aim. The aim of this cross-sectional retrospective study was to study the effect of SARS-CoV-2 S1/S2 infection on population lipid parameters, which are leading risk factors for the development and progression of atherosclerosis, which can be significantly distorted in systemic inflammation and, in particular, during respiratory viral infections.
Material and methods. We analyzed anonymized results of one-time, one-year studies of complete lipid profiles and related laboratory parameters performed in the Helix Laboratory Service from February 1, 2015 to December 30, 2020 in 238541 males and 384437 females aged from 22 to 83 years in 334 populated areas of the European Russia using Roche Cobas C502, C702 (Roche Diagnostics GmbH, Mannheim, Germany), LIAISON XL (DiaSorin S.p.A, Italy) analyzers.
Statistical analysis included methods of descriptive statistics, distribution analysis, sample comparisons, and search for dependencies.
Results. A dramatic change in the magnitude and nature of seasonal population fluctuations in low-density lipoprotein cholesterol and high-density lipoprotein cholesterol (HDL-C) during the COVID-19 spread has been identified.
COVID-19 differentially affects the relationship between high-sensitivity C-reactive protein (hsCRP) and atherogenic and antiatherogenic lipoproteins. These relationships have sex differences, are nonlinear, and in relation to HDL-C are associated with the level of specific anti-SARS-CoV-2 S1/S2 antibodies.
Up to a hsCRP level of 2,5 mg/l, there is a significant increase in population levels of low-density lipoprotein cholesterol with a correlation coefficient of 0,14 for women (p<0,001) and 0,10 for men (p<0,001). At hsCRP levels >2,5 mg/l, the trend reverses. At the same time, HDL-C levels sharply decrease with a negative correlation of -0,23 (p<0,001) in women and -0,22 (p<0,001) in men with hsCRP values <2,5 mg/l, followed by a less pronounced decline.
Conclusion. The study results may be useful for optimal prevention development and adequate assessment of atherogenic dyslipidemia treatment effectiveness in patients after COVID-19.
ОЦЕНКА РИСКА
- The role of the triglyceride-glucose index (TGI) as an additional risk cardiovascular factor has been determined.
- Elevated TGI levels have been shown to be associated with micro- and macrovascular changes in patients at moderate, high and very high cardiovascular risk.
Aim. To evaluate the association of the triglyceride-glucose index (TGI) with micro- and macrovascular changes in patients with moderate, high and very high cardiovascular risk (CVR).
Material and methods. The study included 134 men and 129 women aged 40 to 65 years with a SCORE2 ten-year risk of adverse cardiovascular events of 2,5% or more. Based on a detailed survey, a comprehensive physical and paraclinical examination, the relationship between TGI and CVR factors was assessed using Pearson correlation analysis, followed by a linear correlation strength assessment using the Chaddock scale. Modeling of the TGI association with macro- and microvascular damage in patients with moderate CVD was performed using multivariate logistic regression.
Results. According to regression analysis, increased TGI was associated with an increased risk of both macrovascular and microvascular changes. Similar results were obtained using multivariate logistic regression with model adjustment for age, sex, body mass index, waist circumference, smoking, hypertension, family history of premature cardiovascular disease, lipid-lowering therapy, and glucose-lowering therapy. An increased level of TGI was associated with an increase in the odds ratio (OR) of carotid atherosclerosis (OR 1,73, 95% confidence interval 1,27-2,36, P for trend <0,001), an increase in the urine albumin-creatinine ratio (OR 1,61, 95% CI 1,22-2,13, P for trend <0,001) and a decrease in estimated glomerular filtration rate (OR 1,67, 95% CI 1,10-1,50, P for trend =0,02).
Conclusion. TGI is an important and accessible additional risk factor for both micro- and macrovascular damage in everyday clinical practice, regardless of whether the patient has diabetes. For personalized CVR stratification and determination of further management tactics for patients with moderate, high and very high CR, the maximum available factors should be assessed, each of which can influence the disease course, while the summation of the main and additional factors significantly worsens the prognosis.
- In a population sample of 55-84 years old, a high prevalence of endothelial dysfunction was revealed according to the brachial artery flow-dependent vasodilation test (<10%).
- In the age range of 55-84 years, no associations were identified between flow-dependent vasodilation and cardiometabolic diseases.
- For the first time in a Russian population sample, the determinants of a decrease in flow-dependent vasodilation with aging (metabolic risk factors and smoking) were determined.
- In old and senile age, it remains relevant to correct metabolic risk factors and quit smoking to prevent the progression of endothelial dysfunction.
Aim. To evaluate the association of flow-mediated vasodilation (FMD) with cardiometabolic diseases (CMDs) and their risk factors (RF) in old age.
Material and methods. The study was conducted in the Russian population cohort of the HAPIEE project (Novosibirsk, 2015-2018). Endothelial function was assessed in a random subsample (788 men and women aged 55-84 years) using ultrasound measurements of the brachial artery FMD. Endothelial dysfunction (ED) was recorded with FMD <10%. Cardiovascular diseases (CVD) and risk factors were assessed using standard epidemiological methods.
Results. The incidence of hypertension (HTN) was 78,8% (the same in men and women), major CVDs — 21,7% and 17,1%, type 2 diabetes (T2D) — 18,7% and 19,1% in men and women, respectively. The mean FMD values were 2,7% (SD 7,32) and 3,2% (7,19), while the prevalence of ED was 88,2% and 85,8% in men and women, respectively, and did not differ significantly by sex. Men with ED had higher levels of blood triglycerides (125,1 (71,23) vs 102,7 (45,79) mg/dl; p=0,033), waist/hip circumference indices (0,94 (0,050) vs 0,92 (0,076); p=0,009) and body weight (27,7 (45,79) vs 26,5 (4,36) kg/m2; p=0,077). In women, a tendency towards an association of ED with smoking was revealed (p=0,067). There were no associations of ED with HTN, T2D and CVD in men and women.
Conclusion. The PMD test demonstrated a high incidence of ED in a population sample of 55-84 years old. ED is associated with metabolic risk factors in men and smoking in women. No associations of PMD with CMDs were found, presumably due to the high incidence of ED and cumulative disease in the elderly. Modification of metabolic risk factors and smoking cessation are relevant at any age to prevent the progression of ED.
METHODS OF STUDY
- Patients living in the Far North have more frequent and complex coronary atherosclerosis.
- According to optical coherence tomography, thin-cap fibroatheroma is more often determined in patients living in extreme weather conditions.
- Thin-cap fibroatheroma is associated with a risk of adverse cardiovascular events.
Aim. To evaluate the plaque structural features in patients with coronary artery disease (CAD) permanently residing in the Far North of the Tyumen region in comparison with patients in the South of the Tyumen region.
Material and methods. This pilot case-control study included 32 patients with stable CAD (mean age 62,7±8,9 years, 24 (75%) men). The main group consisted of 16 patients permanently residing in the Far North of Tyumen region (non-indigenous population), while the comparison group consisted of 16 patients permanently residing in the South of the Tyumen region. In all patients, CAD was verified using paraclinical diagnostic methods. All patients underwent optical coherence tomography (OCT), according to which the plaque type was analyzed. The following plaque types were distinguished: fibrous, fibroatheroma, calcified fibroatheroma, thin-cap fibroatheroma (TCFA). TCFA was defined as the presence of a fibrous cap ≤65 μm thick and an arc of the necrotic core of at least 90о. In addition, a lipid-rich plaque was isolated, which was determined by a lipid arc of more than 180о.
Results. According to clinical and angiographic characteristics, patients in the compared groups were statistically comparable. A total of 134 plaques were analyzed from 32 patients (main group — 65 plaques; control group — 69 plaques (p>0,05)). The most common plaque type in both groups was calcified fibroatheroma (46,2% in the Far North group and 50,7% in the South group, p=0,609). TCFA was significantly more often detected in patients living in far north (33,8% vs 17,4%, p=0,031). In this group of patients, thin (<65 µm) fibrous plaque cap was also more often determined (35,4% vs 18,8%, p=0,034). Lipid-rich plaques in both groups was determined with the same frequency (56,9% vs 62,3%, p=0,598).
Conclusion. In patients with verified CAD living in extreme weather conditions, according to OCT, TCFA was more often determined, which could potentially be associated with a higher risk of adverse cardiovascular events.
What is already known about the subject?
- A novel version of electron microscopy of biological tissues allows the analysis of whole and intact segments of elements of cardiovascular system, including calcified atherosclerotic plaques.
What might this study add?
- Diagnostic electron microscopy of atherosclerotic plaques allows high accuracy assessment of the following instability-associated parameters: fibrous cap thickness, lipid distribution and volume, macrophage distribution and proportion, the nature of calcification.
How might this impact on clinical practice?
- Analysis of the results of pathophysiological and clinical effectiveness of anti-atherosclerotic therapy in clinical and preclinical trials.
Aim. To determine the potential of diagnostic electron microscopy of intraplaque processes (severity of lipid damage, fibrous cap thickness and condition, severity of pathological neovascularization, presence, nature and severity of calcification, ratio and distribution of various cell populations).
Material and methods. The study objects were plaques removed during endarterectomy from the human carotid artery and segments of the human internal mammary artery removed during coronary bypass surgery. Whole specimens were subjected to chemical fixation, staining with heavy metal salts, embedding in epoxy resin followed by layer-by-layer grinding, polishing, contrasting, visualization using back-scattered electron scanning electron microscopy and three-dimensional reconstruction with color mapping (modified EM-BSEM).
Results. The use of a modified EM-BSEM made it possible to: 1) visualize the fibrous cap thickness and assess the extracellular matrix; 2) analyze the neointimal lipid distribution; 3) perform three-dimensional reconstruction and analyze the microenvironment of calcifications of various sizes; 4) visualize endothelial cells, defects in interendothelial contacts and the basement membrane of neointimal capillaries with their subsequent three-dimensional reconstruction; 5) perform an analysis of age-dependent defects in the basement membrane and internal elastic membrane of the internal mammary artery. The resolution of the obtained images was significantly superior to intravascular imaging methods (intravascular ultrasound and optical coherence tomography), allowing additional assessment of capillary fluidity, the degree of calcification encapsulation and the condition of elastic fibers. Three-dimensional reconstruction of calcifications, neointimal capillaries and elastic fibers made it possible to assess their spatial density and heterogeneity. Simultaneously with the identification and assessment of these histological structures, objective phenotyping of cell populations was performed, which made it possible to isolate macrophages and foam cells, vascular smooth muscle cells, fibroblasts and endothelial cells in atherosclerotic plaques and automatically identify them through color mapping determined by their electronic contrast distribution signatures.
Conclusion. The modified EM-BSEM method allows for universal electron microscopic diagnosis of atherosclerotic and elastolytic lesions of large arteries with high information content about vascular remodeling and high accuracy. Electronic contrast distribution signatures unique for each cell population indicate the possibility of their automated phenotyping using specialized neural network algorithms.
МЕДИЦИНСКАЯ ИНФОРМАТИКА
- In patients with a high thromboembolism risk due to advanced atherosclerosis, therapy must be adjusted in a timely manner.
- Conventional statistics make it possible to identify groups with a high and low thromboembolism risk, but do not allow division into classes with different severity due to their insufficiently high diagnostic sensitivity and the unclear nature of the task.
- The use of fuzzy decision-making logic, synthesizing membership functions based on informative features makes it possible to differentiate an atherothrombotic condition by severity, which allows timely determination of preventive and therapeutic measures.
Aim. To develop a method for thromboembolism prediction in patients with advanced atherosclerosis.
Material and methods. The study involved 170 patients with advanced atherosclerosis and 110 patients with local atherosclerotic lesions. At the first stage, specialized experts generated signs characterizing the severity of prothrombotic conditions. To determine whether patients belonged to the first or second group, the multivariate statistics method was used. Decision rules (DRs) was developed based on soft computing (SC), as well as the methodology for the synthesis of hybrid fuzzy DRs.
Results. According to the discriminant function coefficient (DFC), the division into classes was made with the formation of an intersection area, which affected the diagnostic sensitivity of this method (=86%). Due to difficulties of separating more heterogeneous groups with a small sample, RP was synthesized according to the atherosclerosis severity classification using SC technology. Atherosclerosis severity classification was adopted according to fuzzy DRs: initiation stage (up to 20%); reverse stage (21-40%); progressive stage (41-65%); critical stage (more than 65%). Assessment of thromboembolism risk in advanced atherosclerosis in the examined patients showed the following trends: progressive stage — 55% of patients; critical stage — 21% of patients; reverse stage — 16% of patients; initiation stage — 7% of patients.
Conclusion. DFC for DRs makes it possible to identify groups with high and low thromboembolism risk. The resulting final fuzzy DRs make it possible to differentiate the atherothrombotic condition in advanced atherosclerosis by severity, which can help to timely determine preventive and therapeutic measures.
REVIEW
- The important role of imaging techniques in identifying vulnerable plaque has been demonstrated.
- Intravascular ultrasound, optical coherence tomography and multislice computed tomography can predict the risk of coronary events.
- Imaging methods make it possible to monitor the atherosclerotic process and the effectiveness of treatment.
The aim was to evaluate the potential of various imaging methods in the diagnosis of vulnerable coronary plaques and their stabilization using various lipid-lowering therapy regimens.
The sources were searched in the PubMed database using the following keywords: "vulnerable (unstable) plaque" AND "PCSK9 inhibitors" AND "intravascular ultrasound" OR "optical coherence tomography" OR "computed tomography angiography". As a result, 8 original clinical trials were selected that corresponded to the review purpose. We assessed the results of following studies on plaque imaging and their regression with various lipid-lowering therapy regimens: GLAGVO, ODYSSEY J, PACMAN-AMI, HUYGENS, ALTAIR, ARCHITECT, etc. The results of most studies have established the advantages of a combined regimen of lipid-lowering therapy (statin+PCSK9 inhibitor) in reducing the rate of cardiovascular events in comparison with statin monotherapy. The reduction in plaque volume ranged from 0,95% to 2,13% in patients receiving a combination of lipid-lowering drugs, while in monotherapy, it increased from 0,05% to 0,92% (GLAGOV, PACMAN-AMI). The changes of minimum fibrous cap thickness varied from 18,0-62,67 µm with combined therapy and 13,2-33,19 µm with monotherapy (PACMAN-AMI, Gao F). Lipid arc regression was 57,5о in combination therapy (statin+PCSK9 inhibitor) and 31,4о in statin monotherapy (HUYGENS). Imaging diagnostic methods makes it possible to identify vulnerable plaques, which helps in consideration of combination lipid-lowering therapy. In addition, plaque visualization makes it possible to evaluate the treatment effectiveness.
- Detection of preclinical abdominal aortic aneurysm (AAA) can significantly reduce mortality from complications.
- World practice of screening programs for AAA demonstrates their undeniable effectiveness.
- Russia needs research to assess the prevalence and risk factors of AAA, which would make it possible to develop own screening program.
Despite the global trend towards a decrease in the prevalence of abdominal aortic aneurysm (AAA), this disease remains one of the sudden death causes in the elderly. This necessitates the need to conduct screening studies, the effectiveness and feasibility of which has been proven in large studies, including population-based ones, and meta-analyses. The traditional and most optimal screening method is ultrasound examination. According to the guidelines of different countries, the indications for abdominal aorta ultrasound vary. Today in Russia there is no accurate data on the prevalence of AAA, while the target group for screening has not been defined, and therefore the country needs to conduct large population studies to study its prevalence and risk factors, as well as to calculate indicators of the clinical and economic effectiveness of implementation AAA screening programs.
What is already known about the subject?
- Lipidology is one of the fastest growing areas of medicine. The main targets of lipid-lowering therapy are low-density lipoprotein cholesterol, lipoprotein(a) and triglycerides.
What might this study add?
- Complete sequencing of the human genome has made it possible not only to identify the main molecular targets of hyperlipidemia, but also to develop innovative approaches to treatment.
How might this impact on clinical practice?
- Targeted lipid-lowering agents offer therapeutic solutions that could revolutionize the treatment of hyperlipidemia and atherosclerosis.
Despite a variety of lipid-lowering drugs, mostly pelleted, aimed at reducing low-density lipoprotein cholesterol and triglycerides, only a small number of patients achieve their target levels. The reasons are insufficient adherence to treatment, rare use of combined lipid-lowering therapy regimens by attending physicians, low availability and high cost of injected lipid-lowering agents. With the advent of technologies for targeted therapy for hyperlipidemia, a new era in cardiology opens. These innovations will lead to higher goal achievement rates through a personalized and precision approach to hyperlipidemia treatment. Novel lipid-lowering drugs are directed at the molecular targets of hypercholesterolemia, hyperlipoproteinemia(a) and hypertriglyceridemia. The review purpose is to systematize following information about innovative lipid-lowering drugs: mechanism of action, stage of development, effectiveness and safety.
- Lack of uniform criteria for familial combined hyperlipidemia (FCH).
- High variability of the FCH phenotype in the same person over time and among members of the same family.
- The difficulty of differential diagnosis of FCH with both monogenic familial hypercholesterolemia and secondary combined hyperlipidemia.
- Insufficient study of the molecular genetic basis of FCH, as well as its monogenic and/or polygenic forms.
Among the various dyslipidemia types, familial combined hyperlipidemia (FCH) is the most common genetic disorder, which is characterized by at least two different forms of lipid disorders: hypercholesterolemia and hypertriglyceridemia. In FCH, the risk of atherosclerotic cardiovascular diseases (CVDs), including at a young age, increases significantly. The aim was to analyze literature data on modern criteria for diagnosis, pathogenesis and data from molecular genetic studies of FCH. Future studies aimed at understanding the underlying genetic and metabolic mechanisms of FCH and developing effective treatment strategies should include larger cohort studies with greater genetic diversity, as well as investigation of epigenetic and lifestyle factors.
CLINICAL PHARMACOLOGY
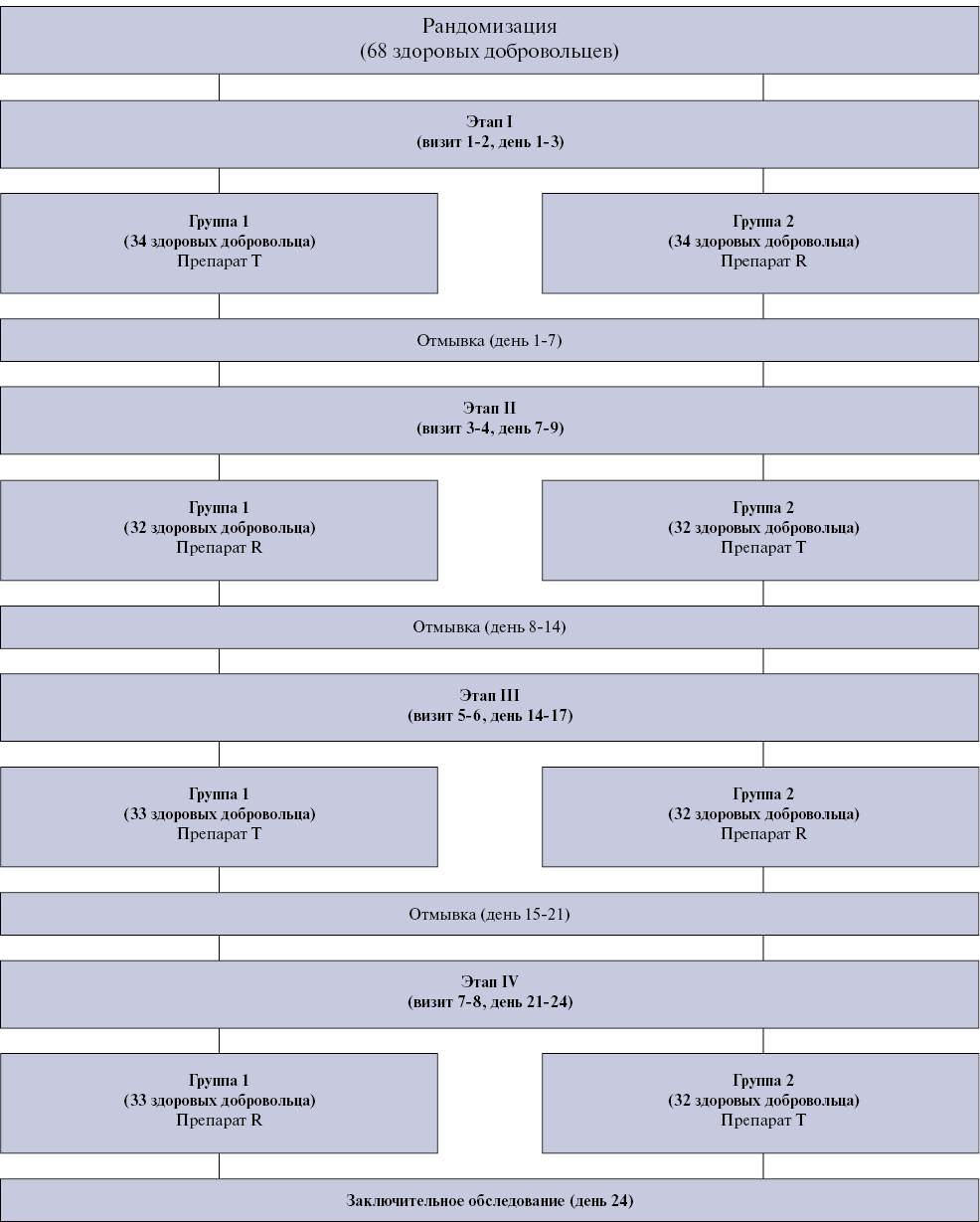
Aim. To study the comparative pharmacokinetics and confirmation of bioequivalence of the generic (T) and original (R) dabigatran etexilate in healthy volunteers after a single oral dose under fasted conditions.
Material and methods. To confirm bioequivalence, an open-label, randomized, replication, crossover, four-step study was conducted to compare the pharmacokinetics and bioequivalence of generic and original dabigatran with a single oral dose 150 mg dabigatran etexilate under fasted conditions in adult healthy male and female volunteers. Sixty-eight subjects participated in the study. During the study, blood plasma samples were taken from volunteers, in which the concentration of total and free dabigatran was determined. Based on the data obtained, pharmacokinetic and statistical analysis was carried out and 90% confidence intervals were calculated for the ratio of mean pharmacokinetic parameters (Сmax, Tmax, AUC0-t, AUC0-∞, AUCt-∞, T1/2, AUCt-∞/AUC0-∞) for total and free dabigatran.
Results. The established 90% confidence intervals for the ratio of AUC0-t, AUC0-∞ and Cmax values for total dabigatran were 82,56-96,36% (mean ratio, 89,19%), 82,39-95,90% (mean ratio, 88,89%) and 85,98-99,17% (mean ratio, 92,34%), respectively. The established 90% confidence intervals for the ratio of AUC0-t, AUC0-∞ and Сmax values for free dabigatran were 83,37-98,29% (mean ratio, 90,53%), 82,98-97,33% (mean ratio, 89,87%) and 85,04-99,28% (mean ratio, 91,88%), respectively. For the estimated pharmacokinetic parameters of dabigatran etexilate, 90% confidence intervals ranged from 80-125% for AUC0-t, AUC0-∞ and Cmax. Additional safety analysis was carried out. Generic and original dabigatran were well tolerated by the volunteers. There were no significant differences in vital signs, paraclinical characteristics throughout the study compared with the initial data, as well as significant differences between the drugs in all studied parameters of adverse events.
Conclusion. The study showed that generic and original dabigatran are bioequivalent. In addition, the data obtained indicate that the agents have similar safety profiles.
INFORMATION
ISSN 2618-7620 (Online)