REVIEW
- In recent years, evidence has been obtained on the potential of circulating cell-free nucleic acids as early and specific biomarkers of cardiovascular diseases (CVD) in order to develop methods for early diagnosis, risk stratification and prognosis of the disease.
- The level of cell-free DNA is elevated in patients with CVD, but there are conflicting data regarding its relationship with other myocardial damage markers and its significance as markers of various pathological conditions.
- Assessment of plasma level and profile of circulating microRNAs is a promising approach for the development of methods for early diagnosis, monitoring and prognosis of the outcome of various pathological conditions in CVD.
- Levels of cell-free DNA and microRNA may be a specific marker of heart transplant rejection, which requires further study.
One of the urgent tasks is the search for early and specific markers of cardiovascular diseases (CVD) in order to stratify the cardiovascular risk, develop methods for their prevention, early diagnosis and treatment. In recent decades, considerable attention has been paid to plasma cell-free nucleic acids free: circulating cell-free DNA (сfDNA) and circulating non-coding RNA, in particular microRNA, which are considered as promising prognostic and diagnostic biomarkers of many pathological conditions, since they play a key role in the regulation of physiological and pathophysiological processes. This review covers current understanding of the potential of plasma cfDNA and microRNA assessment in cardiovascular patients as specific biomarkers for diagnosis, risk stratification, severity assessment and monitoring of CVD, with a focus on coronary artery disease, heart failure and cardiac allograft rejection, where this area of research is promising.
What is already known about the subject of the study?
- Cerebral microbleeds (CMBs) are considered as a predictor of intracranial hemorrhage, which requires analysis of current research data on the safety of oral anticoagulants.
What might this study add?
- The incidence of CMBs in patients with atrial fibrillation receiving oral anticoagulants reaches 30% and increases with age. Superficial CMBs and their increased number are associated with a 6-fold increased risk of intracranial hemorrhage.
How might this impact on clinical practice?
- Further studies in this area are needed in patients receiving direct oral anticoagulants, as the data remain contradictory.
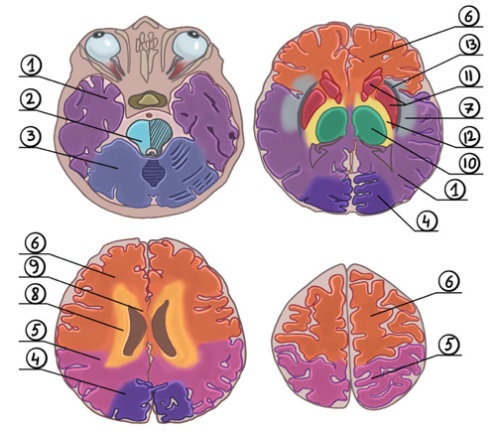
Oral anticoagulants are currently widely used, which requires continued research on their safety. With the improvement of diagnostic methods and power of magnetic resonance systems, cerebral microbleeds (CMBs), which are small deposits of hemosiderin-laden macrophages around the brain vessels, are increasingly being detected. Recently, CMB has been considered as a predictor of intracranial hemorrhage with oral anticoagulant use. In this regard, we decided to summarize the data on the safety of oral anticoagulants in relation to CMBs.
- In atrial fibrillation, inflammasome activation leads to maintenance of ectopic activity.
- In heart failure, the inflammasome promotes initiation of myocardial remodeling and maintenance of chronic inflammation in the cardiac tissue.
- The inflammasome cascade is triggered by myocarditis and pericarditis, which promotes maintenance of inflammatory reactions.
- Coronary artery disease is accompanied by inflammasome activation in cardiomyocytes, which leads to necrosis progression and, as a consequence, to cardiac dysfunction.
- Therapy aimed at inhibiting the inflammasome is a promising method for treating cardiovascular diseases; however, many drugs have not been studied enough at the moment and cannot be used in routine practice.
The role of inflammasomes in cardiovascular diseases has not been sufficiently studied at present. However, there are a number of recent studies showing the participation of these multiprotein complexes in the development and progression of cardiovascular diseases. Thus, in atrial fibrillation, the inflammasome triggering helps to reduce the duration and refractivity of the atrial action potential, induction of early and/or delayed afterdepolarization, which maintains ectopic activity. In heart failure, the triggering of inflammasome cascade initiates and maintains chronic inflammation, leading to cardiac remodeling and fibrosis. In coronary artery disease, inflammasome activation maintains ischemia and increases the necrosis area. Inflammatory reactions in pericarditis and myocarditis also do not occur without the participation of this multiprotein complex. In these pathologies, inflammasome inhibition helps to improve clinical symptoms and normalize the cardiac function. Therefore, inflammasome inhibitor agents can become a promising method of therapy in the above diseases.
- Vascular dementia and vascular cognitive impairment (VCI) are an interdisciplinary problem, and its comprehensive study can make it possible to develop novel diagnostic and therapeutic strategies to reduce the burden of vascular dementia for families and society.
- There is no consensus on the relationship between acute myocardial infarction and the risk of moderate VCI and vascular dementia.
- Based on the presented studies, a significant relationship was found between myocardial infarction and the development and progression rate of moderate VCI and vascular dementia.
Patients with acute myocardial infarction (MI) are identified by Russian and foreign experts as a risk group for moderate vascular cognitive impairment (VCI) and vascular dementia. As a result of various pathogenetic mechanisms, patients with MI develop the so-called cardiac cerebral syndrome, which makes a significant contribution to global cognitive impairment in this group of patients. The impact of MI on the risk and progression of cognitive impairment is one of the key links in improving the prognosis and quality of life in patients after MI. The aim of the review was to analyze the incidence of moderate VCI and vascular dementia in patients with MI in the acute and late periods.
Dilated cardiomyopathy is one of the most common types of cardiomyopathy, characterized by left ventricular dilation and systolic dysfunction. The disease is accompanied by a high risk of adverse outcomes, including heart failure decompensation and sudden cardiac death (SCD). Traditionally, only left ventricular ejection fraction ≤35% was used to identify candidates for cardioverter-defibrillator implantation for the primary prevention of SCD. However, with the advances in therapy for heart failure, cardiac resynchronization therapy and modern cardiac imaging techniques such as delayed contrast-enhanced magnetic resonance imaging and genetic tests, SCD risk stratification approaches should be revised. This paper reviews the state of the art on SCD risk stratification in patients with dilated cardiomyopathy. Particular attention is paid to the role of magnetic resonance imaging and genetic studies, which significantly expand the potential of risk assessment and allow more accurate identification of patients requiring cardioverter-defibrillator implantation for primary SCD prevention.
- The use of telemedicine technologies in patients with heart failure does not affect the quality of life of patients.
- Existing studies on the impact of telemedicine technologies on the quality of life of patients with heart failure have limitations, which could affect the results obtained.
- Randomized controlled trials are needed on a large number of patients with heart failure, evaluating various methods for assessing quality of life.
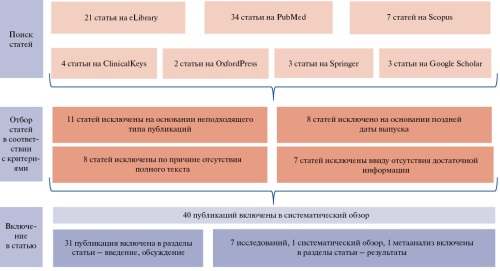
Aim. To study the literature data and evaluate the telemonitoring results in patients with heart failure to determine their impact on the quality of life.
Material and methods. We searched information according to PRISMA requirements using the following databases: PubMed, Embase, Crossref, MedLine, Clinical Trials and e-Library. Ten randomized controlled trials were selected for the final analysis of full-text articles. In these studies, the quality of life was analyzed using the Minnesota Living with Heart Failure Questionnaire (MLHFQ) and EuroQol-5 Dimension (EQ-5D Utilities and EQ-5D VAS) questionnaire.
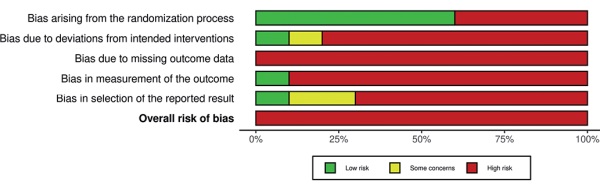
Results. Among 285 patients with telemonitoring and 294 patients with standard management, MLHFQ did not reveal statistical significance (mean difference -0,75, -7,08-5,58, I2=97%, p=0,82). Similar results were obtained for the EuroQol-5 Dimension (EQ-5D VAS — mean difference 2,76, -1,23-6,74, I2=44%, p=0,18) and EQ-5D Utilities (mean difference 0,00, -0,05-0,05, I2=0%, p=1,00) questionnaires.
Conclusion. The current systematic review and meta-analysis showed that the use of telemedicine technologies in patients with heart failure does not affect the quality of life of patients.
- Automatic reports generated by ambulatory blood pressure monitoring devices still contain blood pressure load indices, which can potentially be used by doctors instead of standard blood pressure level to make unfounded clinical decisions.
- The studies available in the literature do not support the independence or superiority of blood pressure load indices over the mean 24-hour or mean day-time or night-time blood pressure; and those studies specifically asked about such superiority or independence give a negative answer to it.
- Based on the available literature data covered by this review, there is no justification for the treatment of hypertension based on the target blood pressure load values.
The aim of this review was to answer the question of whether clinical and research practice require blood pressure load indices from ambulatory BP monitoring data.
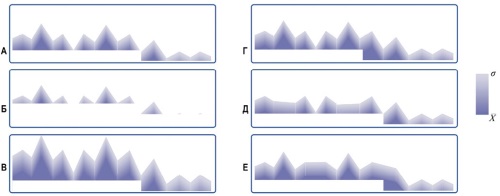
To identify related publications, a search of Pubmed, eLibrary, elpub databases and snowball sampling were used. A total of 264 publications were found. Then, publications were excluded in which the term "blood pressure load" stayed out of the context of 24-hour BP monitoring, as well as reviews and studies with fewer than 21 observations. A total of 69 publications selected were classified as follows: outcome studies; studies on target organ damage and risk factors; studies in special groups; intervention studies.
The literature review showed that there are no studies with methodology provided evidence of a clear additional value of BP load compared to mean BP values. In contrast, studies with high statistical power specifically aimed at the question under study showed lack of predictive power of BP loads for either outcome or target organ damage in general and special populations. There is also no evidence that any intervention based on target BP loads is superior to treatment based on standard BP. The results of our review suggest that there is no need to calculate BP loads. Routine clinical decision-making should be based only on standard BP values compared with the thresholds adopted by medical scientific societies in clinical guidelines.
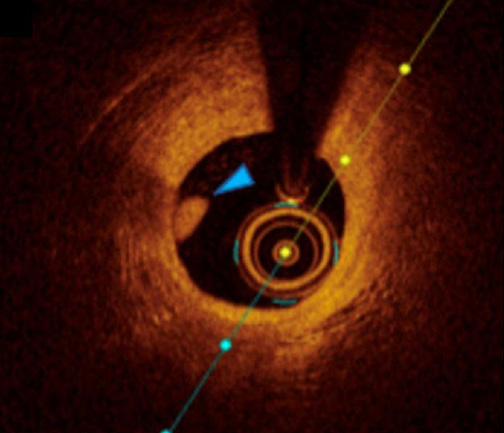
- Modern imaging methods allow to detect acute thrombosis of the infarct-related artery in patients with non-ST-elevation acute coronary syndrome.
- Improvement of thrombosis diagnosis methods allows to improve the quality of healthcare for cardiovascular patients.
- Systematization of literature data on the applied imaging methods of acute thrombosis of the infarct-related artery in patients with non-ST-elevation acute coronary syndrome.
Cardiovascular diseases, in particular ST-elevation (STE-ACS) and non-ST-elevation (NSTE-ACS) acute coronary syndrome remain one of the main causes of death worldwide. Published data indicate that in a number of patients, the cause of NSTE-ACS is infarct-related artery occlusion. In modern medicine, there are both invasive and non-invasive coronary thrombosis imaging methods. The aim of the study was to analyze and systematize the literature data on coronary thrombosis imaging methods. The review was prepared using publications indexed in the PubMed, Google Scholar, Web of Science, and Cyberleninka databases. The search depth was 5 years, starting from 2020. The review is based on summarized data from the most relevant clinical studies, reports, and systematic reviews. The conducted literature analysis showed that both invasive and non-invasive imaging methods have a number of advantages and disadvantages. In this regard, improving these techniques remains an urgent research task.
ПРОБЛЕМНАЯ СТАТЬЯ
What is already known about the subject?
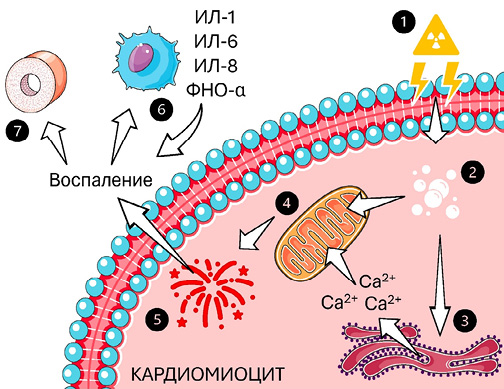
- One of the serious complications of radiation therapy (RT) is radiation-induced heart disease.
What might this study add?
- The pathogenesis of post-radiation heart injury is described in detail from the point of view of acute and delayed body reactions.
- Modern photon therapy limits the risk of cardiac dysfunction, and proton therapy can reduce it to 2,9%.
How might this impact on clinical practice?
- The data obtained can help in the development of safer and more effective RT protocols to reduce the risk of cardiotoxicity.
- Optimization of cardiac function monitoring in patients after RT can improve their long-term health and survival.
Post-radiation chest injury is characterized by complications in the lungs and heart. Radiation-induced cardiac and vascular damage has been described by various authors. Currently, there are 5 following main types of heart injury after radiation therapy: pericarditis, cardiomyopathy, coronary artery disease, acquired valvular heart disease and arrhythmias. The scientific community continues to study this group of heart diseases. There are no unambiguous data on the prevention of these conditions. The aim of this work was to summarize current information on the pathogenesis and consequences of post-radiation heart injury.
ISSN 2618-7620 (Online)