ХРОНИЧЕСКАЯ СЕРДЕЧНАЯ НЕДОСТАТОЧНОСТЬ
- We presented the results of PRIORITY-HF study — the first large-scale prospective study of outpatients with heart failure in Russia.
- Despite the relatively low mortality and hospitalization rates per year, the data obtained indicate an unfavorable clinical profile of outpatients with heart failure, characterized by a younger age and a high severity of comorbidities.
- The results emphasize the need for targeted measures to improve the cardiovascular-kidney-metabolic health of the population.
Aim. Geographic heterogeneity of phenotypes and prognosis in heart failure (HF) highlights the need for region-specific data. The aim of the study was to evaluate characteristics, therapy, and 1-year outcomes in a Russian large representative cohort of outpatients with HF.
Material and methods. PRIORITY-HF is a prospective, observational, multicenter registry study. From 2020 to 2022, outpatients diagnosed with HF aged 18 years and older were included in 50 regions of the Russian Federation.
Results. The study included 19,981 patients with HF (mean age 64.9 years; 63.5% men). HF with reduced ejection fraction (HFrEF) was diagnosed in 34.9% of patients, while HF with mildly reduced ejection fraction (HFmrEF) — in 24.7%, and HF with preserved ejection fraction (HFpEF) — in 40.4%. The most common comorbidities were hypertension (89.0%), coronary artery disease (73.4%), obesity (45.2%), chronic kidney disease (44.7%), and atrial fibrillation/flutter (42.5%).
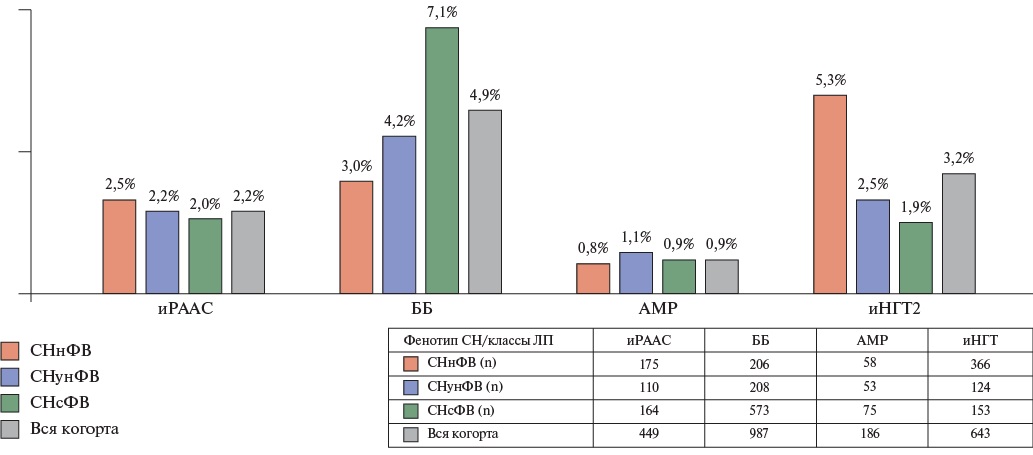
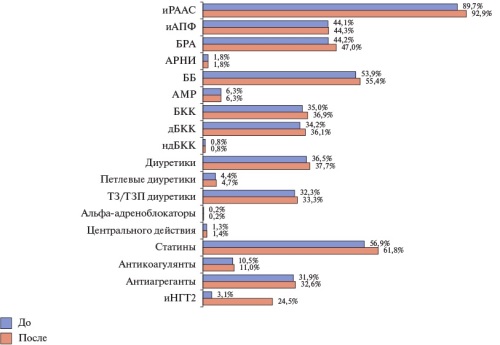
There was high prescription rate of individual classes of recommended HF therapy as follows: 92% of patients received renin-angiotensin-aldosterone system inhibitors, 86% — beta-blockers, 72% — mineralocorticoid receptor antagonists and 40% — sodium-glucose cotransporter-2 inhibitors, but only 46.6% of patients with HFrEF received quadruple therapy.
After 12 months, all-cause mortality was 5.2% in the overall group (HFrEF: 8.1%; HFmrEF: 4.6%; HFpEF: 3.1%), while cumulative HF-related hospitalization rate — 6.3% (HFrEF: 10.4%; HFmrEF: 6.2%; HFpEF: 2.9%).
Conclusion. The obtained data indicate a relatively young age of patients with HF in Russia with a high level of comorbidities and suboptimal therapy, especially in HFrEF. With relatively low mortality and rehospitalization rates, significant differences between the EF subgroups were revealed, which emphasizes the need for targeted interventions to improve the quality of care and prognosis.
Material and methods. This retrospective analysis of contraindication rate to four GDMT classes was performed in 19981 outpatients with HF included in the PRIORITYHF study. The changes of drug prescription and titration were assessed in a cohort of patients without contraindications and who underwent visits at 6 and 12 months of follow-up. The multivariate mixed logistic regression was used to determine factors associated with the prescription and higher doses of GDMT drugs.
Results. A total of 1943 (9,7%) study participants had baseline contraindications to at least one GDMT class. Among the 15575 patients without contraindications who completed all study visits, quadruple therapy coverage increased from 12% (before Visit 1) to 28,1% (after Visit 3) in the overall cohort, from 21,6% to 47,4% in HF with reduced ejection fraction (HFrEF), from 11,5% to 28,2% in HFrEF with mildly reduced EF (HFmrEF), and from 4,5% to 12,7% in HFpEF. Target GDMT doses were used in a small proportion of patients. Sixty (1,2%) patients with HFrEF received drugs with proven efficacy from all four GDMT classes at target doses by study completion. Patients’ age and sex, body mass index, systolic blood pressure and heart rate, comorbidities, cardiac resynchronization therapy, previous hospitalization with HF, duration and functional class of HF, and EF value were associated with the prescription of GDMT classes and higher doses.
Conclusion. Contraindications to at least one GDMT class were identified in 9,7% of patients with HF. For patients without initial contraindications, an increase in quadruple therapy coverage was noted during the follow-up period, but titration and achievement of target doses were insufficient. Increasing awareness and overcoming therapeutic inertia of physicians are critically important for increasing the coverage of patients with HF with optimal therapy.
- Hypertension (HTN) was registered in 89% of patients with heart failure (HF), a third of them did not achieve the target blood pressure (BP) level, and 10,2% had resistance to antihypertensive therapy (AHT).
- Resistance to AHT is associated with female sex, obesity, diabetes, the phenotype of heart failure with mildly reduced ejection fraction and heart failure with preserved ejection fraction, and the risk of hospitalization.
- Initiation of ≥1 class of AHT in uncontrolled HTN was noted only in 35,2% of patients.
- In heart failure with reduced ejection fraction (HFrEF) with uncontrolled hypertension, sodium-glucose cotransporter-2 inhibitors and quadruple therapy were prescribed less frequently.
- Uncontrolled HTN is associated with a lower risk of death, especially in HFrEF.
- Awareness of clinicians about the management strategy for patients with a combination of HF and HTN should be increased.
Aim. To assess the frequency, associated factors, features of hypertension (HTN) treatment and prognosis depending on blood pressure (BP) control and resistance to antihypertensive therapy (AHT) in outpatients with heart failure (HF).
Material and methods. This retrospective analysis of data from 19938 PRIORITYHF study participants with BP data at Visit 1 was performed. No BP control was defined as systolic and/or diastolic BP ≥140 and/or 90 mm Hg. In the absence of BP control on triple AHT (renin-angiotensin-aldosterone system inhibitor + calcium channel blocker + thiazide/thiazide-like diuretic) or BP control while taking triple AHT in combination with at least one other antihypertensive class, resistant HTN (uncontrolled and controlled, respectively) was diagnosed.
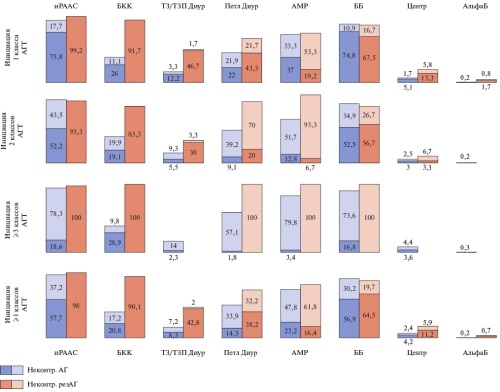
Results. HTN was diagnosed in 17750 (89,0%) patients, of which 32,1% were uncontrolled and 10,2% were resistant (including 4,5% as uncontrolled). In multivariate logistic regression, obesity, type 2 diabetes, and more severe congestion increased the probability of uncontrolled resistant HTN. Initiation of at least one new class of antihypertensives was noted in 2005 (35,2%) patients with uncontrolled HTN and in 152 (19%) patients with uncontrolled resistant HTN. Loop diuretics, mineralocorticoid receptor antagonists, and beta-blockers were most often added to therapy. Underuse of quadruple therapy was noted in HF with reduced ejection fraction, especially in uncontrolled HTN. In the overall group, the death risk was lower in uncontrolled HTN — odds ratio (OR) 0,798 [95% confidence interval (CI) 0,6810,935]. An independent association was found between uncontrolled resistant HTN and an increased probability of all-cause (OR 1,406 [95% CI 1,223-1,615], cardiovascular (OR 1,4 [95% CI 1,172-1,673]) and HF-related (OR 1,475 [95% CI 1,088-
2]) hospitalizations with no significant differences between subgroups in ejection fraction (p for correlation >0,05).
Conclusion. No BP control was detected in every third patient with HF and HTN. The association of uncontrolled resistant HTN with metabolic comorbidities, risk of hospitalization, and the need for multicomponent therapy require increased awareness among physicians about the tactics of managing patients with a combination of different phenotypes of HF and HTN.
- Patients with heart failure (HF) are insufficiently examined to identify markers of chronic kidney disease (CKD), while albuminuria, albumin/creatinine ratio are especially rarely assessed. In addition, incorrect glomerular filtration rate (GFR) estimation is noted.
- Confirmed CKD or CKD-EPI 2021 GFR based on patient sex, age, and entered serum creatinine (aGFR) <60 ml/min/1,73 m2 is associated with a more severe HF course, a greater burden of most cardiovascular comorbid conditions, and non-cardiac comorbidities such as obesity, diabetes, and anemia.
- With an aGFR increase from C1 to C5, the proportions of patients prescribed angiotensin-converting enzyme inhibitors, mineralocorticoid receptor antagonists, sodium-glucose cotransporter-2 inhibitors, renin-angiotensin-aldosterone system blockers, and quadruple therapy decreased.
- A decrease in estimated GFR in patients with HF was independently associated with the risk of death and rehospitalization.
Aim. To evaluate markers of chronic kidney disease (CKD) and their clinical and prognostic role in outpatients with heart failure (HF) based on real-world data.
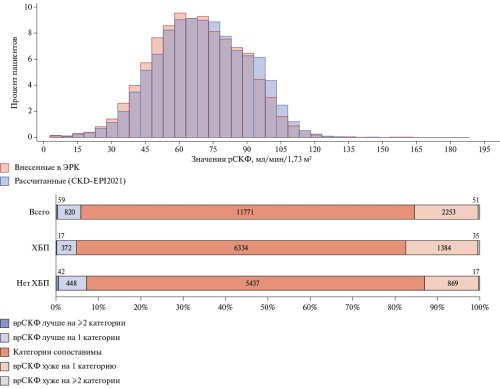
Material and methods. This retrospective analysis of data from the prospective observational multicenter registry study of patients with heart failure in Russia (PRIORITY-HF) was performed, including 19981 patients. To assess CKD markers, the following data obtained at Visit 1 were taken into account: "Has the diagnosis of Chronic Kidney Disease (CKD) been confirmed?", "CKD stage", "CKD-EPI Estimated glomerular filtration rate (eGFR)", "Creatinine", "Albumin" or "Albumin/ creatinine ratio" in a single urine portion. eGFR values entered in case report form were compared with the CKD-EPI 2021 eGFR values based on the patient’s sex, age and the entered serum creatinine (aGFR). Clinical characteristics, therapy after Visit 1 and prognosis were compared in patients with CKD and depending on aGFR value.
Results. The following diagnostic problems were identified: incorrect GFR estimation with more frequent underestimation of values and insufficient assessment of albuminuria. CKD was noted as a concomitant diagnosis in 44,7% of patients with HF, but aGFR <60 ml/min/1,73 m2 was determined in 30,8% of cases. Groups with both reported CKD and aGFR were characterized by a more severe HF course, a greater burden of most cardiovascular and non-cardiovascular (obesity, diabetes mellitus and anemia) comorbidities. A decrease in prescription rate of most classes of guideline-directed medical therapy for HF and quadruple therapy with aGFR <30 ml/min/1,73 m2 was noted. Both CKD and a decrease in aGFR <60 ml/min/1,73 m2 were associated with a higher rate of adverse events. A decrease in eGFR by every 10 ml/min/1,73 m2 was significantly associated with all adverse outcomes with extensive adjustment.
Conclusion. The high prevalence of CKD in the cohort of HF patients, the identified diagnostic problems, a more severe clinical course of HF, and an unfavorable prognosis emphasize the need for comprehensive measures to increase physician awareness and optimize the implementation of guidelines in real-world practice.
- Type 2 diabetes (T2D) occurs in almost a third of outpatients with heart failure (HF).
- Among patients with HF, there is T2D underdiagnosis by the level of glycated hemoglobin (HbA1c) and insufficient glycemic control in the established T2D.
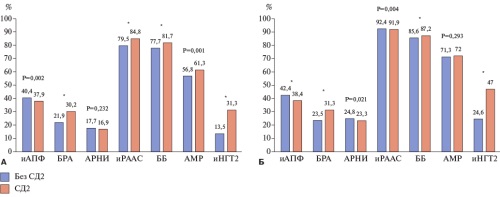
- Patients with T2D were characterized by a more severe HF course, more often received angiotensin II receptor blockers, beta-blockers, sodium-glucose cotransporter-2 inhibitors and had higher titration rates of guideline-directed medical therapy.
- T2D worsens the prognosis of patients with HF. In T2D, HbA1c >9% was associated with an unfavorable prognosis.
Aim. To assess the prevalence, clinical features and prognostic value of type 2 diabetes (T2D) in outpatients with heart failure (HF).
Material and methods. According to the PRIORITY-HF study, a retrospective analysis of T2D prevalence, features of control and treatment of related comorbid conditions was performed in a cohort of 19939 patients with HF. The prognostic role of T2D and glycated
hemoglobin (HbA1c) was estimated using the multivariate Cox regression model. Results. The prevalence of T2D in patients with HF was 27,4%. The HbA1c level at visit 1 was determined in 37,6% of patients with T2D and in 11,6% of cases without T2D. Patients with T2D compared to those without T2D were characterized by a higher burden of cardiovascular comorbidities and such non-cardiac concomitant conditions as chronic kidney disease, anemia, bronchial asthma. Patients with T2D had a higher functional class, longer duration of HF, and a greater HF-related hospitalization rate. At baseline, T2D was associated with more frequent prescription of angiotensin II receptor blockers, renin-angiotensin-aldosterone system blockers, mineralocorticoid receptor antagonists, beta-blockers, sodium-glucose cotransporter-2 (SGLT2) inhibitors. After visit 1, both subgroups showed a prescription rate increase in all classes of guideline-directed medical therapy (GDMT), especially SGLT2 inhibitors. The proportions of patients receiving target GDMT doses were low in both subgroups with and without T2D, but titration of doses of all GDMT classes was more effective among patients with T2D. Metformin was most often used for glycemic control, followed by SGLT2 inhibitors and sulfonylureas, which are not front-line therapy for HF. Patients with T2D were characterized by a more unfavorable prognosis compared to the cohort without T2D. In the subgroup of patients with T2D, HbA1c >9% was associated with an increased all-cause mortality, as well as all-cause and HF-related hospitalization rates.
Conclusion. T2D in patients with HF is associated with a more severe HF course, worsens the prognosis and requires increased awareness of physicians on the diagnostic and therapeutic tactics for managing this cohort of patients.
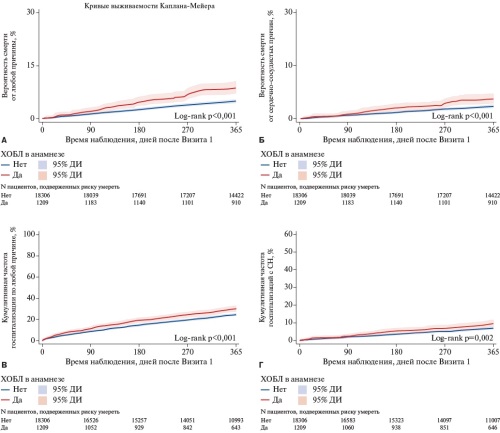
- Low incidence of chronic obstructive pulmonary disease (COPD) in the outpatients with heart failure (HF) may be due to underdiagnosis, especially among those with preserved or mildly reduced ejection fraction.
- The combination of HF with COPD is characterized by a more severe course of HF and a higher intake rate of guideline-directed medical therapy.
- Patients with HF and concomitant COPD have a worse prognosis for all-cause mortality and hospitalizations compared to patients without COPD.
Aim. To assess the prevalence, clinical features and prognosis of heart failure (HF) combined with chronic obstructive pulmonary disease (COPD) according to the prospective observational multicenter registry study of Russian patients with HF — PRIORITY-HF.
Material and methods. The study included 19981 patients from 136 centers. Case report form was used to collect and analyze primary data. During the follow-up period, additional visits to the study centers were conducted at 6 and 12 months. Results. Overall prevalence of COPD in the examined cohort was 6,2%, while with HF with reduced (HFrEF), mildly reduced (HFmrEF) and preserved ejection fraction (HFpEF) it was 7,5%/5,7%/5,4%, respectively (p<0,001). Patients with a combination of HF and COPD compared to the group without COPD were found to have a more severe course of HF as follows: a higher NYHA functional class, a longer duration of HF (24 months vs 23,6 months, p=0,001) and higher HF-related hospitalization rate in history (41,7% vs 31,4%, p<0,001). Comorbid conditions such as hypertension, coronary artery disease, atrial fibrillation, peripheral arterial disease, cerebrovascular disease, chronic kidney disease, and anemia were more frequently recorded in the group with concomitant COPD. Sodium-glucose cotransporter-2 inhibitors, angiotensin receptor-neprilysin inhibitors, mineralocorticoid receptor antagonists, and quadruple therapy were used more frequently in the overall cohort with COPD compared to patients without COPD (p<0,001). The multivariate model demonstrated a more unfavorable prognosis for patients with concomitant COPD regarding all-cause mortality and hospitalizations (odds ratio (OR) 1,304, 95% confidence interval (CI) (1,046-1,625), p=0,018; OR 1,128, 95% CI (1,004-1,266), p=0,042).
Conclusion. A low incidence of COPD was found in the outpatient cohort of patients with HF, which may be associated with underdiagnosis in real-world practice. Patients with a combination of HF and COPD had a more severe course of HF, more often used the main classes of guideline-directed medical therapy and quadruple therapy, and a higher risk of all-cause mortality and hospitalizations during 12-month follow-up.
- In 79,8% of patients with hypertension (HTN) and markers of chronic kidney disease (CKD), the diagnosis of CKD was confirmed during the study; in 42,5% — according to retrospective data.
- There is extremely low rate of using urinary markers of renal involvement for CKD diagnosis.
- Overdiagnosis and underdiagnosis of CKD are due to insufficient examination and incorrect assessment of CKD markers.
- The study shows following findings: women predomination; long HTN history; predomination of stage III HTN and very high cardiovascular risk.
- A serious burden of metabolic risk factors and atherosclerotic cardiovascular diseases was revealed.
- There is a high rate of renin-angiotensin-aldosterone blockers prescription, and after CKD verification 24,5% patients were prescribed the sodium-glucose co-transporter type 2 inhibitors.
Aim. To describe the detection rate of chronic kidney disease (CKD) in patients with hypertension (HTN) and markers of CKD without concomitant diabetes and symptomatic heart failure, as well as to describe the clinical and demographic characteristics and features of therapy in the overall cohort and a subgroup with verified CKD.
Material and methods. The article presents an interim analysis of data from a prospective observational multicenter study of patients with HTN and CKD in the Russian Federation (PRIORITY-CKD).
Results. Data from the first 3249 patients included in the study were analyzed. In 2592 (79,8%) patients with HTN and CKD markers, the diagnosis of CKD was confirmed during the study as follows: in 1380 (42,5%) at Visit 1 and in 1212 (37,3%) at Visit 2. In 2488 (96%) cases, only the estimated glomerular filtration rate was used as the criteria for the diagnosis of CKD. Only in 12 patients (0,5%) albuminuria or proteinuria (alone or together with other CKD markers) was used as diagnostic criteria for CKD diagnosis. Cases of overdiagnosis (12,6%) and underdiagnosis (0,4%) of CKD were identified. In the overall cohort and the subgroup with verified CKD, women predominated (61,6/62,1%), while the median duration of HTN was 9 and 10 years, respectively. More than half of the patients had stage III HTN and very high cardiovascular risk. A high rate of metabolic risk factors (overweight, dyslipidemia, abdominal obesity) and atherosclerotic cardiovascular diseases was noted. Coronary artery disease was observed in a third of patients in the overall cohort and the CKD subgroup. Uncontrolled HTN (systolic BP ≥140 and/or diastolic BP ≥90 mm Hg despite antihypertensive therapy) and resistant HTN were detected in 42,5% and 6,7% of patients in the overall cohort, while in the subgroup with CKD in 42,1% and 7,3%, respectively. Combination antihypertensive therapy after Visit 1 was received by 78,8% of patients in the examined cohort. Only in 21,4% of cases, sodium-glucose cotransporter-2 inhibitors were prescribed after verification of the CKD diagnosis.
Conclusion. In the Russian population, the diagnosis of CKD was confirmed in 79,8% of patients with HTN and CKD markers. Albuminuria/proteinuria was assessed extremely rarely. Cases of overdiagnosis and underdiagnosis of CKD were identified. A high rate of uncontrolled HTN and a serious burden of atherosclerotic cardiovascular diseases were observed in the overall cohort and the subgroup with CKD. After CKD verification, a suboptimal increase in the prescription of sodiumglucose cotransporter-2 inhibitors was noted.
ISSN 2618-7620 (Online)