ORIGINAL ARTICLES
- In most cases, patients with hypertension and multifocal atherosclerosis do not achieve target lipid parameters due to low intensity of lipid-lowering therapy.
- This may increase the residual risk of various vascular events due to the close relationship between lipid metabolism and global coagulation parameters and inflammation markers.
- Treatment of identified disorders will help prevent cardiovascular events.
Aim. To establish the relationship between lipid profile parameters, coagulation system and inflammation markers in patients with hypertension (HTN) and multifocal atherosclerosis (MFA).
Material and methods. The study included 110 patients with HTN and MFA with a median age of 59 (51,0;64,3) years. Of these, 15 patients achieved target lowdensity lipoprotein cholesterol (LDL-C) <1,8 mmol/l (group 1), and 95 patients had LDL-C >1,8 mmol/l (group 2). Patients in both groups received lipid-l owering and comparable antihypertensive, antiplatelet therapy. To identify coagulation disorders, a test was performed on the T-2 Thrombodynamics Analyser System (OOO GemaCor, Moscow, Russia). All study participants were assessed for levels of high-sensitivity C-reactive protein and interleukin-6.
Results. Despite the lipid-l owering therapy, most patients with HTN and MFA (86,4%) did not achieve target LDL-C <1,8 mmol/l. In patients of group 2, compared to group 1, more pronounced procoagulant shifts were noted. The clot growth rate and the permanent clot growth rate were shifted to the hypercoagulation (28,6 μm/min vs 27 μm/min). Correlations between the studied parameters were also revealed. In group 1, the LDL-C level had a moderate direct correlation with the initial clot growth rate (r1=0,54, p1=0,04) and clot density (r1=0,55, p1=0,03), while in group 2, the concentrations of total cholesterol and LDL-C correlated with clot growth delay (r2=-0,22, p2=0,03 and r2=-0,21, p2=0,04, respectively).
Conclusion. In patients with HTN and MFA, complex relationships between lipid parameters, coagulation parameters, and inflammatory markers are observed, especially in the group with unachieved lipid target levels. Extra efforts are needed to identify patients with HTN and MFA in clinical practice and to prescribe optimal lipid-lowering therapy. In addition to lipid parameters, correction of other disorders (hemostasis, inflammation) that may affect the prognosis is necessary.
- Most patients with heart failure (HF) aged ≥60 years have 2 or more comorbidities and take 6 or more medications.
- Outpatients with HF aged ≥60 years, regardless of the left ventricular ejection fraction (EF), have a suboptimal adherence level, requiring interventions aimed at improving it.
- Medication adherence is significantly lower in HF with preserved EF than in those with mildly reduced and reduced EF.
Aim. To assess clinical characteristics and medication adherence in patients with heart failure (HF) with different left ventricle ejection fractions (LVEF).
Material and methods. The study involved 65 outpatients aged ≥60 years with a verified diagnosis of HF. A standard physical examination, laboratory and echocardiographic studies were performed. Adherence to treatment was assessed using the National Society of Evidence-B ased Pharmacotherapy Adherence Scale. A patient was considered to have complete adherence with a score of 0, incomplete adherence — ≥1.
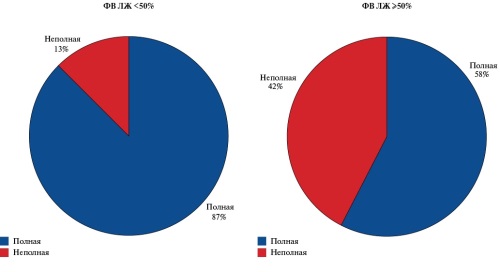
Results. Preserved LVEF (≥50%) was present in 33 (50,8%) patients (mean age, 76,2±6,6 years). Mildly reduced and reduced LVEF (<50%) was recorded in 32 (49,2%) patients aged 69,8±7,7 years. Regardless of the LVEF, all patients (100%) had two or more chronic diseases, while 45,5% of patients with LVEF ≥50% and 53,1% of patients with LVEF <50% took six or more medications. Most patients took beta-blockers (78,8% in the group with LVEF ≥50%; 87,5% in the group with LVEF <50%), while in isolated cases — angiotensin receptor- neprilysin inhibitors (3% of patients with preserved LVEF; 6,3% — with reduced and moderately reduced LVEF). At the same time, no patient with HF took quadruple therapy. Full adherence to treatment was found in 87,5% of patients in the group with LVEF <50% and in 57,6% in the group with LVEF ≥50%, p=0,007. As the leading reason for noncomplete adherence to treatment, most patients (61,1%) indicated forgetfulness.
Conclusion. Complete adherence rate in outpatients with HF with preserved EF is lower than in patients with reduced and mildly reduced EF. Regardless of LVEF, patients with HF require measures to improve medication adherence
- End-stage heart failure refractory to therapy is an indication for implantation of a left ventricular assist device (LVAD).
- Based on our own experience of 6-month follow-up of patients with LVAD, its effectiveness, mortality, main postoperative complications and their causes were analyzed.
- A conclusion was made about the need for more careful selection of patients for intervention to improve the outcomes.
Aim. To study mortality, postoperative complications, clinical course, and quality of life of patients with heart failure (HF) within 6 months after left ventricular assist device (LVAD) implantation.
Material and methods. The study included 53 patients who met the criteria for LVAD implantation. Twenty three patients underwent surgery (group 1), while 30 patients refused implantation (group 2). The follow-up period was 6 months. The death number and causes, hospitalization and HF decompensation rates, the changes of N-terminal pro-brain natriuretic peptide levels, the functional class of HF, the incidence of postoperative complications were assessed. Exercise tolerance (ET) was determined using a 6-minute walk test, while quality of life — using the EQ-5D questionnaire.
Results. Patient mortality in the LVAD group was 26%, while in group 2 — 23,3%. In the main group, 1 patient died due to cardiovascular cause; 2 — gastrointestinal bleeding; 1 — infectious complications (sepsis); 1 — cerebrovascular accident; 1 — acute non-occlusive mesenteric ischemia. In the control group, all death cases were due to cardiovascular pathology. Among the complications after implantation, the most common were pleurisy, delirium, ventricular tachycardia, right ventricular failure, gastrointestinal bleeding, LVAD-associated infection. In group 1, there was a significantly lower number of rehospitalizations compared to group 2, including those due to HF decompensation (p=0,034, p<0,001, respectively). In the main group, there was an improvement in the quality of life (p<0,001), HF class (p<0,001), and ET (p=0,006), which led to a reliable difference between the groups after 6 months.
Conclusion. LVAD implantation is accompanied by a decrease in the number of rehospitalizations and HF decompensation, as well as improvement of ET, HF class and quality of life of patients, but not a decrease in mortality. To reduce the incidence of postoperative complications and improve the prognosis, a more careful selection of patients for intervention, assessment of their cognitive status and compliance is necessary.
- In patients with non-obstructive coronary artery disease, according to adenosine triphosphate stress computed tomography myocardial perfusion, qualitative and semi-quantitative analysis of perfusion defects demonstrated a decrease in the transmural perfusion coefficient segmentally and globally. In addition, there was a relationship between the left ventricular myocardial ischemia volume and ST depression according to Holter monitoring, and no correlation with atherosclerosis risk factors.
Aim. To assess the relationship between left ventricular (LV) myocardial perfusion parameters according to adenosine triphosphate (ATP) stress computed tomography myocardial perfusion (CTP) with clinical parameters in patients with non-obstructive coronary artery disease (CAD).
Material and methods. ATP CTP was performed in 74 patients with documented non-obstructive CAD. Myocardial perfusion was assessed using qualitative and semiquantitative methods. The volume of myocardial ischemia was assessed depending on the number of segments with perfusion defects. The study protocol included assessment of LV myocardial perfusion at rest and in stress with ATP administration at a constant rate of 0,16 mg/kg/min, for a total duration of 4-5 min. All patients underwent the following examinations: electrocardiography, Holter monitoring, echocardiography, blood tests. The results of myocardial perfusion were compared with age, sex, atherosclerosis risk factors, angina clinical picture, and the results of additional examination methods.
Results. Transient LV myocardial perfusion defects were visualized in 100% of patients during ATP CTP with subendocardial location of varying severity. The transmural perfusion coefficient (TPС) was significantly reduced globally and segmentally in the stress phase in all patients (p<0,0001). ST segment depression according to Holter monitoring was associated with a greater LV ischemia volume. When dividing patients into 3 groups depending on the number of affected segments, no significant differences were found according to the intergroup analysis between the LV myocardial ischemia volume and the average values of atherosclerosis risk factors.
Conclusion. LV myocardial perfusion defects were detected in 74 patients with an established non-obstructive CAD. No significant differences were found between the LV myocardial ischemia volume and the main risk factors for atherosclerosis, but there was an association between ST segment depression and LV myocardial ischemia volume, a significant decrease in global and segmental TPC with ATP stress test.
- Patients develop atrial fibrillation after endovascular patent foramen ovale closure.
- Age over 52 years, excess body weight, and left atrial dilation are risk factors for atrial fibrillation.
One of the known potential complications associated with endovascular closure of the patent foramen ovale (PFO) is de novo atrial fibrillation (AF).
Aim. To assess the risk factors and incidence of de novo AF in patients who underwent endovascular PFO closure.
Material and methods. The data of 276 patients who underwent endovascular PFO closure for the period from 2020 to 2023 at the Chazov National Medical Research Center of Cardiology were analyzed. All patients underwent examinations in accordance with clinical guidelines. De novo AF in the postoperative period was assessed by Holter monitoring, while 1, 6 and 12 months after the intervention — by electrocardiographic recording. Based on univariate regression analysis, risk factors associated with de novo AF were identified.
Results. De novo AF in the postoperative period was registered in 2 patients. One month after the intervention, AF episodes were diagnosed in 6 patients. After 6 months, AF detected earlier persisted in 3 patients,and there were 3 new cases. Twelve months after the intervention, AF was recorded in 2 patients. According to regression analysis, the following parameters were associated with de novo AF: age ≥52,0 years (hazard ratio (HR) 6,22; 95% confidence interval (CI): 1,51-25,56), body mass index ≥28,07 kg/m2 (HR 8,48; 95% CI: 1,72-41,73), CHARGE-AF score ≥0,56 (HR 4,59; 95% CI: 1,12-18,82), left atrial size ≥4,00 cm (HR 19,56; 95% CI: 2,10-181,88), LAVi ≥34 ml/m2 (HR 45,67; 95% CI: 5,46-381,83) according to echocardiography.
Conclusion. Echocardiographic signs of left atrial and left ventricular dilation were significantly associated with a high risk of de novo AF in the immediate and longterm periods after endovascular PFO closure.
- The Ex-PRO score for predicting long-term complications in extrasystole includes the following parameters: type IIIB plaque in the carotid bifurcation (5 points), extrasystole before the peak of transmitral blood flow ≥700 (4 points), hemodynamically insignificant carotid bifurcation stenosis (4 points), female sex (2 points), left ventricular impaired local contractility (2 points), hemodynamically insignificant lower limb stenosis (1 point).
Aim. To create a score for predicting arterial events (myocardial infarctions, strokes, ischemic events in other arterial systems) in patients with extrasystole.
Material and methods. The study included 740 patients (634 — the main group, 106 — control). The main group had 700 or more premature beats per day, and the control group had <700 premature beats. The main group was divided into two subgroups depending on the phase of the biomechanical cardiac cycle in which the ventricular systole of the extrasystolic contraction occurred — before (I — n=192) or after (II — n=442) the peak E on echocardiography. Standard laboratory (including blood lipid profile, coagulation test) and clinical investigations were performed. The prospective study was conducted for 1 year from the first visit moment. There were following endpoints: arterial events (myocardial infarction, stroke, ischemic events in other arterial systems).
Results. At the first visit, the groups of patients were equivalent in comorbidities, prior events, data from additional research methods. However, a significantly higher prevalence of ischemic events within 1 year was revealed in subgroup II. The creation of an original Ex- PRO score for predicting long-term complications with premature beats ≥700 or more per day made it possible to predict ischemic events in this category of patients (prediction accuracy 87,1%).
Conclusion. Extrasystole is an additional factor in the development of arterial events in various arterial systems. Ex- PRO includes the following parameters: type IIIB plaque according to extracranial Doppler ultrasound, extrasystole up to the peak transmitral flow ≥700 per day, hemodynamically insignificant carotid bifurcation stenosis according to extracranial Doppler ultrasound, female sex, impaired left ventricular local contractility, hemodynamically insignificant lower limb artery stenosis.
- Coronary artery disease (CAD) is the leading cause of death worldwide. There are no studies assessing mortality specifically from chronic types of CAD.
- Significant differences between men and women are recorded in the standardized mortality rates, but not the unstandardized death rates. The share of CAD in all-cause mortality is the same for men and women. The share of deaths from CAD in women over 80 years of age reaches 60%, while in men — 23%. A significant change in the structure of CAD by ICD codes in the period of 2014-2023 is probably due to the declining criteria (including postmortem) for diagnosing each form of CAD.
- Clarification by clinicians of the criteria for chronic CAD types will contribute to a better understanding of the death causes, and develop targeted prevention and treatment programs.
Aim. To assess the dynamics of non-standardized (NSMR) and standardized mortality rates (SMR) of chronic coronary artery disease (CAD), the contribution to all-cause mortality, as well as the dynamics and structure of chronic CAD among men and women in the Russian Federation in 2014-2023.
Material and methods. Rosstat data on mortality in one-year age groups of patients for 2014-2023 in accordance with the Rosstat Brief Nomenclature of Death Causes. The calculations were performed using the program (certificate of state registration of the computer program dated September 30, 2016, № 201666114). The European standard (European Standard Population, 1976) was used to calculate the SMR.
Results. A decrease in the SMR from chronic CAD was found in both women (2014 — 147,6 per 100 thousand population, 2023 — 126 per 100 thousand population) and men (2014 — 275 per 100 thousand population, 2023 — 221 per 100 thousand population). The NCMR differences in men and women did not exceed 5%, while the SMR from chronic CAD differed by almost 2 times due to the age disproportion (in age ≥80 years in women, there were 60% of deaths from chronic CAD, while in men — 23,6%). The proportion of chronic CAD in all-cause mortality in men was 23,9%, while in women — 23,4%. The highest values of SMR were recorded from "I25.1 Atherosclerotic heart disease" (the proportion in the chronic CAD structure in 2014 in women — 64,5%, in men — 56,8%; in 2023 — 60,4% and 51,4%, respectively). In both men and women, the SMR and the proportion of "I25.2-6,8 Other forms of chronic CAD" in the structure of SMR from chronic CAD increased (in 2014 in women — 21,5%, in men — 29,3%, in 2023 — 37% and 46%, respectively). The SMR from I25.0 and I25.9 significantly decreased, amounting to <4% in the structure of chronic CAD in both men and women in 2023.
Conclusion. The obtained results indicate problems with defining individual forms of chronic CAD as the underlying cause of death, which complicates understanding the death causes. It is necessary to consider creating uniform guidelines for the Russian Federation, where the classification of chronic CAD according to ICD-10 would be adapted to the clinical terminology and the most probable clinical variants, as well as the main principles of morphological classification. Typification of coding approaches will serve to improve the quality of analysis of chronic CAD mortality statistics data and subsequent adoption of targeted management decisions.
ISSN 2618-7620 (Online)