CLINICAL CASES
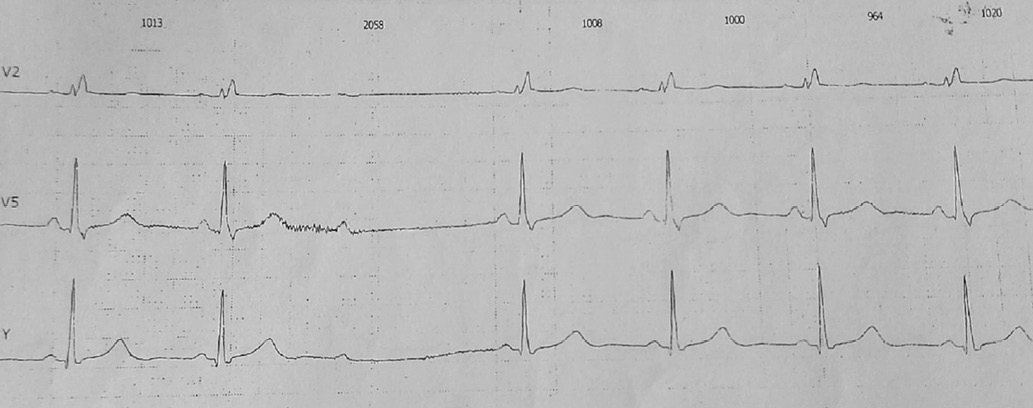
- Primary cardiac lymphomas are a rare pathology with non-specific manifestations, including heart failure, cardiac arrhythmias and conduction disorders.
- The case of an 88-year-old female patient with right atrial B-cell lymphoma, previously undiagnosed during examination before pacemaker implantation for third-degree atrioventricular block, is presented.
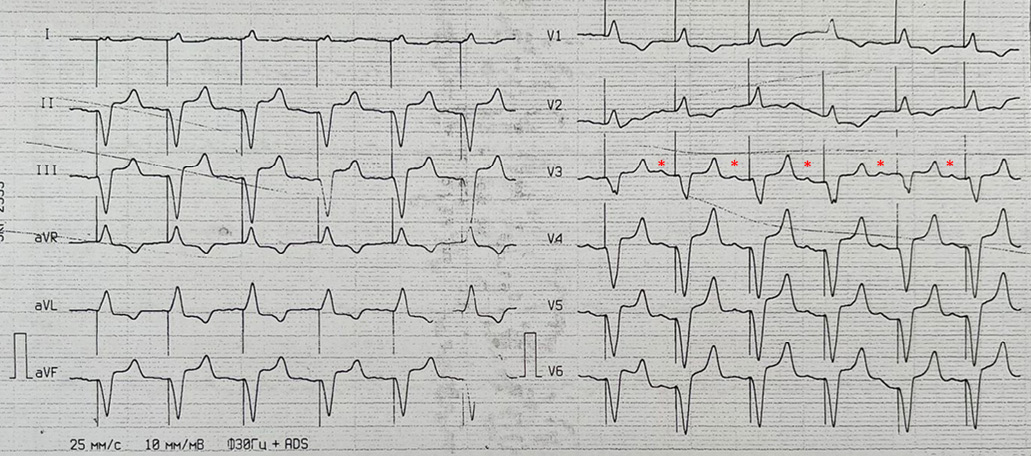
- Electrocardiographic performance is interesting (signs of right, not left bundle branch block in right ventricular pacing). The difficulties in interpreting echocardiographic manifestations of the disease are also described.
- The second finding at autopsy was clear cell renal cell carcinoma, also previously undiagnosed during echocardiographic examination.
Introduction. Primary cardiac lymphomas are a rare pathology that presents certain diagnostic difficulties. In addition to chemotherapy, an important aspect of such patients is arrhythmias and conduction disorders. Indications for pacemaker implantation and timing of the intervention in such situations continue to be discussed.
Brief description. A case of right atrial (RA) B-cell lymphoma in an elderly female patient is presented. The patient had previously been examined for bradycardia and presyncope. Third-degree atrioventricular (AV) block and complete left bundle branch block were detected, followed by a dual-chamber pacemaker implantation. Apparently, conduction disorders were caused by tumor growth in the AV node area. However, paraclinical signs could not be identified at that time. Three weeks later, the patient was hospitalized due to hypotension and coma. The specific electrocardiographic performance (signs of right, not left bundle branch block in right ventricular pacing) required assessment for lead displacement and cardiac perforation. Echocardiography revealed para-aortic hyperechoic cavities with heterogeneous contents, linear shadows in the aortic valve cusp coaptation area, interpreted as aortic root abscess or aortic aneurysm, and manifestations of infective endocarditis. The RA tumor was diagnosed only at autopsy. The second finding was clear cell renal cell carcinoma, which had also not been previously detected by echocardiographic examination.
Discussion. A case of a rare combination of two tumors demonstrates the difficulties in diagnosing cardiac lesions and emphasizes the importance of their early recognition even when manifested by non-specific symptoms.
- The case clearly describes a patient with arrhythmogenic mitral valve prolapse.
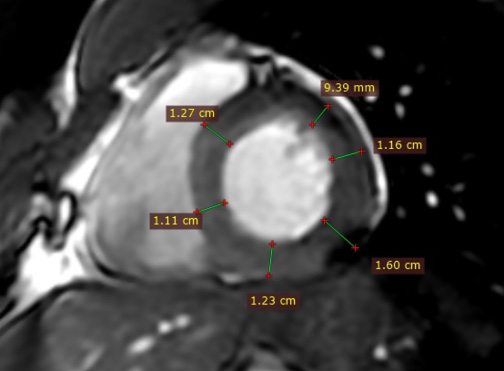
- A description of mitral annular disjunction and cark papillary muscles sign is provided.
Introduction. Recently, a subgroup of patients with mitral valve prolapse has been identified with an increased risk of ventricular arrhythmias and sudden cardiac death. One of the most characteristic signs of the arrhythmogenic mitral valve prolapse is mitral annular disjunction, detected by transthoracic or transesophageal echocardiography or by cardiac magnetic resonance imaging. Clinical and imaging data are used to stratify the risk of ventricular arrhythmias and determine patient management strategy.
Case report. The article presents a case of a young man with arrhythmogenic mitral valve prolapse. The case demonstrates the anatomical features of mitral valve and related subvalvular structures, and also considers their impact on cardiac arrhythmias. Particular attention is paid to the description of mitral annular disjunction and dark papillary muscles sign.
Conclusion. One of the tasks for imaging diagnostics in patients with ventricular arrhythmias and mitral valve prolapse is the assessment of phenotypic risk factors. Given the relationship of mitral annular disjunction with mitral valve prolapse, the development of mitral insufficiency and association with life-threatening ventricular arrhythmias, its timely diagnosis and follow-up of patients are extremely important.
- Myocardial infarction can be associated with chronic inflammatory and cancer diseases, being the first reason for seeking medical help.
- Chronic inflammatory bowel diseases, polycythemia vera are associated with a high risk of thrombosis.
- A case demonstrates the development of myocardial infarction in a patient with ulcerative colitis and polycythemia vera, and draws attention to the importance of a systemic approach to the diagnosis and treatment of such comorbid patients.
Introduction. Myocardial infarction (MI) developing before the age of 45 is not casuistic, but is often associated with conventional risk factors, chronic non-cardiac diseases, being the first reason for seeking medical help. Patients with inflammatory bowel diseases are at increased risk of cardiovascular diseases, gastrointestinal cancer, and extraintestinal cancer, including myeloproliferative neoplasms. A common genetic predisposition to myeloproliferative and inflammatory diseases, including inflammatory bowel disease, is described. In contrast, myeloproliferative diseases are often associated with abdominal pain syndrome, thrombosis of various locations.
Brief description. We describe a case of a 40-year-old man with MI at the start of corticosteroid and mesalazine therapy for newly diagnosed ulcerative colitis. Percutaneous coronary angioplasty with stenting of the anterior descending artery was performed. The early postoperative period was complicated by acute stent thrombosis, which required repeated stenting and intra-aortic balloon counterpulsation. Despite the 1-year dual antiplatelet therapy (DAPT) after discharge from the hospital, intestinal bleeding did not relapse against the background of treatment of ulcerative colitis. Immunosuppressive therapy included azathioprin. Glucocorticosteroid therapy was discontinued due to high risk of thrombosis. Anti-inflammatory therapy was carried out with mesalazine. During hospitalization, thrombocytosis was diagnosed for the first time. Hematologist diagnosed JAK+ polycythemia vera, and cytoreductive therapy with hydroxyurea was prescribed.
Discussion. MI was obviously associated with thrombosis against the background of chronic myeloproliferative disease and inflammatory bowel disease. Management of such patients is difficult due to the high risk of thrombotic and hemorrhagic events. DAPT was not associated with bleeding. Myeloproliferative diseases, inflammatory bowel diseases should be taken into account in patients with early onset of coronary artery disease for their timely diagnosis and development of a secondary prevention plan.
More than 100 million women use combined oral contraceptives to prevent unintended pregnancy, as well as for a number of other medical indications. Taking estrogen and progestin drugs is associated with the risk of acute thromboembolic and vascular events. This is a consequence of an increase in serum coagulation factors and a direct effect on endothelial dysfunction, which enhances platelet aggregation. This article demonstrates the development of myocardial infarction and pulmonary embolism in a young man during feminizing therapy.
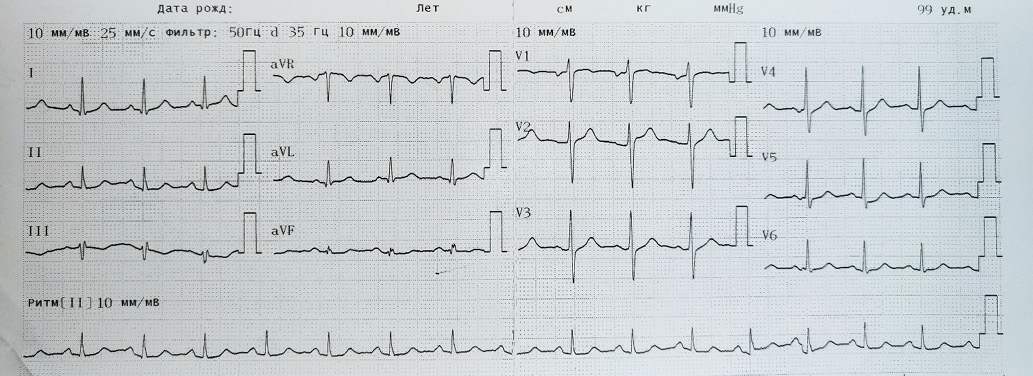
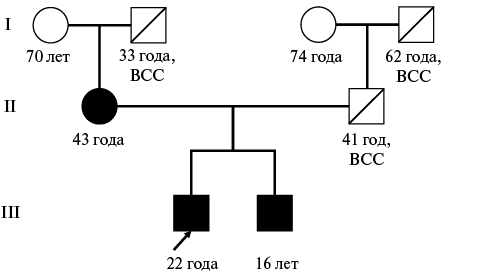
- Stratification of sudden cardiac death risk, collection of family history, assessment of echocardiographic parameters and 24-hour electrocardiographic monitoring data is a key task in the prevention of fatal arrhythmias in young patients.
- The combination of ACTC1 and LDB3 gene mutations may be associated with biventricular myocardial hypertrophy and myocardial bridging, which requires confirmation using a larger number of observations.
Introduction. Hypertrophic cardiomyopathy (HCM) significantly increases the risk of sudden cardiac death (SCD), especially in young patients. Familial HCM requires an individual approach to risk stratification and determining indications for primary prevention of SCD.
Brief description. This case describes a patient with a rare genetic anomaly (a combination of ACTC1 and LDB3 mutations). Thanks to timely diagnosis, indications for a cardioverter-defibrillator implantation were determined, which made it possible to stop an episode of ventricular fibrillation (VF). The case describes the changes of the patient's echocardiographic parameters, morphological features (biventricular myocardial hypertrophy, myocardial bridge), as well as the disease course, therapeutic approaches and 6-year treatment outcomes.
Discussion. Careful stratification of SCD risk, including assessment of family history, constant monitoring with dynamic echocardiography and Holter monitoring, allowed timely implantation of a cardioverter-defibrillator and stopping VF. Preventive measures, continuity between the inpatient and outpatient stages saved the patient's life, improved the prognosis and slowed the progression of left ventricular hypertrophy. A rare genetic variant of HCM with mutations in the ACTC1 and LDB3 genes has been described in only three cases over 5 years, which emphasizes the scientific significance of this case. The combination of biventricular hypertrophy, myocardial bridge, and episodes of ventricular tachycardia and VF may be associated with this genotype, which requires further study to improve SCD risk management strategies.
- The combination of hypertrophic cardiomyopathy and infective endocarditis is quite rare.
- The main diagnostic method for this condition is echocardiography.
- Treatment of this group of patients requires an individual approach. Depending on the location and area of involvement, the scope of treatment may include antibiotic therapy, lavage of heart cavities, replacement of affected valves, as well as treatment of hypertrophy by septal myectomy.
- This case demonstrates the difficulties in timely diagnosis of endocarditis in a patient with hypertrophic cardiomyopathy and is aimed at developing greater clinical alertness among colleagues.
Infective endocarditis in patients with hypertrophic cardiomyopathy is a rare clinical combination. However, this combination of diseases increases the already high risk of death in patients with hypertrophic cardiomyopathy. In this regard, early diagnosis of this pathology, timely antibacterial therapy, and, if necessary, surgical treatment are necessary. The article describes a clinical case.
- The presented case reports demonstrate the significance of patent for a men ovale in ischemic stroke in young patients without other risk factors.
- In the case of cryptogenic stroke, it is of great importance to identify a right-to-left cardiac shunt using all available diagnostic methods.
- Primary care physicians should be informed about the association of patent foramen ovale and neurological diseases, primarily stroke, the risk of paradoxical embolism, and primary and secondary prevention measures.
Introduction. Causal relationship between minor congenital heart defects and neurological pathology remains a relevant and debatable issue.
Brief description. Two cases of ischemic stroke of different locations associated with patent foramen ovale (PFO) are presented in patients aged 20 and 32 years without other risk factors.
Conclusion. In both cases of cryptogenic stroke, an examination for PFO by transesophageal echocardiography and bilateral cerebral microemboli monitoring were performed. Diagnosis of a right-to-left shunt in the first case was difficult and required a repeat bubble and transesophageal echocardiography with contrast enhancement and the Valsalva maneuver. Confirmation of functioning PFO allowed us to clarify the pathogenetic variant of stroke, determine the tactics of treatment and secondary prevention measures.
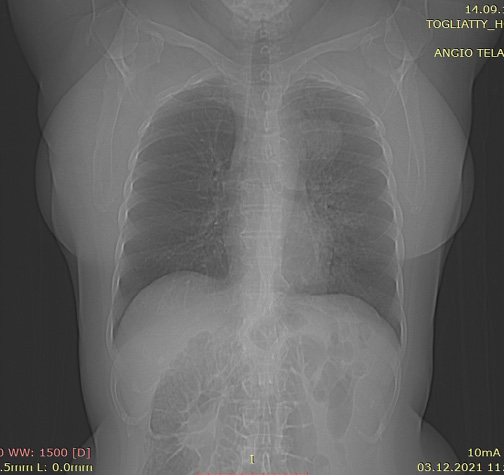
- Combination of pulmonary embolism and aortic dissection is extremely rare; their diagnosis in conditions of non-specific manifestations requires a clinical approach using paraclinical methods.
- A case of a combination of massive pulmonary embolism and aortic dissection is presented, illustrated by paraclin-ical examination and autopsy data in a 42-year-old male patient with hypertension, obesity and gout.
- Treatment of such combination is extremely difficult even with timely diagnosis, since the use of antithrombotic agents in pulmonary embolism is absolutely contraindicated in aortic dissection, and cases of successful surgical treatment are extremely rare.
The article describes a rare case of lifetime diagnosis of a combination of massive pulmonary embolism and aortic dissection (DeBakey type I, Stanford type A) in a 42-year-old male patient with hypertension, obesity and gout. The combination of these potentially fatal pathologies, even with timely diagnosis, significantly complicates the choice of treatment strategy, since the use of antithrombotic agents for pulmonary embolism is absolutely contraindicated in aortic dissection, and successful surgical treatment in these cases are extremely rare.
The case is illustrated by paraclinical examination and autopsy data.
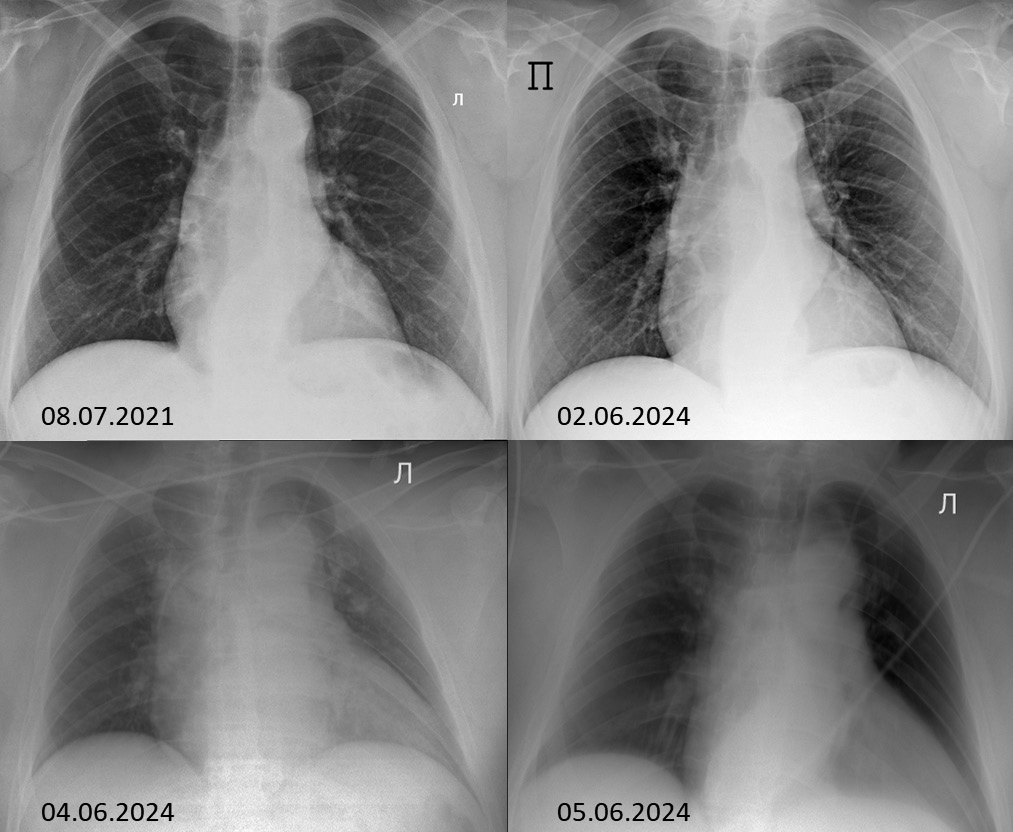
- Pulmonary hemorrhage is a rare complication of aortic aneurysm.
- Timely assessment of hemoptysis (pulmonary hemorrhage) severity and determination of the cause is a decisive stage in determining the proper treatment tactics.
- Surgical intervention only on the aorta without involving lung allows eliminating such a complication as pulmonary hemorrhage.
Introduction. Pulmonary hemorrhage is one of the life-threatening complications of some respiratory diseases. Rarely, it is a complication of an aortic aneurysm. In this case, the life risk is greater compared to other causes of pulmonary hemorrhage.
Brief description. A patient with an aortic arch aneurysm developed pulmonary hemorrhage as a result of damage to left lung apex tissue. The patient underwent urgent on-pump aortic arch replacement with circulatory arrest. The postoperative period was uneventful, and on the 14th day she was discharged in a satisfactory condition. In control examination 26 months after the surgery, the condition was satisfactory, and the patient returned to normal life. Control chest computed tomography revealed no pathology.
Discussion. Limiting surgical intervention only to the aorta in this patient allowed treating pulmonary hemorrhage without intervention on the lung tissue.
CLINICAL OBSERVATION
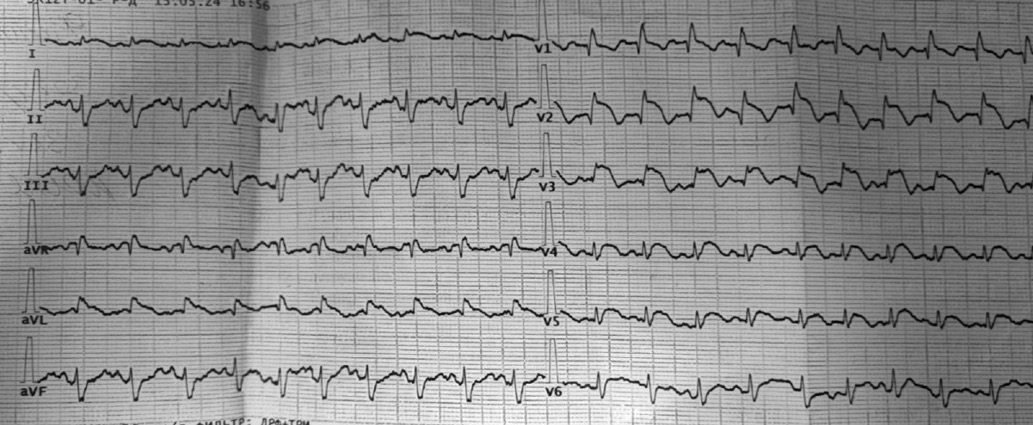
Introduction. The problem of pacemaker implantation in atrioventricular (AV) block remains relevant, which creates conditions for a collegial approach taking into account personalized medicine in each specific case.
Brief description. A 70-year-old female patient was observed by an arrhythmologist for 9 months with second-degree type II AV block with transient third-degree AV block according to 24-hour electrocardiographic monitoring. A decision was made to implant a pacemaker, but the patient refrained from elective hospitalization. A detailed examination revealed that she was taking plaquenil and methylprednisolone as baseline therapy for collagenosis. Upon agreement with the rheumatologist, plaquenil was discontinued and the metypred dose was adjusted. Subsequently, the clinical condition remained without significant changes. However, according to the monitoring results, significant improvement was noted.
Discussion. This case demonstrates the need for a physician to take into account all patient data when prescribing treatment. Also, based on the considered case, the authors proposed a model for predicting fatal complications when detecting conduction disorders.
ISSN 2618-7620 (Online)