ORIGINAL ARTICLES
Aim. To study clinical, laboratory and psychological aspects of moderate coronavirus disease 2019 (COVID-19) in cardiovascular patients one month after discharge from the hospital.
Material and methods. The study included 88 patients with cardiovascular diseases hospitalized for COVID-19. After 1 month, 72 respondents continued the participation in the study. Medical history collection, physical examination, and diagnostic investigations were performed. We used the Hospital Anxiety and Depression Scale (HADS) by Zigmond A. S., Snaith R. P., Beck Anxiety Inventory scale, Mini-mental State Examination (MMSE) scale for assessing mental status.
Results. One month after discharge, there was a decrease in the number of patients with signs of impaired respiratory system, such as cough, shortness of breath, chest congestion, while a decrease in exercise tolerance persists was revealed in 80,5% (out of 95,5% during hospiatalization), generalized weakness and increased sweating — in 69,5%. In addition, 38,9% of patients noted a noticeable, newly reported, hair loss. Attention is drawn to the high prevalence of neurological symptoms during hospiatalization, including dizziness, severe headaches not relieved by analgesics and non-steroidal anti-inflammatory drugs, lethargy, disorientation of place and time, and in some cases even hallucinations. Some of the symptoms persist after 1 month: 55,5% note a decrease in memory, 36% — feelings of fear and anxiety, 63,9% — sleep disorders in the form of frequent nocturnal awakenings (19,4%), insomnia (16,6%), long falling asleep (11,1%). Some of the respondents revealed unfavorable events over the past month as follows: blood pressure (BP) destabilization in the form of episodes of BP increase and decrease during the day — 36,0%, hypertensive crisis — 14,0%. There was an increase in the number of patients with subclinical and clinical depression (p<0,05). There was also an increase in the number of patients with hypercholesterolemia compared with inhospital data by 15,5%.
Conclusion. One month after discharge, the respiratory symptoms naturally decrease, but new symptoms appear, such as shortness of breath during exercise, fatigue, unsteady gait, hair loss, and increased sweating. There was an increase in the number of patients with subclinical and clinical depression on the HADS scale. Among laboratory parameters, an increase in the number of patients with increased level of total cholesterol and low-density lipoproteins was revealed.
Aim. To assess the diagnostic value of heart rate variability (HRV) parameters and regulatory-adaptive status index and their prognostic value after orthotopic heart transplantation.
Material and methods. The study included 70 patients after orthotopic heart transplantation using a modified bicaval technique performed in the period from 2012 to 2015. The follow-up period was 36±1 month. Most of the recipients were men — 59 (84,29%). The mean age was 50,24±10 years. Twelve, 24 and 36 months after the operation, recipients underwent right ventricular endomyocardial biopsy, 24-hou relectrocardiographic monitoring, and a cardiorespiratory synchronization (CRS) test. Statistical data processing was carried out using the Statistica 10 software (StatSoft Inc., version 10.0.228.8, Oklahoma, USA). The informativeness of studied parameters in predicting rejection episode was assessed by ROC analysis.
Results. Twelve months after transplantation, rejection episode was diagnosed in 23 (33%) recipients, 24 months — in 23 (34,8%), 36 months — in 19 (29,6%). CRS characteristics did not differ significantly depending on the presence of a rejection episode as 12 months after surgery (p>0,2) and subsequently (p>0,3). HRV values in the first year after surgery did not show differences in the groups with a rejection episode. After 2 years, the high-frequency component of the HRV frequency domain had the highest predictive value (AUC=0,693, p=0,005). Three years after the operation, all analyzed HRV parameters demonstrated informative value for the diagnosis of rejection episode, the highest predictive value among which had the heart rate (AUC=0,873, p<0,001).
Conclusion. The study of HRV should be considered to assess the risk of a rejection episodes in recipients 2 and 3 years after surgery. The regulatory-adaptive status index, being an integral value of cardiac transplant reinnervation, does not demonstrate predictive value in relation to the rejection episode within 3 years after transplantation. However, it confirms the fact of cardiac transplant reinnervation and allows assessing the regulatory-adaptive status of recipients after surgery.
CLINICAL CASE
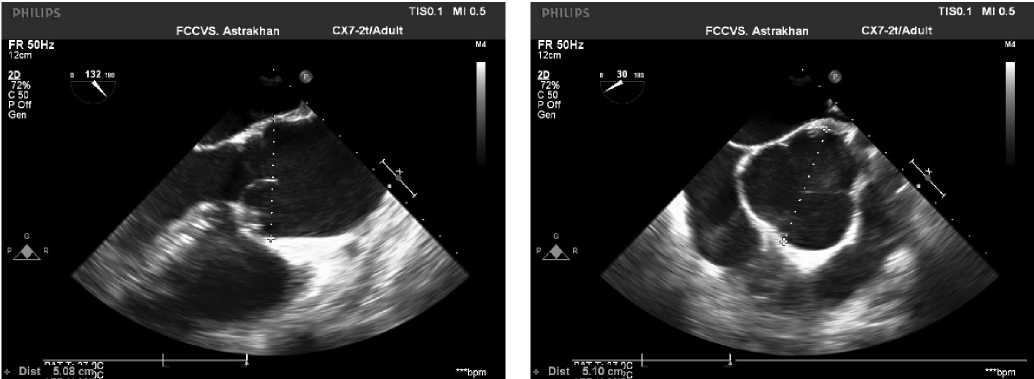
Pulmonary autograft in the aortic position provides high survival rate and quality of life for patients, low incidence of valve-related complications, and excellent hemodynamic characteristics both in the early and long-term period. However, in some patients in the long-term period, pulmonary autograft may dilate, which in turn is one of the reasons for reoperations. In patients who require surgery for annuloaortic ectasia with aortic valve (AV) regurgitation or aortic root aneurysm (or both) with normal AV leaflets, David procedure is considered.
Aim. To analyze results of David procedure after a prior Ross operation.
Material and methods. From April 2009 to December 2020, 212 Ross operations were performed on patients 18 years of age and older. The median age of the operated patients was 34 (27-45) years. In the long-term period, 10 (4,7%) patients required a second AV operation and 7 (3,3%) of them required another intervention on the ascending aorta due to aortic dilatation. Four out of 10 patients underwent David procedure. The follow-up period for patients after David procedure ranged from 2 to 84 months.
Results. The age of patients ranged from 23 to 45 years. Three patients had hypertension. The follow-up period from Ross's operation to David's one was 26 to 140 months. All patients had enlarged aortic annulus from 27 to 30 mm. The duration of myocardial ischemia ranged from 87 to 142 minutes, while the duration of artificial circulation — from 119 to 165 minutes. The graft diameter was 30 mm in two patients and 32 mm in the remaining ones. The length of stay in intensive care unit ranged from 16 to 23 hours. In the early postoperative period, no one had following postoperative complications: acute renal failure requiring hemodialysis, perioperative myocardial injury, stroke, sternal infection, respiratory failure requiring mechanical ventilation for ≥24 hours, resternotomy for bleeding and tamponade. In addition, there were no in hospital deaths. All patients had no aortic regurgitation at the time of discharge. All patients are alive and there were no reoperations. In one patient, in the long-term period, there was a mild aortic regurgitation, while in three patients — there is no regurgitation.
Conclusion. The presented case series show that David procedure can be performed safely and effectively in a significant number of patients requiring a second autograft surgery due to neosinus dilatation. In the medium term, the David procedure has shown good outcomes in these patients with 100% survival and no aortic regurgitation and reoperation.
EXPERT CONSENSUS
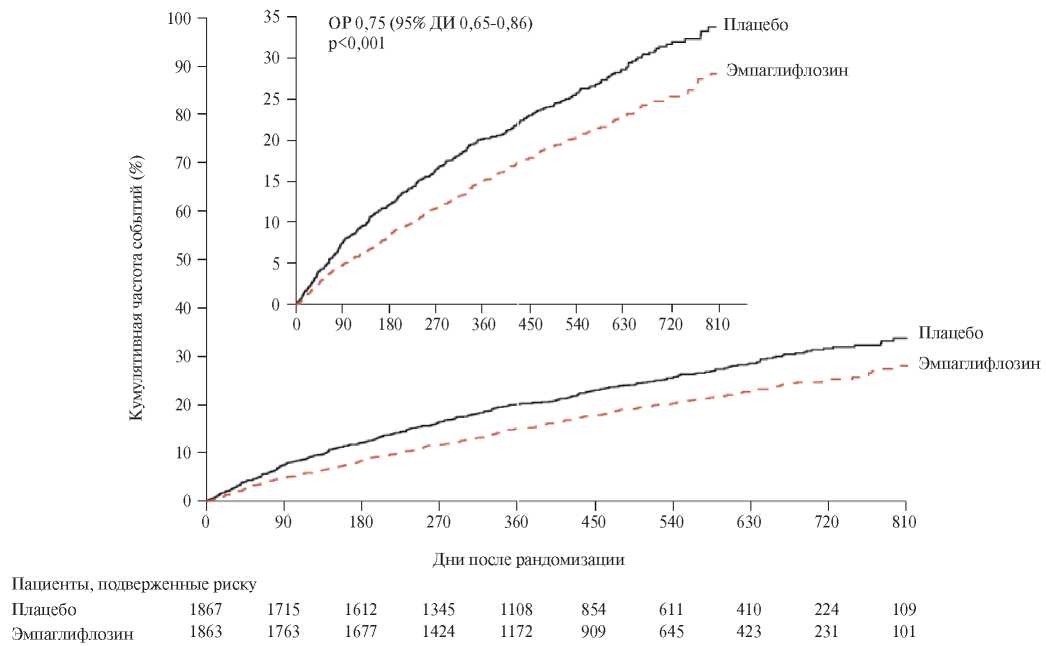
At an online meeting of experts held on May 14, 2021 additional research results on a sodium-glucose co-transporter-2 (SGLT2) inhibitor empagliflozin in patients with heart failure with reduced ejection fraction were considered. According to the data from the EMPEROR-Reduced international study, cardiovascular and renal effects of empagliflozin therapy in patients with and without type 2 diabetes (T2D) were analyzed. A number of proposals and recommendations was accepted regarding the further study of cardiovascular and renal effects of empagliflozin and its use in clinical practice in patients with heart failure, regardless of the T2D presence.
REVIEW
In the EMPA-REG OUTCOME, CANVAS and DECLARE-TIMI 58 studies, in patients with type 2 diabetes and established cardiovascular diseases or risk factors, a decrease in the risk of cardiovascular events and development or worsening of heart failure course without an increase in hypoglycemia incidence was revealed in those receiving sodium-glucose co-transporter-2 (SGLT2) inhibitors compared with placebo. To date, various mechanisms of action of SGLT2 inhibitors have been described, which are considered from the standpoint of their influence on the course and prognosis of heart failure. In the EMPEROR-Reduced study in the group of patients receiving empagliflozin, a significant reduction in the risk of cardiovascular death and hospitalizations for heart failure, regardless of the type 2 diabetes presence, was revealed.
Patients with atrial fibrillation (AF) often have comorbidities or characteristics (senile age, chronic kidney disease, high risk of coronary events, cognitive impairment) that can affect the patient's prognosis and that must be taken into account when prescribing therapy for stroke prevention. However, there are groups of patients with a high risk of bleeding, which cause concern to the doctor about possible hemorrhagic events. Direct Oral Anticoagulant (DOAC) Xarelto® (rivaroxaban) compared with other DOACs confirmed a favorable safety profile in the widest patient population: from children to senile patients. Moreover, high safety indicators in the treatment with rivaroxaban were obtained in vulnerable, from the point of view of hemorrhagic risks, patients with AF with various risk factors: those with a high risk of bleeding according to HAS-BLED scores, elderly patients, patients with chronic kidney disease, including advanced stages, as well as with anemia. It is important to remember that bleeding is not the only undesirable outcome for an elderly patient with AF. To ensure the most favorable prognosis of his life and health, it is necessary to level the maximum possible number of risks. The use of rivaroxaban may make it possible to approach the therapy of an elderly patient with AF in a comprehensive manner: to prevent stroke with a proven safety profile, while simultaneously reducing the risks of coronary events and renal complications, as well as contributing to the formation of high adherence — a necessary condition for obtaining the expected results of therapy.
The coronavirus disease 2019 (COVID-19) pandemic is associated with high virulence, mortality and healthcare burden around the world. One of its features is procoagulant activity, which leads to a high incidence of thromboembolic events in the lungs and other organs. Therefore, from the very onset of the moderate COVID-19, low molecular weight heparins began to be used as anticoagulants, which proved to have a beneficial effect on mortality and the disease course and were included in all guidelines. However, the question on anticoagulant therapy need after discharge from the hospital is controversial. The opinions of various medical professional communities on this issue are divided. In particular, some of them, including the Russian Ministry of Health guidelines recommend 30-45day anticoagulation using novel oral anticoagulants (dabigatran, rivaroxaban, apixaban), but other sources do not provide such recommendations. This review discusses the effectiveness of anticoagulant therapy after COVID-19, as well as the need to use stratification scales to assess this therapy.
Physical activity is a generally accepted means of primary and secondary prevention of cardiovascular diseases, but in some cases, it can be a risk factor for cardiovascular events, including sudden cardiac death (SCD). Most studies analyze the relationship of cardiovascular events with the volume and general directions of exercise. Besides, a significant part of the guidelines and studies are devoted to the effects of aerobic exercise, while the importance of anaerobic exercise remains controversial. The review analyzes works devoted to the influence of strength training, such as weightlifting, bodybuilding, powerlifting, etc., on the cardiovascular system, as well as their relationship with SCD and other cardiovascular events. The design and contingent of the analyzed papers did not allow them to be systematized correctly. Therefore, the review is largely analytical in nature.
The article is devoted to the modern understanding of endothelial dysfunction development, the role of hyperhomocysteinemia, and, as a consequence, hypertension in patients with multiple myeloma receiving multiagent chemotherapy. Considering that the potential of a standard examination does not allow identifying subclinical endothelial dysfunction, using specific techniques is necessary, in particular, to determine the homocysteine level to monitor the endothelial function.
The aim of this review was to summarize the current understanding of hypertension etiology and prospects for detecting early, subclinical endothelial changes, including in patients with multiple myeloma.
Assessment of endothelial dysfunction can be useful for detecting precisely the subclinical cardiovascular disease in order to stratify the risk of developing cardiovascular events in patients receiving multiagent chemotherapy.
The second part of the review highlights treatments for different types of sleep apnea in patients with heart failure. In both obstructive and central sleep apnea, ventilatory support during sleep takes a special place in treatment. Therefore, the review details the role of different ventilation modes (in particular, CPAP therapy and adaptive servo-ventilation), analyzes available evidence-based medicine data. The role of low-flow oxygen therapy, surgical treatment, implantable devices, specific therapy (theophylline, acetazolamide) in the treatment of central sleep apnea is also shown, and a novel method of treating central sleep apnea is considered — phrenic nerve stimulation.
INFORMATION
ISSN 2618-7620 (Online)