ORIGINAL ARTICLES
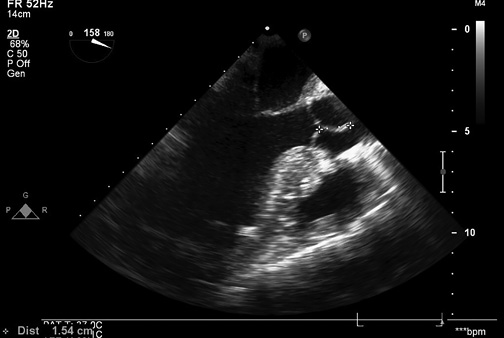
The Ozaki procedure is a promising procedure, which does not require consumables in the form of an artificial valve with a frame, preserves the natural participation of annulus in the cardiac cycle, thereby leading to excellent hemodynamic parameters, such as the valve pressure gradient and effective orifice area.
Aim. To evaluate the aortic valve (AV) hemodynamic characteristics after the Ozaki procedure according to echocardiography.
Material and methods. The retrospective multicenter study included 277 patients with AV defects who were operated on from January 2017 to June 2022 in five centers in Russia. After the Ozaki procedure, the following endpoints were assessed: immediate echocardiographic results (peak AV gradient, mean AV gradient, AV effective orifice area, aortic regurgitation grade), mid-term clinical (three-year survival rate, three-year freedom from reoperation, three-year freedom from grade ≤2 aortic regurgitation) and echocardiographic results (peak and mean AV gradient, AV effective orifice area, aortic regurgitation grade, AV calcification severity). The median follow-up period was 23 (13-32) months. The mean echocardiography follow-up period was 21±10 months.
Results. During the treatment, a decrease in the peak AV gradient was observed from 74±30 mm Hg before surgery up to 12 (8-16) mm Hg one week after surgery, which remained in the mid-term period — 12 (9-15) mm Hg. There was also a decrease in the mean gradient from 40 (27-53) mm Hg before surgery up to 6 (4-8) mm Hg one week after surgery. By the mid-term period, the mean gradient was 6 (4-8) mm Hg. The AV effective orifice area increased from 1 (1-1) cm2 to 2 (2-2) cm2 in the mid-term follow-up period. Three-year survival rate was 90,2%, freedom from reoperation was 95%, freedom from grade ³2 aortic regurgitation was 88%, and no patient had AV calcification.
Conclusion. The Ozaki procedure in patients with AV defects has good immediate and mid-term hemodynamic parameters according to echocardiography. However, there remains a need for large randomized controlled trials comparing Ozaki procedure with biological AV replacement.
- Acute chest pain is a leading cause of emergency department visits.
- Optimal diagnostic tactics for acute chest pain remains one of the most challenging problems in the emergency department.
- First-line coronary computed tomography angiography approach in patients with low-to-intermediate-risk NSTE-ACS is not inferior to the standard of care for managing these patients, while significantly reducing the need for the invasive coronary angiography.
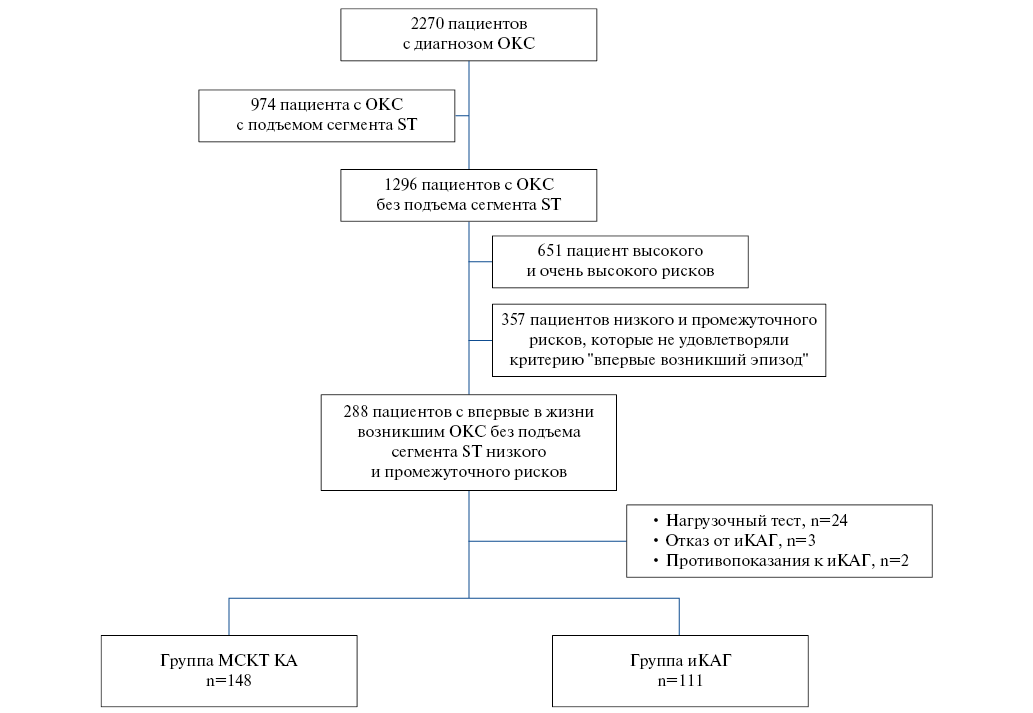
Aim. To evaluate the strategy of using coronary computed tomography angiography (CCTA) in patients with low-to-intermediate risk of non-ST segment elevation acute coronary syndrome (NSTE-ACS) in relation to early (in-hospital) and long-term prognosis in comparison with standard management tactics.
Material and methods. The study included 259 patients (men (M), 47,9%, mean age, 62,2±9,4 years). Patients in group 1 (n=148 people, M 46,6%, mean age 61,99±9,92 years) underwent CCTA to assess coronary involvement, and patients in group 2 (n=111 people, M 49,5%, mean age 62,4±8,6 years) — invasive coronary angiography (ICA). The follow-up lasted 18 months.
Results. Patients in both groups were comparable in age, concomitant chronic diseases and smoking. Patients in the CCTA group compared with the ICA group had lower GRACE score and lower values of high-sensitivity Troponin I. In 85 patients (57,4%) of group 1 there was no coronary involvement, while 41 patients (27,7%) had <50% stenosis, 22 patients (14,9%) — >50% stenosis in at least one coronary artery. In group 2, the majority of patients also had non-involved coronary vessels (n=76; 68,5%), while hemodynamically insignificant (20-40%) and significant lesions were detected in 20 patients (12,3%) and 15 people (13,5%), respectively. In group 1, 20 patients were referred for ICA as follows: 10 patients underwent percutaneous coronary interventions; 2 patients had multivessel disease; in 4 patients, intraoperative fractional flow reserve revealed hemodynamically insignificant stenoses; in 4 remaining patients, no significant lesions were detected. All-cause mortality was 4,05% in the CCTA group, and 7,2% in the ICA group (p=0,28). In the CCTA group, cardiovascular mortality was 0%, and in the ICA group — 0,9% (p=0,43).
Conclusion. CCTA in patients with low-to-intermediate risk ACS is not inferior to the standard tactics for managing these patients and significantly reduces the need for iCAG.
- The serum biomarker profile of patients with psoriasis/coronary artery disease/coronary artery disease+psoriasis was significantly different from each other.
- Risk factors for cardiovascular hospitalization were psoriasis and an increase in the serum level of N-terminal pro-brain natriuretic peptide.
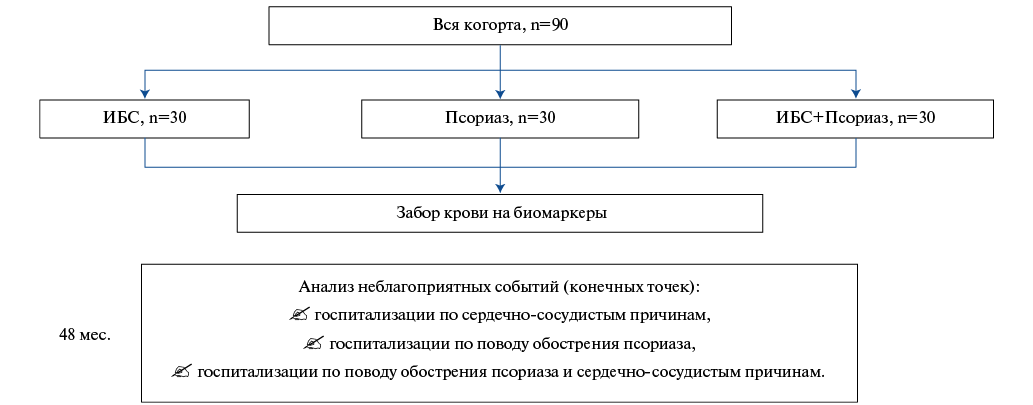
Aim. To study serum biomarker profile in patients with coronary artery disease (CAD) and psoriasis and the impact on the incidence of hospitalization for cardiovascular reasons and psoriasis.
Material and methods. The study included 90 patients divided into following 3 groups: with psoriasis (n=30), coronary artery disease (CAD) (n=30) and CAD+psoriasis (n=30) in whom serum biomarkers were determined at the beginning of the study (growth stimulation expressed gene 2, N-terminal pro-brain natriuretic peptide (NT-proBNP), interleukin-17 and tumor necrosis factor alpha) and hospitalization rates were monitored over 4 years.
Results. There was a significant difference in the concentrations of all biomarkers between the groups (p<0,05), with the maximum values being in the CAD+psoriasis group, except for NT-proBNP. In regression analysis, risk factors for cardiovascular hospitalizations were psoriasis (p=0,049) and increased NT-proBNP concentrations (p<0,001).
Conclusion. Comorbidity leads to an increase in the serum concentration of biomarkers, while the risk factors for cardiovascular hospitalization were psoriasis and serum NT-proBNP level.
- Short-term adherence to cardiovascular and coronavirus disease 2019 (COVID-19) therapy is comparable.
- A patient's self-assessment during the COVID-19 affects compliance with medical recommendations.
- Adverse cardiovascular events increase compliance up to 6 months after recovery from COVID-19.
Aim. To evaluate the relationship of various factors with adherence to therapy in cardiovascular patients after a coronavirus disease 2019 (COVID-19).
Material and methods. The study included 284 patients (inpatients — 176, outpatients — 108) with cardiovascular diseases (hypertension, heart failure (HF), coronary artery disease, atrial fibrillation) after COVID-19. We collected data on cardiovascular history, made a questionnaire survey about COVID-19 course (symptoms, their severity, self-assessment of the disease severity). Paraclinical diagnostic investigations were carried out. In addition, 1, 3, 6 months after recovery, all respondents were invited for examination, laboratory tests, and survey using the Hospital Anxiety and Depression Scale (HADS). Cardiovascular therapy adherence was assessed at 1, 3 and 6 months after recovery and adherence to COVID-19 treatment 1 month after inclusion in the study by comparing the compliance of the drugs prescribed at discharge with its actual use.
Results. In total, 212 respondents continued study participation after 1 month, while 64,2% were adherent to cardiovascular therapy and 56,6% — to COVID-19 therapy. Compliance at 3 and 6 months was 60,4% (n=212) and 52,8% (n=188), respectively. A moderate correlation was found between adherence to treatment and the persistence of apprehension 1 month after recovery (r=0,33, p<0,05), moderate or severe weakness during disease (r=0,31, p<0,05), COVID-19 severity (r=0,39, p<0,05). Inhospital respondents with lung tissue involvement >25% (n=64, 36,4%) were more adherent to standard cardiovascular therapy, prescribed in accordance with clinical guidelines (r=0,336, p<0,05). Adverse events in the form of a hypertensive crisis, arrhythmias, decompensated HF 1, 3, 6 months after recovery significantly increased the compliance with medical recommendations (p<0,05). Medication adherence regarding COVID-19 was associated with the disease severity, HF history, apprehension and anxiety, weakness, and decreased exercise tolerance (p<0,05).
Conclusion. After 1 month, adherence to cardiovascular and COVID-19 therapy did not differ significantly (p>0,05). Compliance after 1, 3, 6 months was positively influenced by COVID-19 severity, the subjective feeling of weakness, apprehension and anxiety during disease and the persistence of a subjective feeling of anxiety after recovery. Adverse events (hypertensive crisis, arrhythmia, decompensated HF) during 1, 3 and 6 months after COVID-19 significantly (p<0,05) increased adherence to treatment.
- When planning training, the doctor's specialty and work experience should be taken into account.
- Unjustifiably high self-rating of knowledge interferes with professional development.
- Direct study of the text of clinical guidelines is the best way for doctors to educate themselves.
Aim. To find out the relationship between the awareness level of clinical guidelines on heart failure (HF) with reduced ejection fraction and a number of professional characteristics (specialty, work experience, self-assessment of awareness level, attitude towards the use of guidelines, the main way of document study). To improve the efficiency and development of the postgraduate education system, the factors that influence doctors' awareness of guidelines should be determined.
Material and methods. The study included the results of an anonymous survey of 207 doctors (155 cardiologists, 44 therapists, 8 doctors of other specialties). To assess the significance of differences, Student's t-test, c2-test and Fisher's exact test were used.
Results. The mean number of correct answers to the questionnaire among cardiologists was significantly higher than among general practitioners (p<0,001). In the group of physicians with less than 5 years of work experience, there was a large variability in the mean number of correct answers — 6,2±4,0. Physicians with 6-10 years and 11-20 years of experience in their specialty were more likely to choose the correct answers than doctors with more than 20 years of experience. Professionals who considered themselves "fully informed" on clinical guidelines gave fewer correct answers than doctors who had less high self-rating (p<0,001). The proportion of correct answers in the subgroup of doctors who consider guidelines to be mandatory was greater than in the subgroups of doctors who hold a different opinion (p<0,05). The best results were shown by physicians who indicated direct text-oriented way as preferred for studying guidelines (p<0,001).
Conclusion. The awareness level of clinical guidelines on the treatment of HF by cardiologists should be considered insufficient, and by therapists — extremely low. Doctors are not sufficiently informed about the need to comply with clinical guidelines. When planning training, the specialty and work experience of the doctor should be taken into account. Unjustifiably high self-rating of knowledge interferes with professional development. The best way of self-education should be considered direct study of the text of clinical guidelines.
- In patients with heart failure with mildly reduced ejection fraction (HFmrHF), parameters of atrial electrical remodeling, as well as body mass index, play an important role in the occurrence of paroxysmal/persistent atrial fibrillation (AF).
- Deterioration of left ventricular diastolic function and changes in left atrium geometry are possible risk factors for paroxysmal/persistent AF in patients with HFmrHF.
- An increase in the concentration of inflammatory markers contributes to paroxysmal/persistent AF in patients with HFmrHF, and an increase in the level of a profibrotic marker contributes to persistent AF in these patients.
Aim. To study possible risk factors (RFs) for the development of paroxysmal and persistent atrial fibrillation (AF) in patients with heart failure with mildly reduced ejection fraction (HFmrHF).
Material and methods. The study included 193 patients with chronic HFmrHF and non-valvular paroxysmal/persistent AF. Seventy-six comparable patients, but without AF, were studied as a control group. All patients underwent a detailed physical examination, including electrocardiography (ECG), echocardiography, ambulatory blood pressure monitoring, and Holter ECG monitoring. Levels of inflammatory markers, namely high-sensitivity C-reactive protein, interleukin-6, tumor necrosis factor-a and fibrotic marker, transforming growth factor-b1 (TGF-b1) were measured using ELISA. The results obtained were analyzed using the method of binary logistic regression and odds ratio (OR), which allows us to assess the relationship of a specific outcome with possible risk factors and compare study groups according to the detection rate of risk factors.
Results. A higher level of diastolic blood pressure (DBP) (OR=1,09, confidence interval (CI)=1,01-1,17, p=0,017) is a possible risk factor for paroxysmal AF in patients with CHF. Possible risk factors for paroxysmal and persistent AF in such patients are an increase in episodes of hypertensive crisis (OR=1,17, CI=1,071,43, p=0,001) and an increase in body mass index (BMI) (OR=1,13, CI=0,931,27, p=0,031). An increase in the OR index of left ventricular diastolic and systolic parameters was associated with significant atrial and ventricular remodeling, which contributes to AF progression from paroxysmal to persistent. Higher levels of inflammatory markers were observed in patients with AF compared with patients with HFmrHF without AF. The increase in the OR level of TGF-b1 (OR=3,84, CI=2,106,23, p=0,005) was significant in patients with persistent AF.
Conclusion. Using the OR method, an increase in DBP, the prevalence of hypertensive crisis, BMI, left atrial and ventricular remodeling, an increase in markers of systemic inflammation and fibrosis are possible risk factors for AF in patients with HFmrHF.
МЕТОДЫ ОБУЧЕНИЯ ПАЦИЕНТОВ
- People with disabilities make up approximately 15% of the world's population and need to learn the principles and rules of first aid for cardiac arrest.
- All free online CPR courses analyzed were found to have digital content accessibility issues.
- Students with visual, cognitive and motor impairments are most vulnerable to accessibility restrictions, including older people, who are likely to witness cardiac arrest at home and therefore constitute a priority category for resuscitation training.
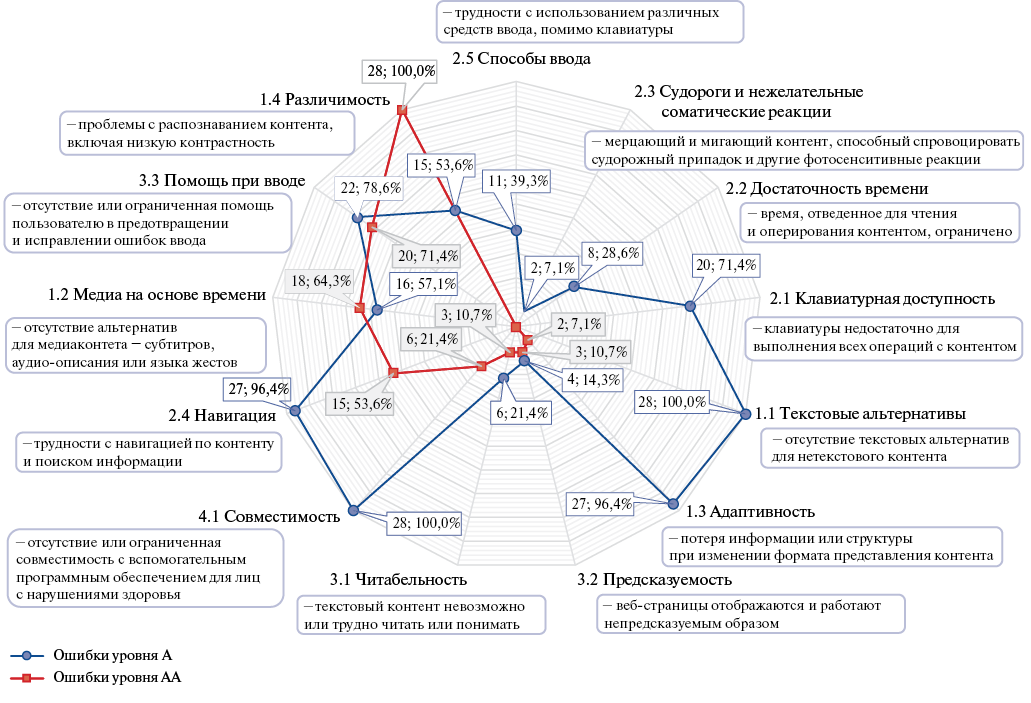
Aim. Basic first aid digital training for cardiac arrest opens up opportunities for mass dissemination of knowledge, popularization and motivation of the population to provide assistance, and can also replace the theoretical part of classroom training, reducing the cost of training. However, due to poor design, such training may not be available to people with disabilities (PWD), who constitute a large population of more than one billion potential participants in first aid. The aim was to study the digital accessibility (web accessibility) of massive open online courses in cardiopulmonary resuscitation (CPR) for PWD.
Material and methods. A search was carried out for free English-language online courses teaching the principles and rules of providing first aid in cardiac arrest. In addition, the digital content of online courses was assessed for compliance with the international Web Content Accessibility Guidelines (WCAG) 2.1.
Results. All basic CPR online courses analyzed (n=28) were characterized by poor web accessibility. For each course, between 26,9% and 51,3% of the WCAG 2.1 guideline success criteria were not met. All courses have web accessibility errors related to text contrast and visual issues, lack of alternative text descriptions for non-text content, missing abbreviations, and web page layout issues that prevent the use of assistive technologies (such as text-to-speech software). Overall, none of the courses meet all of the criteria for the minimum acceptable level of compliance with WCAG 2.1 guidelines. The discovered problems of web accessibility can serve as serious, sometimes insurmountable barriers to the mastery of courses by students (including older people) with visual impairments, hearing loss, motor, cognitive and neurological disorders.
Conclusion. All free mass online courses on basic CPR have deficiencies in the availability of digital content, which significantly complicate the learning of educational materials by PWD. The development of uniform guidelines for accessible educational content, along with the intensification of research and the implementation of organizational and methodological measures to ensure the availability of educational resources on first aid for various categories of the population, should help create equal opportunities for quality training. In addition, this should significantly expand the population coverage with training, and increase the frequency and effectiveness of first aid.
CLINICAL CASE
The young age of patients does not rule out the risk of acute coronary syndrome, even in the absence of widely known risk factors, including genetic.
Myocardial infarction usually occurs in people over 50 years of age, but younger patients can also be affected. The article presents a case of a young patient, 34 years old, who was admitted to the cardiology department with a diagnosis of lowrisk non-ST segment elevation acute coronary syndrome. The patient complained of anginal pain that occurred for the first time. However, she did not have typical risk factors for cardiovascular diseases. Coronary angiography showed a critical stenosis of 99% in the proximal third of the 2nd segment of the right coronary artery. A case clearly demonstrates the importance of a thorough examination of young patients with complaints of chest pain, which is often mistakenly interpreted as a pathology of other organs and systems other than the cardiovascular one. No risk factors in a patient does not guarantee low risk of myocardial infarction, and a detailed examination of the patient will help to avoid underdiagnosis of acute coronary syndrome.
SUPPORTING A PRACTITIONER
REVIEW
- The increasing prevalence of HIV infection causes an inevitable increase in the proportion of HIV-infected patients among patients with acute coronary syndrome (ACS).
- Increased survival of HIV-infected patients increases the importance of traditional risk factors for myocardial infarction (MI).
- The current Russian and European clinical guidelines for ACS/MI lack evidence-based data on the management of HIV-infected patients.
- The review provides new data on the features of the pathogenesis, course and treatment of MI in this population, which will be of practical importance for cardiologists.
HIV infection increases the risk of premature myocardial infarction (MI) and other atherosclerotic cardiovascular diseases, which are the main noncommunicable cause of death in HIV-infected patients. The review presents the analysis of recent literature on the incidence, prevalence and risk factors of MI in HIV-infected people. It established that MI is associated with the combined effects of traditional cardiovascular risk factors, HIV infection and the cardiometabolic effects of antiretroviral therapy. Pathogenetic features of acute coronary syndrome in HIV infection under conditions of systemic immune-mediated inflammation, hypercoagulation and direct exposure to the virus are highlighted. The clinical features and coronary damage in MI are described. Methods of treating MI are compared. We concluded that the volume and quality of care for patients with HIV and MI is insufficient. From the perspective of possible drug interactions with antiretroviral therapy, effectiveness and safety of methods for secondary prevention of MI was analyzed.
The work covers the management of patients after heart valves surgery and answers current issues in practical cardiology: therapy of patients after mechanical and biological valve replacement; the use of antiplatelet agents in patients without prior atrial fibrillation after transcatheter aortic valve implantation; determining the duration vitamin K antagonist therapy after mitral or tricuspid valve surgery; choosing management strategy in patients with thrombotic complications on prosthetic heart valves.
After heart valve surgery, anticoagulant therapy is usually recommended. The duration and necessity of combining oral anticoagulants with antiplatelet drugs depends on the type of manipulation performed, patient comorbidity and some other factors. Several randomized trials have shown that continued direct oral anticoagulation as monotherapy in some groups of patients requiring cardiac surgery is superior in efficacy and safety to treatment combining anticoagulant and antiplatelet drugs. The presented literature review reflects the management strategy of patients after heart valve operations.
- Efficacy and safety of oral anticoagulants and vitamin K antagonists are comparable.
- The administration of direct oral anticoagulants to patients with stage 4 and 5 chronic kidney disease, including those receiving hemodialysis, was accompanied by a significant reduction in the number of major bleedings, compared with warfarin therapy.
Aim. To compare the effectiveness and safety of direct oral anticoagulants (DOACs) with a vitamin K antagonist (VKA) in patients with atrial fibrillation (AF) and stage 4 and 5 chronic kidney disease (CKD).
Material and methods. We searched in the PubMed, Google Scholar, and Web of Science databases from 1990 to 2022 for studies that compared DOACs with VKAs in patients with AF and stage 4 and 5 CKD. The patient, intervention, comparison, outcome (PICO) search strategy was used. Data were extracted by independent researchers and meta-analyzed.
Results. A total of 6 studies were included in this meta-analysis. In terms of effectiveness, DOACs were comparable to VKAs. In terms of safety, DOACs and VKAs also had no statistical differences in hemorrhagic stroke, minor/gastrointestinal bleeding, overall mortality, but there was statistical significance in major bleeding.
Conclusion. In terms of efficacy and safety, in general, DOACs were comparable to VKAs, but there were a number of following differences: the administration of DOACs to patients with stage 4 and 5 CKD, as well as those on hemodialysis, was accompanied by a significant reduction in the number of major bleedings, compared with warfarin therapy.
AD MEMORIAM
ISSN 2618-7620 (Online)