Перейти к:
Гипертрофическая кардиомиопатия. Клинические рекомендации 2025
https://doi.org/10.15829/1560-4071-2025-6387
EDN: BUUCJT
Аннотация
Российское кардиологическое общество
При участии: Ассоциации сердечно-сосудистых хирургов России, Российского общества медицинских генетиков Одобрено Научно-практическим Советом Минздрава Российской Федерации
Ключевые слова
Для цитирования:
Бокерия Л.А., Шляхто Е.В., Габрусенко С.А., Гудкова А.Я., Козиолова Н.А., Александрова С.А., Алехин М.Н., Афанасьев А.В., Богатырева М.М., Богачев-Прокофьев А.В., Богданов Д.В., Берсенева М.И., Гордеев М.Л., Дземeшкевич С.Л., Евтушенко А.В., Заклязьминская Е.В., Зенченко Д.И., Иртюга О.Б., Каплунова В.Ю., Каштанов М.Г., Костарева А.А., Крутиков А.Н., Маленков Д.А., Новикова Т.Н., Рудь С.Д., Рыбка М.М., Саидова М.А., Стрельцова А.А., Стукалова О.В., Чмелевский М.П., Шапошник И.И., Шлойдо Е.А. Гипертрофическая кардиомиопатия. Клинические рекомендации 2025. Российский кардиологический журнал. 2025;30(5):6387. https://doi.org/10.15829/1560-4071-2025-6387. EDN: BUUCJT
For citation:
Bokeria l.A., Shlyakhto E.V., Gabrusenko S.A., Gudkova A.Ya., Koziolova N.A., Alexandrova S.A., Alekhin M.N., Afanasyev A.V., Bogatyreva M.M., Bogachev-Prokofiev A.V., Bogdanov D.V., Berseneva M.I., Gordeev M.L., Dzemeshkevich S.L., Yevtushenko A.V., Zaklyazminskaya E.V., Zenchenko D.I., Irtyuga O.B., Kaplunova V.Yu., Kashtanov M.G., Kostareva A.A., Krutikov A.N., Malenkov D.A., Novikova T.N., Rud S.D., Rybka M.M., Saidova M.A., Streltsova A.A., Stukalova O.V., Chmelevsky M.P., Shaposhnik I.I., Shloido E.A. 2025 Clinical practice guidelines for Hypertrophic cardiomyopathy. Russian Journal of Cardiology. 2025;30(5):6387. (In Russ.) https://doi.org/10.15829/1560-4071-2025-6387. EDN: BUUCJT
Список сокращений
- АГ — артериальная гипертензия
- АД — артериальное давление
- АК — аортальный клапан
- АРА — антагонисты рецепторов к ангиотензину II
- АС — аортальный стеноз
- ВОЗ — Всемирная организация здравоохранения
- ВСС — внезапная сердечная смерть
- ВТЛЖ — выходной тракт левого желудочка
- ВТПЖ — выходной тракт правого желудочка
- ГКМП — гипертрофическая кардиомиопатия
- ГЛЖ — гипертрофия левого желудочка
- ГД — градиент давления
- дГКМП — дилатационная стадия гипертрофической кардиомиопатии
- ДНК — дезоксирибонуклеиновая кислота
- ЕОК, ESC — Европейское общество кардиологов
- ЖНР — желудочковые нарушения ритма
- ЖТ — желудочковая тахикардия
- иАПФ — ингибиторы ангиотензинпревращающего фермента
- ИБС — ишемическая болезнь сердца
- ИК — искусственное кровообращение
- ИКД — имплантируемый кардиовертер-дефибриллятор (кардиовертер-дефибриллятор имплантируемый однокамерный***; кардиовертер-дефибриллятор имплантируемый двухкамерный***; кардиовертер-дефибриллятор имплантируемый трехкамерный (бивентрикулярный)***)
- ИМ — инфаркт миокарда
- КАГ — коронароангиография
- КДО — конечно-диастолический объем
- КТ — компьютерная томография
- ЛА — легочная артерия
- ЛГ — легочная гипертензия
- ЛЖ — левый желудочек
- ЛП — левое предсердие
- МЖП — межжелудочковая перегородка
- МК — митральный клапан
- МНО — международное нормализованное отношение
- МСКТ — мультиспиральная компьютерная томография
- МР — митральная регургитация
- МРТ — магнитно-резонансная томография
- ОГКМП — обструктивная гипертрофическая кардиомиопатия
- ОКС — острый коронарный синдром
- ПЖ — правый желудочек
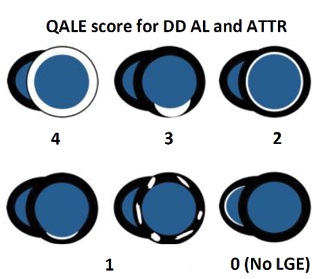
- ПНГ — позднее накопление гадолиний-содержащего контрастного вещества
- ПОАК — прямые оральные антикоагулянты (ингибиторы тромбина прямые: дабигатрана этексилат** или прямые ингибиторы фактора Xa: апиксабан**, ривароксабан**, эдоксабан)
- ПСД — переднее систолическое движение
- ПЭТ — позитронно-эмиссионная томография
- рГКМП — рестриктивный фенотип гипертрофической кардиомиопатии
- РКО — Российское кардиологическое общество
- РОМГ — Российское общество медицинских генетиков
- СМЭ — септальная миоэктомия (А16.10.003.23 Миэктомия по Морроу (Morrow) в условиях искусственного кровообращения)
- ТП — трепетание предсердий
- ТТР — транстиреиновый
- ТТ-ЭхоКГ — трансторакальная эхокардиография
- УДД — уровни достоверности доказательств
- УО — ударный объем
- УУР — уровни убедительности рекомендаций
- ФВ — фракция выброса
- ФЖ — фибрилляция желудочков
- ФК — функциональный класс
- ФН — физическая нагрузка
- ФП — фибрилляция предсердий
- ХМ — холтеровское мониторирование
- ХСН — хроническая сердечная недостаточность
- ЧП-ЭхоКГ — чреспищеводная эхокардиография
- ЧСС — частота сердечных сокращений
- ЭКГ — электрокардиография
- ЭКС — электрокардиостимулятор, электрокардиостимуляция
- ЭСА — этаноловая септальная аблация (06.ЕБГ.13.001.006 Спиртовая септальная аблация эндоваскулярным доступом)
- ЭхоКГ — эхокардиография
- ACC — American College of Cardiology (Американская коллегия кардиологов)
- ACMG — The American College of Medical Genetics and Genomics (Американская коллегия медицинской генетики)
- AHA — American Heart Association (Американская ассоциация сердца)
- ATTR — транстиретиновый амилоидоз
- EACVI — European Association of Cardiovascular Imaging (Европейская ассоциация по сердечно-сосудистой визуализации)
- HCM Risk-SCD — шкала риска ВСС при ГКМП
- INOCA — ischemia with non-obstructive coronary arteries (ишемия без обструкции коронарных артерий)
- MINOCA — myocardial infarction with non-obstructive coronary arteries (инфаркт миокарда без обструкции коронарных артерий)
- MOGE’S — классификация кардиомиопатий
- NT-proBNP — N-концевой промозговой натрийуретический пептид
- NYHA — Нью-Йоркская ассоциация сердца
- SAM-syndrome — systolic anterior motion syndrome (передне-систолическое движение створок митрального клапана)
** — препарат включен в перечень жизненно необходимых и важнейших лекарственных препаратов; *** — медицинское изделие, имплантируемое при оказании медицинской помощи в рамках программы государственных гарантий бесплатного оказания гражданам медицинской помощи.
Термины и определения
Гипертрофическая кардиомиопатия (ГКМП) — это преимущественно генетически обусловленное заболевание (семейные и несемейные формы), характеризующееся гипертрофией миокарда левого желудочка (ЛЖ) (≥1,5 см у взрослых) и/или реже правого желудочка (ПЖ), чаще асимметричного характера за счет утолщения межжелудочковой перегородки (МЖП), фиброзом и феноменом "disarray", которое не может объясняться исключительно повышением нагрузки давлением и возникающее при отсутствии других потенциально причинных системных, синдромных или метаболических заболеваний.
Обструктивная гипертрофическая кардиомиопатия (ОГКМП) — форма ГКМП, сопровождающаяся нарушением внутрисердечной гемодинамики в виде препятствия систолическому изгнанию из ЛЖ и/или ПЖ, что приводит к увеличению градиента давления (ГД) в выходном тракте ЛЖ и/или ПЖ (ВТЛЖ; ВТПЖ). Обструктивной формой также является ГКМП со среднежелудочковой обструкцией.
ГКМП-фенотип — гипертрофия ЛЖ (ГЛЖ) с толщиной стенки ≥1,5 см в одном или более сегментах, которая может быть обусловлена различными причинами. ГКМП-фенотип ≠ ГКМП.
Субклиническая стадия ГКМП — этап в развитии заболевания, при котором нет клинической симптоматики, характерной для ГКМП.
Догипертрофическая стадия ГКМП — этап в развитии заболевания, при котором отсутствуют признаки гипертрофии миокарда, определяемые с помощью визуализирующих методов. Догипертрофическая стадия не эквивалентна ГКМП генотип(+)/фенотип(-).
Генотип(+)/фенотип(-) — носители генетического варианта высокого класса патогенности: V (патогенный) или IV (вероятно патогенный), ассоциированного с ГКМП.
Внезапная сердечная смерть (ВСС) — ненасильственная, обусловленная заболеваниями сердца смерть, манифестирующая внезапной потерей сознания в течение первого часа с момента появления острых симптомов.
Стратификация риска ВСС — определение независимых предикторов, определяющих вероятность риска ВСС.
Передне-систолическое движение створок митрального клапана (МК) — движение створок МК в систолу к МЖП вплоть до касания (митрально-септальный контакт), участвующее в создании обструкции ВТЛЖ. Англоязычный термин — systolic anterior motion syndrome (SAM-syndrome).
Базальная обструкция (обструкция в ВТЛЖ) — препятствие на уровне ВТЛЖ систолическому изгнанию из ЛЖ.
Среднежелудочковая обструкция — препятствие систолическому кровотоку в средней части полости ЛЖ, на уровне срединных сегментов ЛЖ.
Латентная обструкция — гемодинамическая форма ОГКМП, при которой препятствие систолическому изгнанию из ЛЖ возникает только при нагрузке или провокационных пробах.
"Классический фенотип" ГКМП — морфофункциональный фенотип ГКМП, при котором сочетаются асимметричная ГЛЖ (гипертрофия МЖП), уменьшенный размер полости ЛЖ и обструкция ВТЛЖ.
Негативное ремоделирование (англ. adverse remodeling) — финальная стадия адаптивных и дезадаптивных изменений в пораженном органе. При этом к основному ГКМП-фенотипу присоединяется дополнительный фенотип — дилатационный или рестриктивный, обозначаемые как "дилатационная стадия ГКМП" (дГКМП) или "ГКМП с рестриктивным фенотипом" (рГКМП), соответственно.
Септальная миоэктомия (СМЭ) — операция резекции миокарда МЖП (А16.10.003.23 Миэктомия по Морроу (Morrow) в условиях искусственного кровообращения (ИК))
Редукция МЖП — хирургическое (А16.10.003.23 Миэктомия по Морроу (Morrow) в условиях ИК) или эндоваскулярное (этаноловая септальная аблация (ЭСА)) воздействие по уменьшению толщины МЖП.
Секвенирование нового поколения — (NGS, массовое параллельное секвенирование) технология высокоточного одновременного определения последовательности.
Феномен "disarray" — беспорядочное расположение кардиомиоцитов и мышечных волокон.
Генотип-позитивный (G+) пациент с ГКМП — это пациент, у которого в генах, ответственных за ГКМП, выявлен хотя бы один (или более) генетический вариант высоких классов патогенности: V (патогенный) или IV (вероятно патогенный), согласно критериям патогенности, разработанным Российским обществом медицинских генетиков (РОМГ) и/или Американской коллегией медицинской генетики (ACMG).
Генотип-негативный (G-) пациент с ГКМП — это пациент, у которого в генах, ответственных за ГКМП, не было выявлено ни одного генетического варианта высоких классов патогенности: V (патогенный) или IV (вероятно патогенный), согласно критериям патогенности, разработанным РОМГ и/или ACMG.
Уровень достоверности доказательств (УДД) — степень уверенности в том, что найденный эффект от применения медицинского вмешательства является истинным.
Уровень убедительности рекомендаций (УУР) — степень уверенности в достоверности эффекта вмешательства и в том, что следование рекомендациям принесет больше пользы, чем вреда в конкретной ситуации.
Фенокопия ГКМП — заболевание, фенотипически похожее на ГКМП по данным рутинных методов исследования (электрокардиографии (ЭКГ), эхокардиографии (ЭхоКГ)), но отличающееся иным этиопатогенезом и возможностью этиопатогенетической терапии для отдельных нозологий.
Рабочая группа по разработке/актуализации клинических рекомендаций — коллектив специалистов, работающих совместно и согласовано в целях разработки/актуализации клинических рекомендаций и несущих общую ответственность за результаты данной работы.
1. Краткая информация по заболеванию или состоянию (группе заболеваний или состояний)
1.1. Определение заболевания или состояния (группы заболеваний или состояний)
ГКМП — это преимущественно генетически обусловленное заболевание (семейные и несемейные формы), характеризующееся ГЛЖ (≥1,5 см у взрослых) и/или реже ПЖ, чаще асимметричного характера за счет утолщения МЖП, фиброзом и феноменом "disarray", которое не может объясняться исключительно повышением нагрузки давлением и возникающее при отсутствии других потенциально причинных системных, синдромных или метаболических заболеваний.
Комментарии. Общепринятой классификации различных этиологических форм ГКМП нет.
В рекомендациях AHA/ACC (2020) под ГКМП понимаются саркомерные ГКМП, либо генотип-отрицательные пациенты с так называемым ГКМП-фенотипом (толщина миокарда ЛЖ ≥15 мм — критерий ГКМП у пробанда), но при этом ГЛЖ не обусловлена другим сердечным, системным или метаболическим заболеванием (ГКМП-фенотип ≠ ГКМП). Соответственно, метаболические и мультиорганные синдромы (RAS-патии, митохондриальные миопатии, гликогенозы/лизосомальные болезни накопления, амилоидоз, саркоидоз, гемохроматоз) не попадают в рубрику ГКМП. Эти болезни часто называют "фенокопиями" или синдромными ГКМП [1][2].
При втором подходе, который разделяют европейские кардиологи (Европейское общество кардиологов, ЕОК) и американские педиатры (the American Heart Association Council on Cardiovascular Disease in the Young) к ГКМП относится большая группа заболеваний, при которых выявляется ГКМП-фенотип (ГЛЖ с толщиной стенки ≥15 мм у взрослых или >2 Z-оценок у детей), при этом оговаривается, что такая степень ГЛЖ не обусловлена исключительно условиями нагрузки на ЛЖ.
В рекомендациях ЕОК (2014) приведены 8 этиологических подгрупп заболевания: саркомерные ГКМП, метаболические, митохондриальные кардиомиопатии (КМП), нейромышечные болезни, синдромы мальформации и RAS-патии, инфильтративные/воспалительные болезни миокарда, эндокринные нарушения, а также ГКМП, развившаяся после применения лекарственных препаратов [3-6].
То есть все так называемые синдромные ГКМП (термин чаще используемый у пациентов детского возраста) и "фенокопии" (термин чаще используемый у взрослых пациентов) считаются как "ГКМП, имеющие специфическую причину".
Возраст манифестации клинических проявлений — важная детерминанта прогноза и этиологической принадлежности ГКМП-фенотипа. Например, ГКМП, диагностируемый в возрасте до одного года, связан с худшим прогнозом и нередко вызван наследственными нарушениями метаболизма (болезни накопления гликогена, лизосомальные болезни накопления) или мультиорганными врожденными синдромами и пороками развития, такими как RAS-патии [7-9].
Этиологическими причинами ГКМП-фенотипа у детей могут быть нервно-мышечные и митохондриальные заболевания, которые гораздо реже выявляются у взрослых пациентов [9-12].
Наличие 2-х кардинально различающихся подходов вносит определенную терминологическую путаницу и затрудняет анализ данных, а также эпидемиологические, диагностические и организационные мероприятия.
В настоящий момент в текущих отечественных клинических рекомендациях фенокопии и синдромальные формы не относятся к понятию ГКМП. Краткое их описание приводится с целью обратить внимание врачей на необходимость их идентификации и проведения дифференциального диагноза.
1.2. Этиология и патогенез заболевания или состояния (группы заболеваний или состояний)
Этиология ГКМП
В 1990-х годах ХХв была выдвинута теория моногенного происхождения ГКМП, т.е. допущение, что единственного молекулярного события достаточно для развития заболевания [13].
По мере накопления данных оказалось, что приблизительно в половине случаев заболевание развивается в результате носительства патогенных и вероятно патогенных вариантов в генах, кодирующих саркомерные белки кардиомиоцитов [1][14-17].
Около 60% пациентов имеют отягощенную семейную историю — хотя бы одного родственника с диагностированной КМП, а около 40% являются первыми больными в семье [1].
В семейных случаях у 70-75% пробандов в родословной прослеживается аутосомно-доминантный тип наследования, на долю аутосомно-рецессивных и сцепленных с полом форм приходится ~15% случаев [3].
ГКМП является заболеванием c выраженной анатомической, клинической и генетической гетерогенностью. ГКМП может манифестировать в любом возрасте. Средний возраст манифестации заболевания у взрослых составляет ~40 лет [18].
Дебют ГКМП в детском и подростковом возрасте, а также у молодых взрослых часто ассоциирован с семейной формой заболевания и более тяжелым течением [3][9][19-25].
Большая часть известных мутаций локализована в генах, кодирующих белки толстых (MYH7, MYBPC3) и тонких (TPM1, TNNT2, TNNI3, MYL2, MYL3, ACTC1) миофиламентов структуры саркомера [1][3][16].
Поиск мутаций в 8 генах с доказанной патогенетической ролью в развитии ГКМП позволяет выявить причинные генетические варианты у 60-85% первичных пациентов в зависимости от исследуемой когорты [1][3][16][19-24].
На долю причинных вариантов в генах MYH7 и MYBPC3 приходится около половины всех случаев генотип-позитивных пробандов с ГКМП [1][3][16][19-24][26-29].
В большинстве случаев причинные варианты, ассоциированные с ГКМП, представляют собой уникальные замены, описанные однократно или всего для нескольких случаев. Частота каждой такой замены среди всех генетических причин ГКМП не превышает 1% [11][30][31].
У части пациентов (5-7% пробандов) заболевание может развиваться на фоне носительства нескольких (2, 3) патогенных и вероятно-патогенных вариантов. Наиболее часто встречаются комбинации мутаций в генах, кодирующих саркомерные белки. В этом случае заболевание характеризуется более ранним дебютом (часто в детском возрасте), большей степенью гипертрофии МЖП и более высоким риском развития синдрома ВСС [3][20][25][32-35].
ВСС при ГКМП возможна и при отсутствии значимой ГЛЖ, подобные случаи наиболее часто ассоциированы с мутациями в гене тропонина Т (TNNT2) [29][36][37].
Помимо вышеперечисленных 8 саркомерных генов к настоящему времени описаны более 40 генов, кодирующих как саркомерные (TTN, MYH6, ACNT2, TNNC1 и т.д.), так и несаркомерные белки миокарда (CSRP3, FHL1, PLN, FLNC и т.д.), в которых были выявлены редкие генетические варианты, предположительно ассоциированные с ГКМП [16].
Однако уровень доказательности для большинства этих генов остаётся невысоким [38]. В 2019г международная экспертная группа консорциума ClinGen провела анализ доказательности причинной взаимосвязи редких находок в 33 описанных генах с развитием ГКМП1. Только для 8 генов (MYBPC3, MYH7, TNNT2, TNNI3, TPM1, ACTC1, MYL2, MYL3) причинный характер мутаций был оценен как установленный (definitive), для 3 генов (CSRP3, TNNC1, JPH2) причинность имела средний уровень доказательности (moderate), а для остальных генов доказательность их роли в патогенезе ГКМП была ограниченной (limited) или отсутствовала [39][40].
При секвенировании всего генома было обнаружено, что 20% случаев с ГКМП без известной мутации в гене саркомера связано с патологическими вариантами в некодирующих областях или в генах, ранее не идентифицированных как связанных с клиническим фенотипом ГКМП. Анализ интронных областей на основе WGS позволяет выявить патогенный вариант еще у 9% пациентов с семейной ГКМП [23][41].
С другой стороны, выявление вариантов IV и V классов патогенности у членов семьи, которые не соответствуют клиническим диагностическим критериям ГКМП, также является распространенным явлением. Данное обстоятельство позволяет высказать предположение, что механизмы, ответственные за фенотипические проявления заболевания, зависят не только от причинных мутаций в генах белков саркомера. Патогенез во многом может определяться наличием комбинации других генетических вариантов, которые либо компенсируют, либо способствуют неблагоприятным последствиям мутации, а также негенетическими причинами или факторами окружающей среды [23].
Наблюдение за взрослыми членами семьи пробанда показало, что только у 10% генотип-позитивных пациентов развивается клинический фенотип ГКМП, при этом у подавляющего большинства из них — в пожилом возрасте. И, наконец, нельзя игнорировать хорошо известный факт, что у 50% пациентов с установленным клиническим диагнозом ГКМП не выявляют мутаций в генах, кодирующих выработку сократительных белков, классифицируемых как патогенные или вероятно патогенные [11][17][42].
По данным визуализирующих методов в этой когорте пациентов продемонстрирована значимо более высокая частота выявления систолического движения передней створки МК в сочетании с динамической обструкцией в ВТЛЖ (52%) и наличием кальциноза кольца МК (27%) [17][43].
Пациенты с ГКМП, включенные в регистр EORP (EurObservational Research Program), имеют высокую распространенность сердечно-сосудистых факторов риска, сравнимую с данными в общей европейской популяции. Пациенты с ГКМП в сочетании с артериальной гипертензией (АГ) и ожирением характеризовались более старшим возрастом, несемейной формой ГКМП, более высоким классом хронической сердечной недостаточности (ХСН) по NYHA и большей степенью выраженности диастолической дисфункции ЛЖ [43-52].
Результаты полногеномного секвенирования показали, что у пациентов с ГКМП без АГ было больше идентифицировано патогенных вариантов, в то время как у пациентов с ГКМП и АГ чаще встречались варианты неопределенной клинической значимости (64% vs 24%, P<0,05) [53].
В некоторых когортах до 40% пациентов с "классической" ГКМП не имеют ни семейного анамнеза заболевания, ни патогенной мутации саркомера. Маловероятным также является то, что будут идентифицированы новые варианты генов, кодирующих сократительные белки или варианты других генов, которые подтвердят моногенную этиологию для подгруппы "несемейной ГКМП" [17][54].
Обсуждается гипотеза многофакторного генеза ГКМП [16][17][23][54-57].
Молекулярный патогенез ГКМП
Причиной ГКМП наиболее часто являются мутации в генах, кодирующих сократительные белки миокарда. В основе молекулярного патогенеза таких вариантов ГКМП часто лежит нарушение кальциевого гомеостаза и повышение чувствительности миофиламентов к ионам кальция. Это проявляется в усилении силы сокращения саркомера в систолу, снижении степени его расслабления в диастолу на фоне повышенной потребностей кардиомиоцита в аденозинтрифосфорной кислоте, что влечет нарушение внутриклеточных сигнальных процессов и реактивацию компенсаторных эмбриональных программ гипертрофического роста [39][58].
На уровне кардиомиоцитов данные процессы приводят к повышению синтеза эмбриональных форм саркомерных белков и активации киназных сигнальных каскадов, обеспечивающих процессы собственно гипертрофии кардиомиоцитов, а также к усилению внеклеточных сигнальных систем, направленных на пролиферацию фибробластов, трансформации фибробластов в миофибробласты и дисбаланс в системе коллагенолиза [39][58][59].
На гистологическом уровне отражением прямого действия "причинного" генетического варианта и молекулярного патогенеза является дискомплексация кардиомиоцитов и мышечных волокон — феномен "disarray", а также фиброз разной степени выраженности [3][20][39][59-65].
Этиология и патогенез фенокопий ГКМП
Этот раздел внесен в клинические рекомендации по ГКМП (2023) с целью обратить внимание врачей на необходимость проведения дифференциального диагноза ГКМП с фенокопиями и синдромными формами ГКМП, у которых при визуализации выявляется ГКМП-фенотип. Фенокопия ГКМП это заболевание по морфофункциональному фенотипу похожее на ГКМП по данным рутинных методов исследования (ЭКГ, ЭхоКГ), но отличающееся иным этиопатогенезом и возможностью этиопатогенетической терапии для отдельных нозологий.
Еще раз необходимо подчеркнуть, что в соответствие с текущей классификацией ГКМП ЕОК данные формы относятся к понятию ГКМП. Однако в рамках текущей версии отечественных рекомендаций рассматриваются в качестве отдельной группы и вынесены за рамки понятия ГКМП [66].
Наиболее часто встречающиеся фенокопии ГКМП и их молекулярный патогенез представлены в таблице 1, Приложение А32 [67-76].
Патогенез симптомов и синдромов ГКМП
Патогенез ГКМП на органном уровне заключается в совокупности нескольких синдромов: обструкции ВТЛЖ, ишемии миокарда, систолической и диастолической дисфункции ЛЖ, аритмическом синдроме, ХСН, легочной гипертензии (ЛГ), формировании верхушечной аневризмы ЛЖ, автономной дисфункции сердца.
Синдром обструкции ВТЛЖ
В создании обструкции ВТЛЖ участвуют структурные, кинетические и геометрические факторы [77].
1. Структурные аномалии:
a. сужение ВТЛЖ гипертрофированной МЖП (уменьшение степени обструкции ВТЛЖ после миоэктомии/ЭСА обусловлено воздействием на этот фактор);
b. SAM-синдром (передне-систолическое движение створок МК);
c. уменьшенная полость ЛЖ;
c. аномалии папиллярных мышц (и другие малые аномалии сердца) (гипертрофия и дислокация, добавочная папиллярная мышца);
c. апикально-базальный мышечный пучок.
2. Кинетические факторы — гиперсократимость ЛЖ и ускорение кровотока в ВТЛЖ;
3. Геометрические факторы:
a. переднее смещение МК, точка коаптации створок МК смещена ближе к МЖП [78];
b. малый аорто-митральный угол (<120°).
Чем больше факторов имеется у конкретного пациента, тем более выражен синдром обструкции ВТЛЖ.
SAM-синдром (переднее систолическое движение (ПСД) МК) обусловлен следующими факторами:
a) аномалии створок МК (удлинение, избыточность);
b) нарушение координации кровотока в полости ЛЖ в раннюю систолу, в результате чего на створки МК действует сила, сдвигающая их в сторону ВТЛЖ [79][80];
c) аномалии хорд МК;
d) меньшее соотношение длины передней и задней створок МК (<1,3), при этом точка коаптации створок МК смещается кпереди ближе к ВТЛЖ [81-83].
У пациентов с латентной обструкцией провоцирующими ее факторами являются: увеличение сократимости ЛЖ при нагрузке, приводящее к уменьшению конечно-систолического размера ЛЖ и переднему смещению МК; ускорение кровотока в ВТЛЖ в период систолы, усугубляющее SAM-синдром (ПСД МК) [84].
У пациентов с ГКМП может быть лабильная обструкция, характеризующаяся значительными спонтанными колебаниями внутрижелудочкового ГД без видимой причины [85].
Кроме обструкции ВТЛЖ, у пациентов с ГКМП может наблюдаться среднежелудочковая обструкция. Среднежелудочковая обструкция развивается у пациентов с гипертрофией срединных сегментов МЖП и, как правило, в сочетании с гипертрофией папиллярных мышц [86-88].
При комбинированной гипертрофии (МЖП + апикальные сегменты) может быть 2-уровневая обструкция (срединно-желудочковая + на уровне ВТЛЖ) [89].
Митральная регургитация
Митральная регургитация (МР) может быть обусловлена как врожденными аномалиями МК (удлинение, избыточность, изменение соотношения длины передней и задней створок), так и в сочетании с пролапсом МК.
Факторы, участвующие в МР:
— врожденные аномалии МК (расщепление створки);
— ПСД МК (SAM-синдром) с обструкцией ВТЛЖ (подтягивание передней створки МК в область ВТЛЖ за счет эффекта Вентури, что нарушает коаптацию створок МК);
— пролапс створок МК;
— изменения подклапанного аппарата МК (переднее смещение папиллярных мышц, апикальное смещение папиллярных мышц, разрыв хорд МК и др.);
— приобретенные изменения МК (ревматические);
— дегенеративные изменения створок МК с их утолщением, в сочетании с кальцинозом митрального кольца и ограничением подвижности задней створки МК (как правило в старшей возрастной группе).
Типичное направление тока МР, обусловленной SAM-синдромом (ПСД МК) в левом предсердии (ЛП) — кзади и латерально. Однако центральное и переднее направление тока МР также возможно, что не позволяет по направлению тока МР делать ввод о ее природе.
Увеличение толщины створок МК и аортального клапана (АК), сочетание МР и небольшой аортальной регургитации может наблюдаться при некоторых фенокопиях ГКМП, в частности, при кардиальном амилоидозе. Данное обстоятельство важно помнить при проведении дифференциального диагноза, особенно у пациентов старшего возраста.
Синдром ишемии миокарда ЛЖ
У пациентов с ГКМП при интактных коронарных артериях может развиваться ишемия миокарда. В англоязычной литературе используют термин INOCA (ischemia and no obstructive coronary artery) [90].
Факторы, приводящие к ишемии миокарда:
a) относительная коронарная недостаточность (уменьшение резерва коронарного кровотока при выраженной гипертрофии);
b) ишемия субэндокардиальных слоев миокарда за счет компрессии интрамуральных коронарных артерий;
c) периваскулярный фиброз, при этом интрамуральные коронарные артерии не могут расшириться во время физической нагрузки (ФН), когда возрастает потребность миокарда в кислороде и требуется увеличение коронарного кровотока;
d) врожденная патология коронарных артерий — "миокардиальные мышечные мостики" и интрамуральное расположение ветвей крупных коронарных артерий;
e) помимо перечисленных причин, у 15-25% пациентов наблюдают сопутствующий атеросклероз в эпикардиальных коронарных артериях (в старшей возрастной группе пациентов).
У пациентов с ГКМП и фенокопиями ГКМП может развиваться инфаркт миокарда (ИМ) как 2 типа, (без атеротромбоза), так и 1 типа. Факторы риска развития ИМ 2 типа у пациентов с ГКМП представлены в таблице 2, Приложение А3 [91-106].
Синдром дисфункции ЛЖ
Диастолическая функция ЛЖ может быть нарушена уже у носителей мутации, в догипертрофической стадии ГКМП [107].
При ГКМП нарушения касаются двух основных детерминант диастолического наполнения ЛЖ — активной релаксации и растяжимости миокарда. Гипертрофия миокарда per se вызывает нарушение активного расслабления. Хаотическое расположение сократительных элементов (disarray) и интерстициальный фиброз приводят к снижению податливости ЛЖ, и, как следствие, к возрастанию сопротивления наполнению ЛЖ и повышению давления наполнения. В начальных стадиях ГКМП нарушено только активное расслабление миокарда, при этом давление в ЛП не увеличено. По мере прогрессирования гипертрофии, развития фиброза, нарастания степени МР, присоединения ишемии миокарда диастолические нарушения нарастают, приводя к увеличению давления в ЛП (соответственно, и к увеличению конечно-диастолического давления ЛЖ). Также выраженная диастолическая дисфункция может приводить к развитию ЛГ у некоторых пациентов (ЛГ у 50% симптомных пациентов) [108-111].
Систолическая функция ЛЖ может оцениваться как по параметрам сократимости, так и по объемным показателям.
Глобальная систолическая функция ЛЖ, оцениваемая по параметрам сократимости, у пациентов с ГКМП сверхнормальная, что выражается высокой фракцией выброса (ФВ) ЛЖ. Следует учесть, что показатель ФВ при ГЛЖ и маленьком ЛЖ может некорректно характеризовать сократимость. Региональная систолическая функция ЛЖ гетерогенна: гипертрофированные сегменты ЛЖ гипокинетичны (снижена степень систолического утолщения и деформация), а негипертрофированные сегменты имеют нормальную/сверхнормальную сократимость.
Объемным показателем систолической функции ЛЖ является величина ударного объема (УО). При ГКМП и уменьшенном ЛЖ (малый конечно-диастолический объем (КДО)) УО снижен, несмотря на высокую ФВ ЛЖ. Также снижена возможность прироста УО при ФН.
Систолическая функция ЛЖ, анализируемая по систолической деформации, может быть нарушена уже у носителей ГКМП-мутации, на догипертрофической стадии.
При прогрессировании заболевания (негативное ремоделирование, adverse remodeling) в дилатационной стадии наблюдается уменьшение степени гипертрофии ("выгорание"), сопровождаемое снижением общей сократимости ЛЖ (ФВ <50%) [108][110][112-116].
ПЖ при ГКМП
У 30-44% пациентов с ГКМП наблюдаются структурные и функциональные нарушения в ПЖ. Критерием гипертрофии миокарда ПЖ считается увеличение толщины стенки ПЖ >5 мм. Толщина миокарда ПЖ >10 мм считается экстремальной гипертрофией ПЖ [117].
Гипертрофия ПЖ в единичных случаях бывает изолированной, без ГЛЖ [118].
Структурное ремоделирование ПЖ в 15-90% приводит к внутрижелудочковой обструкции, которая может быть на уровне срединных сегментов ПЖ или на уровне ВТПЖ [119].
Критерием наличия обструкции ВТПЖ считается увеличение ГД в ВТПЖ >16 мм рт.ст. в покое [120].
Увеличение толщины ПСПЖ у пациентов старше 60 лет с ГКМП-фенотипом требует исключения кардиального амилоидоза.
Систолическая дисфункция ПЖ проявляется уменьшением продольной деформации ПЖ; при этом другие показатели систолической функции ПЖ (TAPSE и s’ латеральной части трикуспидального кольца), как правило, в пределах нормальных значений.
Диастолическая дисфункция ПЖ в начальных стадиях характеризуется Е/А <1, увеличением RV DecT (время замедления кровотока в фазу раннего наполнения ПЖ), E/e’ >6,0. Показано, что наличие диастолической дисфункции ПЖ является предиктором ВСС и ХСН [111][117][119-123].
ВСС
В основе патогенеза ВСС лежат фатальные нарушения ритма, вызванные ишемией миокарда и электрической нестабильностью. ВСС чаще обусловлена фибрилляцией желудочков (ФЖ) (62,4%), брадиаритмиями (16,5%), желудочковой тахикардией (ЖТ) типа "torsades de pointes" (12,7%), ЖТ (8,3%) и асистолией.
ВСС поражает пациентов с ГКМП в любом возрасте (даже старше 60 лет), с пиком в период от 30 до 50 лет. В отличие от аритмогенной КМП, при которой существует четкая связь между интенсивными физическими упражнениями и повышенным риском ВСС (данные регистра КМП Великобритании), ВСС при ГКМП в большинстве случаев возникала в покое или при обычной ФН [1][95][124-137].
Синкопы
Синкопальные состояния могут быть обусловлены как аритмическими, так и гемодинамическими причинами. К гемодинамическим причинам относят ситуативное увеличение обструкции ВТЛЖ (ФН), вызывающее значимое уменьшение УО и падение артериального давления (АД), а также снижение периферического сопротивления в результате неадекватной вазодилатации, в т.ч. вазовагальные обмороки (см. также Приложение Б8) [138-141].
Фибрилляция предсердий
Факторы:
a) "предсердная миопатия" — показано, что функция ЛП нарушена у носителей мутации в доклинической стадии до развития гипертрофии [142].
b) структурное (дилатация) и функциональное ремоделирование ЛП, приводящее к электрической нестабильности;
c) интерстициальный фиброз ЛП [143-150].
Известно, что фибрилляция предсердий (ФП) — частый симптом при фенокопиях ГКМП, например, частота выявления ФП при амилоидозе сердца может достигать 69%. Причина увеличения ЛП многофакторна. Необходимо отметить, что нарушение сократительной функции ЛП при транстиреиновой (ТТР) амилоидной КМП не зависит от размера ЛП [151].
ХСН
Факторы:
a) уменьшенный ЛЖ (малый КДО) и, несмотря на высокую ФВ ЛЖ, малый УО ЛЖ;
b) неспособность увеличить в должной степени УО при ФН;
c) обструкция ВТЛЖ, вносящая вклад в уменьшение УО;
d) систолическая дисфункция ЛЖ при прогрессировании ГКМП, особенно в дилатационной стадии (ишемия миокарда, диссинхрония ЛЖ);
e) диастолическая дисфункция ЛЖ (фиброз миокарда, повышение давления в ЛП и конечно-диастолического давления);
f) МР (вносит вклад в повышение давления в ЛП);
g) нарушения ритма (ФП);
h) ЛГ [108][114][116][147][148][152-155].
У 10% пациентов с ГКМП с "классическим фенотипом" в покое при ультразвуковом исследовании легких регистрируются В-линии, что свидетельствует о застое в легких. При стресс-ЭхоКГ частота выявления В-линий возрастает до 30%. У этих больных при ФН усугубляется диастолическая дисфункция, возрастает МР и давление в легочной артерии (ЛА) [156].
Формирование верхушечной аневризмы ЛЖ
Частота развития верхушечной аневризмы составляет примерно 2-3% от всех случаев ГКМП [157][159].
Верхушечные аневризмы при ГКМП могут развиваться как при изолированной верхушечной ГЛЖ, так и при морфологических вариантах, когда гипертрофия развивается преимущественно в средних сегментах ЛЖ (конфигурация "песочных часов") или при смешанных вариантах, когда гипертрофия развивается в верхушечных и средних сегментах ЛЖ [159].
При среднежелудочковой ОГКМП верхушечные аневризмы ЛЖ присутствуют более чем в 20% случаев [87].
Развитие верхушечной аневризмы ЛЖ при ГКМП обусловлено сочетанием факторов, взывающих ишемию миокарда при ГКМП и дополнительным фактором — систолическая среднежелудочковая обструкция вызывает резкое повышение давления в верхушке ЛЖ, что приводит к снижению коронарной перфузии, особенно в субэндокардиальных слоях миокарда и апоптозу кардиомиоцитов [160][161].
По размеру верхушечные аневризмы разделяют на малые (<2 см), средние (2-4 см) и большие (>4 см). Не выявлено взаимосвязи между размером аневризмы и клиническим исходом [159].
Но имеются данные о том, что ~20% случаев тромбоэмболических событий и образования тромба в верхушке ЛЖ произошло при аневризмах малых размеров, в то время как ~70% событий ВСС было у пациентов со средними и большими аневризмами [159].
Верхушечные аневризмы являются независимым предиктором потенциально летальных аритмий, включая неустойчивую и устойчивую ЖТ и ФЖ [162-165].
Области рубцевания миокарда, прилегающие к рубцовому ободку аневризмы на стыке жизнеспособной и аномальной ткани, где возникают контуры re-entry, представляют собой первичный аритмогенный субстрат для возникновения злокачественных желудочковых тахиаритмий независимо от размера аневризмы [159].
Наличие верхушечной аневризмы ассоциировано с 4-кратным увеличением риска ВСС и 6-кратным увеличением риска тромбоэмболических событий/образованием тромба в верхушке ЛЖ [166].
В 2020г наличие верхушечной аневризмы (независимо от размера) впервые вошло в список установленных клинических факторов риска ВСС при ГКМП [1].
Верхушечные аневризмы могут развиваться и при болезни Фабри (до 10% случаев), как при ее типичной морфологической форме (симметричной ГЛЖ), так и при атипичных — асимметричной и апикальной [167].
Автономная дисфункция
Показано, что у пациентов с ГКМП нарушена симпатическая иннервация в сердце и эти нарушения прогрессируют при развитии негативного ремоделирования (систолическая дисфункция и дилатационная стадия) [168].
Признаками дисфункции вегетативной нервной системы является неадекватная реакция АД и частоты сердечных сокращений (ЧСС) на нагрузку. Следует учитывать, что неадекватная реакция АД на ФН также может быть обусловлена чисто гемодинамическими причинами — недостаточным приростом УО при ФН (малый КДО ЛЖ + нарушение диастолического наполнения ЛЖ + увеличение обструкции ВТЛЖ при ФН).
Недостаточным приростом АД при ФН считается увеличение АД менее, чем на 20 мм рт.ст. на пике ФН или падение АД ≥20 мм рт.ст. от пиковой в процессе ФН [1].
У пациентов с ГКМП также выявляется недостаточный прирост ЧСС при ФН (резерв ЧСС — отношение пиковой ЧСС к исходной при стресс-ЭхоКГ). Степень снижения резерва ЧСС не зависит от приема бета-блокаторов и является независимым предиктором плохого прогноза [169].
Следует учитывать, что в старшей возрастной группе пациентов наличие автономной дисфункции требует исключения кардиальных форм амилоидоза.
ЛГ
Гистологические данные показывают, что у пациентов с ОГКМП происходит ремоделирование как артериальных, так и венозных сосудов легких. Отмечается гипертрофия сосудистой стенки и увеличивается доля фиброзной ткани. При этом повышение давления в ЛА может быть небольшим [170].
У 20% пациентов с ГКМП и нормальным давлением в ЛА в покое регистрируется его повышение при стресс-ЭхоКГ [171].
ЛГ (среднее давление в ЛА ≥25 мм рт.ст. при инвазивном измерении) выявляется у 50% симптомных пациентов с ХСН с показаниями к редукции МЖП. У некоторых больных (до 10%) диагностируется прекапиллярная ЛГ (давление заклинивания ЛА ≤15 мм рт.ст., легочное сосудистое сопротивление >3,0 единиц Вуда). Пациенты с прекапиллярной ЛГ по другим параметрам значимо не отличались от других пациентов с ГКМП и ЛГ. Степень повышения давления в ЛА в диапазоне 40-60 мм рт.ст. После СМЭ давление в ЛА снижается, но не до нормальных величин [108][172].
ЛГ является предиктором плохого прогноза при ГКМП.
1.3. Эпидемиология заболевания или состояния (группы заболеваний или состояний)
При ГКМП нет четкой географической, этнической или половой структуры распределения.
ГКМП — практически единственное кардиоваскулярное заболевание, которое может манифестировать в любом возрасте человека от младенчества до глубокой старости (с первых дней до 90 и более лет); при этом средний возраст пациентов при установке диагноза составляет 30-40 лет.
Согласно данным эпидемиологических исследований, проводимых в разных частях света, распространенность ГКМП составляет 1:500 в общей популяции. В разных возрастных когортах она варьируется от 1:500 до 1:200.
При применении более чувствительных методов визуализации (магнитно-резонансная томография (МРТ), компьютерная томография (КТ)) и более широком использовании генетического тестирования и каскадного скрининга для родственников первой линии родства распространенность ГКМП соответствует 0,6% (1:167).
Частота в общей популяции превышает встречаемость ГКМП в кардиологической практике, т.к. большая часть пациентов остается неидентифицированной ввиду бессимптомности. При выявлении гипертрофии сердца в старших возрастных группах и толщине стенки ЛЖ ≥12 мм необходимо учитывать возможность фенокопий ГКМП и вторичной ГЛЖ [34][173][174].
В первую очередь это касается ТТР амилоидных КМП. Выделяют два типа ТТР-КМП — нативного, нормального "дикого" типа, приобретенный ненаследственный амилоидоз сердца, к которому относится большинство случаев болезни и наследственного типа [175]. C 2020г амилоидная ТТР-КМП входит в перечень редких (орфанных) заболеваний. Амилоидные ТТР-КМП часто не диагностируются из-за того, что напоминают другие причины ГЛЖ, такие как ГКМП, АГ и аортальный стеноз (АС). В когортах пациентов с АС и транскатетерной заменой АК распространенность приобретенного кардиального TTR wt-амилоидоза соответствовала 16%, из которых в 62% случаев выявлены критерии низкоградиентного низкопотокового АС [176].
1.4. Особенности кодирования заболевания или состояния (группы заболеваний или состояний) по Международной статистической классификации болезней и проблем, связанных со здоровьем
МКБ-10
I42.1 — Обструктивная гипертрофическая кардиомиопатия.
I42.2 — Другая гипертрофическая кардиомиопатия.
1.5. Классификация заболевания или состояния (группы заболеваний или состояний)
В повседневной клинической практике применяют несколько классификационных подходов — клинический, гемодинамический, морфологический, генетический.
Клинические варианты течения ГКМП — см. Раздел 1.6.
Гемодинамический принцип классификации
В зависимости от наличия или отсутствия обструкции ВТЛЖ в покое и при нагрузке выделяют следующие варианты ГКМП:
— необструктивная ГКМП: ГД в ВТЛЖ <30 мм рт.ст. в покое и при нагрузке;
— обструктивная ГКМП: ГД в ВТЛЖ >30 (50) мм рт.ст. в покое и при нагрузке. В том числе латентная обструкция, при которой ГД в ВТЛЖ <30 в покое и >30 (50) мм рт.ст. при нагрузке (подробнее критерии обструкции ВТЛЖ см. в Разделе "Диагностика").
Морфологический принцип классификации ГКМП
1. Асимметричная форма ГКМП:
• Гипертрофия МЖП (+/- вовлечение ПЖ);
— Базальной части МЖП (субаортальная);
— Сигмовидная МЖП;
— Гипертрофия всей МЖП;
— Двояковыпуклая МЖП (англ. "reverse curve") — преимущественно среднежелудочковая гипертрофия МЖП без вовлечения свободной стенки ЛЖ [177-180];
• Комбинированная (МЖП + другой отдел ЛЖ или ПЖ);
• Гипертрофия другой стенки ЛЖ (боковая, задняя);
2. Апикальная гипертрофия (+/- срединные сегменты ЛЖ);
3. Среднежелудочковая ГКМП (с вовлечением срединных отделов не только МЖП, но и свободной стенки ЛЖ, ЛЖ типа "песочные часы");
4. Симметричная форма ГКМП.
По данным многоцентрового регистра пациентов с ГКМП, >80% пациентов c ГКМП относятся к двум морфологическим подтипам — гипертрофия базальной части МЖП (46%) и двояковыпуклая МЖП (38%) [179].
Концентрическая ГКМП составляет 1% случаев, среднежелудочковая ОГКМП с формированием верхушечной аневризмы — 3%, верхушечная ГКМП — 8%.
Клинические особенности наиболее часто встречающихся морфологических подтипов ГКМП представлены в таблице 3, Приложение А3.
Классификация ГКМП по степени выраженности гипертрофии:
- "Умеренная" (в англоязычной литературе используется термин "mild"): максимальная толщина стенки ЛЖ <18 мм;
- Промежуточная;
- Экстремальная (максимальная толщина стенки ЛЖ ≥30 мм).
Классификация КМП MOGE(s) выделяет не только "классические" морфофункциональные фенотипы (гипертрофический, дилатационный, рестриктивный, аритмогенная дисплазия, некомпактный миокард), но и смешанные фенотипы [27][181][182].
Клинико-морфологическая классификация по стадиям ГКМП
В 2012г Olivotto I, et al. [183] выделили 4 стадии развития ГКМП:
1 стадия: догипертрофическая — этап в развитии заболевания у лиц, являющихся носителями мутаций, вызывающих ГКМП, при которой отсутствуют признаки гипертрофии миокарда, определяемые с помощью визуализирующих методов.
2 стадия: "классический фенотип" ГКМП — этап, при котором гипертрофический фенотип полностью выражен, ЛЖ гипердинамичен (ФВ ЛЖ >65% по данным МРТ), при отсутствии обширных фиброзных изменений, свидетельствующих о прогрессировании заболевания.
3 стадия: негативное ремоделирование — этап, который определяется наличием неблагоприятных структурных изменений, накладывающихся на "классический" фенотип ГКМП, выражающихся в нарастающем фиброзе ЛЖ и ухудшении систолической функции ЛЖ (ФВ ЛЖ в диапазоне от 50% до 65%), при относительно сохранном клиническом и гемодинамическом статусе.
4 стадия: выраженная дисфункция — этап клинического развития ГКМП, характеризующийся систолической дисфункцией ЛЖ (ФВ ЛЖ <50%), сопровождающийся крайней степенью фиброза и ремоделирования и обычно связанный с гемодинамической декомпенсацией и неблагоприятным исходом.
В настоящих рекомендациях 3 и 4 стадия объединены термином "негативное ремоделирование".
ЭхоКГ признаки "классического фенотипа" ГКМП:
- асимметричная ГЛЖ;
- размер полости ЛЖ в пределах нормальных значений/уменьшенный;
- ФВ ЛЖ >65%;
- обструкция ВТЛЖ;
- диастолическая функция ЛЖ сохранена или диастолическая дисфункция ЛЖ 1 степени.
1.6. Клиническая картина заболевания или состояния (группы заболеваний или состояний)
ГКМП — заболевание, характеризующееся выраженной гетерогенностью клинических проявлений.
Клинические варианты течения ГКМП:
1. ВСС — может отмечаться при любом варианте течения ГКМП, в т.ч. без предшествующей симптоматики (наиболее часто встречается у молодых пациентов <35 лет, включая спортсменов);
2. Бессимптомное течение — встречается у пациентов с исходно необструктивной формой ГКМП (небольшая степень гипертрофии миокарда, без сопутствующих аномалий МК). Продолжительность жизни у этих пациентов как в общей популяции — 75 лет и более;
3. Симптомное стабильное (на фоне медикаментозной терапии) доброкачественное течение:
a) у пациентов с исходно необструктивной формой ГКМП;
b) при ОГКМП с небольшой степенью обструкции ВТЛЖ;
4. Симптомное осложненное течение ГКМП проявляется:
a) ФП — пароксизмальная, персистирующая или постоянная (от 25 до 30%), ассоциированная с сердечной недостаточностью различной степени выраженности и повышенным риском тромбоэмболических осложнений, включая инсульт;
b) ХСН — появление одышки, слабости, утомляемости, в сочетании, пресинкопы и синкопы, аритмии. Нарастание тяжести ХСН до III-IV функционального класса (ФК) (NYHA) при сохраненной систолической функции ЛЖ;
c) Синдром стенокардии (в т.ч. атипичный болевой синдром) или безболевая ишемия. Ишемия миокарда при ГКМП может осложняться ИМ 2 типа;
d) "Конечная стадия": дальнейшее прогрессирование явлений застойной сердечной недостаточности, связанной с негативным ремоделированием и выраженной систолической и диастолической дисфункцией ЛЖ;
e) Развитие верхушечной аневризмы ЛЖ.
Симптомы ХСН встречаются часто, но ее клинический профиль (IV стадия по Оливотто) различается у разных пациентов. У одних сердечная недостаточность связана с диастолической дисфункцией при сохраненной ФВ и малых размерах ЛЖ (рГКМП) или обструкцией ВТЛЖ (с МР или без нее), в других, симптомы вызваны систолической дисфункцией ЛЖ (дГКМП). При этом к основному ГКМП-фенотипу присоединяется дополнительный фенотип — дилатационный или рестриктивный, обозначаемые как дГКМП или рГКМП, соответственно. Степень увеличения ЛЖ в дГКМП, как правило, небольшая, более того, размер и объем ЛЖ может быть в пределах нормальных значений, но при этом динамика свидетельствует о дилатации (например, конечно-диастолический размер ЛЖ 35 мм → 55 мм, при условии корректного измерения). В дГКМП может наблюдаться уменьшение толщины миокарда ЛЖ — так называемый феномен "выгорания гипертрофии", обусловленный гибелью кардиомиоцитов. При ГКМП важно признание гетерогенности механизмов сердечной недостаточности, поскольку это влияет на лечение и прогноз [35][116][183][184].
Формализованный подход, предложенный Rowin EJ, et al., к оценке вариантов клинического течения предлагает учитывать наличие у пациента одного и более одного синдрома (ХСН+ФП, ХСН+ВСС, ФП+ВСС, ХСН+ФП+ВСС) и использование термина "прогрессирующее течение симптомной ГКМП" [185].
Основные клинико-морфологические варианты течения и исходы заболевания при ГКМП представлены в таблице 4, Приложение А3 [3][20][61][185-191].
Общие принципы формулировки диагнозов при ГКМП
Наряду с морфофункциональным классом необходимо указать:
- Семейная форма;
— генетический вариант обнаружен — класс патогенный или вероятно патогенный;
— генетический вариант не обнаружен;
— генетическое исследование не проводилось;
- Несемейная форма;
— генетический вариант обнаружен, мутация de novo — класс патогенный или вероятно патогенный;
— генетический вариант не обнаружен;
— генетическое исследование не проводилось;
- Вариант ГЛЖ (асимметричная/симметричная);
- Паттерн морфологии МЖП (двояковыпуклая, базальная гипертрофия, верхушечная и т.д.);
- Указать гемодинамический вариант: обструктивная (в т.ч. латентная)/необструктивная;
- Указать клинический вариант;
— ВСС;
— бессимптомное течение;
— симптомное стабильное (на фоне медикаментозной терапии);
— прогрессирующее;
- Отразить в диагнозе стадию по Olivotto (I-IV ст.) и варианты негативного ремоделирования;
— дГКМП;
— рГКМП;
— наличие верхушечной аневризмы ЛЖ;
- Необходимо указать в диагнозе расчетный риск ВСС и дату на момент стратификации.
Калькулятор риска ВСС (с учетом европейской и американской модели) представлен на сайте https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator (при выполненной МРТ с контрастированием — внести сведения о позднем накоплении гадолиний-содержащего контрастного вещества (ПНГ))
Варианты формулировки диагноза ГКМП после редукции МЖП:
— Состояние после СМЭ МЖП из аорты по Морроу (дата);
— Состояние после расширенной миоэктомии МЖП доступом через верхушку ЛЖ (дата) ГД в ВТЛЖ;
— Состояние после расширенной миоэктомии МЖП доступом через ПЖ (дата) ГД в ВТЛЖ;
— Состояние после расширенной миоэктомии МЖП двужелудочковым доступом (дата) ГД в ВТЛЖ;
Добавлять: с видеоподдержкой/с мобилизацией сердца; в условиях ИК (периферического ИК), гипотермии и фармакохолодовая кристаллоидная кардиоплегия/кровяная кардиоплегия (дата);
— Имплантация двухкамерного имплантируемого кардиовертера-дефибриллятора (ИКД) в эндокардиальном варианте в режиме стимуляции DDD Vitality 2 DR (дата). Коррекция желудочкового электрода. Полное истощение батареи питания (состояние EOL). ХСН IIA ст., II ФК.
— ЭСА. Состояние после ЭСА от (дата).
Примеры формулировки диагноза
- Основной: Несемейная ГКМП (генетическое исследование не проводилось), обструктивная форма. Стадия II по Olivotto. Асимметричная ГЛЖ (максимальная гипертрофия — базальной части МЖП, SAM-синдром. ГД в ВТЛЖ =67 мм рт.ст.). Коронароангиография (КАГ): гемодинамически значимые стенозы коронарных артерий отсутствуют (дата). Синдром стенокардии. Риск ВСС — 3,87% низкий (дата) https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator. Осложнения: МН 0-I ст. ХСН с сохранной ФВ (ФВ ЛЖ 87%), 1 стадия, 2 ФК. Одиночная и парная предсердная экстрасистолия. Желудочковая экстрасистолия 4 градации по Ryan.
- Основной: Кардиомиопатия со смешанным фенотипом: необструктивная семейная ГКМП. Асимметричная ГЛЖ (комбинированная гипертрофия МЖП и передней стенки ЛЖ). Генетическое исследование не проводилось. Риск ВСС — 3,26% низкий (дата) https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator. Бивентрикулярная некомпактная кардиомиопатия. Осложнение: ХСН с сохранной ФВ (ФВ ЛЖ 76%), 1 стадия, 1 ФК.
- Основной: Семейная генетическая необструктивная ГКМП. Стадия по Оливотто IV Дилатационная фаза. Асимметричная ГЛЖ (всей МЖП). Генетический вариант MYBPC3 (сhr11:47360209: С>Т NM_000256.3: R724W), патогенный вариант по классификации Американской коллегии медицинской генетики (ACMG от 2015г). Осложнение. ФП/трепетание предсердий (ТП) пароксизмальная форма (HAS-BLED 2, EHRA II). Желудочковая экстрасистолия 5 гр. по Ryan. Неустойчивая пароксизмальная мономорфная ЖТ. Высокий риск ВСС — (7,87%) (дата) https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator, имплантация ИКД DF-1 (дата) ХСНнФВ (ФВ ЛЖ 35%), 1 стадия, 4 ФК. Асцит. Двусторонний гидроторакс. Гидроперикард. Застойная гепатомегалия. Рецидивирующая тромбоэмболия мелких ветвей легочной артерии (даты). Постановка экстракорпоральной мембранной оксигенации (дата).
- Основной: Семейная необструктивная ГКМП. Стадия по Olivotto II (ФВ ЛЖ 71%). Асимметричная ГЛЖ (вся МЖП). Генетическое исследование не проводилось. Бессимптомное течение. Риск ВСС — 2,89% низкий (дата) https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator. Предстадия сердечной недостаточности.
- Основной: Семейная необструктивная ГКМП. Стадия по Olivotto II. (ФВ 74%) Генетический вариант не определен. Асимметричная ГЛЖ (двояковыпуклая форма МЖП). Риск ВСС — 9,87% высокий (дата). https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator. Впервые выявленная. Осложнение: ФЖ, предотвращенная ВСС (дата). ИКД (дата). Предстадия сердечной недостаточности.
2. Диагностика заболевания или состояния (группы заболеваний или состояний), медицинские показания и противопоказания к применению методов диагностики
Критерии диагноза ГКМП
Критерием диагноза ГКМП у взрослых является увеличение толщины стенки ЛЖ в одном или более сегментах ≥15 мм (определяемое любым визуализирующим методом — ЭхоКГ/МРТ/КТ), которая не объясняется исключительно увеличением нагрузки давлением (см. определение). У родственников пробанда критерием диагноза ГКМП является толщина стенки ЛЖ, равная 13-14 мм [1][3].
Диагностика может быть затруднена в ситуациях сочетания ГКМП с АГ (см. Раздел "ГКМП и АГ"), со стенозом АК, у спортсменов и др. При ГКМП-фенотипе требуется исключение фенокопий ГКМП, в первую очередь наследственного и ненаследственного транстиретинового амилоидоза (ATTR).
Критерием вовлечения ПЖ при ГКМП является увеличение толщины стенки ПЖ >5 мм, а толщина миокарда ПЖ >10 мм считается экстремальной гипертрофией ПЖ [173][192].
Критерием диагноза ОГКМП считается ГД в ВТЛЖ ≥30 мм рт.ст., в покое или провоцируемый. Критерием гемодинамически значимой обструкции, когда требуются более интенсивная терапия или хирургические/эндоваскулярные методы лечения, считается ГД ≥50 мм рт.ст. [1][3][193].
При ГКМП, кроме субаортальной обструкции, может наблюдаться среднежелудочковая обструкция (изолированная или в сочетании с субаортальной). Критерий среднежелудочковой обструкции — ГД ≥30 мм рт.ст. в покое или провоцируемый [1].
Критерием обструкции ВТПЖ считается увеличение ГД в ВТПЖ >16 мм рт.ст. в покое [120].
2.1. Жалобы и анамнез
- У всех пациентов рекомендован детальный анализ жалоб и анамнеза, в т.ч. семейный анамнез до 3-го поколения (сбор анамнеза и жалоб при патологии сердца и перикарда) [1][3][95][194][195].
ЕОК/РКО IC (УДД 5, УУР С)
Комментарии. Многие пациенты не имеют жалоб или они малозначительны. В таких случаях диагноз ставится случайно или по результатам скрининга.
Должен быть решен вопрос об отличии истинного отсутствия симптомов от адаптации за счет образа жизни, путем проведения теста с максимальной переносимой ФН и оценки биомаркеров ХСН в динамике.
В развернутой стадии заболевания при ГКМП наиболее частыми жалобами являются одышка, снижение толерантности к ФН, разнообразные болевые ощущения в грудной клетке кардиалгического и/или стенокардитического характера, нарушения ритма сердечной деятельности (перебои, учащенное сердцебиение), головокружение, пресинкопы и синкопы.
Важно помнить, что манифестация клинических проявлений ГКМП в молодом и пожилом возрасте имеет существенные различия.
Молодой возраст ассоциирован с семейной формой заболевания и является важной детерминантой тяжести течения, риска нежелательных кардиоваскулярных событий, доказанным фактором риска ВСС [25].
Необходимо учитывать все, в т.ч. дополнительные "новые", факторы риска ВСС, особенно у носителей патогенных вариантов, в т.ч. у родственников пробанда — генотип(+)/фенотип(-) (см. соотв. разделы).
При сборе семейного анамнеза обращают внимание на то, были ли у родственников указания на ВСС, ХСН, синкопальные состояния, имплантированные электрокардиостимуляторы (ЭКС), инсульт в молодом возрасте и другие системные заболевания.
Пожилой возраст ассоциирован с несемейной формой заболевания и коморбидностью (АГ, индекс массы тела/ожирение, дислипидемия, ишемическая болезнь сердца (ИБС)). При сборе жалоб и исследовании анамнеза в когорте пациентов в возрасте старше 60 лет необходимо также помнить о высокой частоте выявления амилоидоза сердца у лиц с необъяснимой ГЛЖ и сердечной недостаточностью с сохраненной ФВ, которая варьирует от 6% до 16% [154][196].
2.2. Физикальное обследование
- У всех пациентов рекомендуется стандартное физикальное обследование сердечно-сосудистой системы, включающее аускультацию сердца (аускультация терапевтическая), измерение АД на периферических артериях, при необходимости — повторное, а также лежа, сидя, стоя, исследование пульса, измерение частоты сердцебиения, при ФП — дефицит пульса [1][3][197-200].
ЕОК/РКО IC (УДД 5, УУР С)
Комментарии. Основной диагностический признак ОГКМП — грубый систолический шум выброса, который выявляют над всей поверхность сердца, с максимумом на верхушке и в четвертом межреберье слева от грудины. Систолический шум — низкочастотный, носит характер крещендо-декрещендо, выслушивается вдоль левого края грудины и усиливается под воздействием факторов, увеличивающих внутрижелудочковый ГД: переход в вертикальное положение, динамическая ФН, тахикардия, прием пищи, проба Вальсальвы, прием периферических вазодилататоров.
Большинство пациентов с обструкцией ВТЛЖ также имеют аускультативные признаки МР. Со стороны других систем и органов при ГКМП обычно клинически значимых отклонений нет [3][20][201][202].
У пациентов с обструкцией ВТЛЖ часто выявляется неустойчивость артериального пульса (значительные колебания ЧСС в ортостазе и клиностазе, во время бодрствования и сна). Это может также быть обусловлено автономной (вегетативной) дисфункцией (см. Раздел "Патогенез").
- При физикальном обследовании пациента рекомендуется тщательное исследование симптоматики не только со стороны сердечно-сосудистой системы, но и других органов и систем, что может указывать на фенокопии ГКМП [69-70][72][74][75][181][203-210].
ЕОК IB (УДД 4, УУР C)
2.3. Лабораторная диагностика
- У всех пациентов с ГКМП для выявления сопутствующих заболеваний рекомендуется рутинное лабораторное обследование, включающее общий (клинический) анализ крови и общий (клинический) анализ мочи, анализ крови биохимический общетерапевтический (исследование уровня холестерина в крови; исследование уровня триглицеридов в крови; исследование уровня калия в крови; исследование уровня натрия в крови; исследование уровня глюкозы в крови; определение соотношения белковых фракций методом электрофореза; определение активности аланинаминотрансферазы в крови; определение активности аспартатаминотрансферазы в крови; определение активности креатинкиназы в крови; исследование уровня мочевины в крови; исследование уровня креатинина в крови; исследование уровня общего билирубина в крови; исследование уровня мочевой кислоты в крови), расчет скорости клубочковой фильтрации [3][203][211].
ЕОК/РКО IC (УДД 5, УУР С)
Комментарии. Рутинное лабораторное обследование помогает выявить сопутствующие заболевания, которые могут вызвать или усугубить миокардиальную дисфункцию и состояние пациента.
Исследования уровня N-концевого промозгового натрийуретического пептида (NT-proBNP) в крови и уровня тропонинов I, T в крови (высокоспецифичного сердечного тропонина I или T в крови) не входят в рутинное лабораторное обследование, однако их высокие уровни ассоциированы с выраженностью диастолической дисфункции, ГЛЖ, тяжестью функциональных нарушений (ишемии миокарда, прогрессирование ХСН) и неблагоприятным прогнозом [3][59][60][108][186][211].
Высокий уровень NT-proBNP и высокочувствительного сердечного тропонина T ассоциированы с сердечной недостаточностью и другими сердечно-сосудистыми событиями. Несмотря на сопоставимые значения толщины стенок желудочков, значения NT-proBNP в плазме крови в 3-5 раз выше у пациентов с амилоидозом сердца. Диспропорционально высокое увеличение уровня NT-proBNP при амилоидных КМП важно учитывать при проведении дифференциального диагноза внутри ГКМП-фенотипа [212][213].
При подозрении на конкретную фенокопию ГКМП с целью проведения дифференциального диагноза рекомендуется специальное лабораторное обследование [3][74][203][204][209][210].
Для исключения AL-амилоидоза определяют показатели, характеризующие плазмоклеточную дискразию:
a) исследование моноклональности легких цепей иммуноглобулинов в крови методом иммунофиксации; исследование моноклональности легких цепей иммуноглобулинов в моче методом иммунофиксации;
b) повышение концентрации одной из свободных легких цепей иммуноглобулинов (вовлеченная цепь) в сыворотке крови и/или моче (нефелометрический метод, FreeliteTM, Birmingham, UK) с нарушением их нормального соотношения κ/λ;
c) увеличение количества плазматических клеток в миелограмме (обычно от 5 до 10% по данным цитологического исследования мазка костного мозга (миелограмма)).
Амилоидная AТТР-КМП является необратимо прогрессирующим заболеванием с высокой степенью инвалидизации вследствие тяжелого поражения сердца, периферической и/или автономной полиневропатии. Смертность пациентов с амилоидной АТТР-КМП обычно является результатом прогрессирующей сердечной недостаточности. После постановки диагноза амилоидной AТТР-КМП медиана выживаемости у пациентов, не получавших лечения, составляет ~2-3,5 года.
AТТР-КМП часто не диагностируется из-за того, что оно напоминает другие причины ГЛЖ, в первую очередь ГКМП. У пациентов с AТТР-КМП (наследственной и приобретенной) могут присутствовать как кардиальные, так и некардиальные проявления и признаки, которые, особенно в совокупности, могут указывать на наличие этого заболевания [214]. Среди них: ХСН с сохранённой ФВ, непереносимость стандартных препаратов для лечения ХСН, низкий вольтаж относительно массы ЛЖ. К некардиальным симптомам заболевания относят синдром запястного канала, стеноз поясничного отдела позвоночного канала, нарушения работы желудочно-кишечного тракта и дисфункция периферической и вегетативной нервной системы.
Для ATTR-КМП независимо от других проявлений разработана этиопатогенетическая терапия (Тафамидис 61 мг (Виндамэкс) биоэквивалентен, но не взаимозаменяем в пересчете на мг тафамидису меглюмину в дозе 80 мг).
Данные национального регистра Франции показали, что 8% пациентов, направленных по поводу ГКМП, имеют патогенную мутацию в гене транстиретина [215]. Maurizi N, et al. обнаружили, что распространенность кардиального амилоидоза среди пациентов с первоначальным диагнозом ГКМП составляет 9%, и она увеличивается с возрастом: с 1% в возрасте 40-49 лет до 26% у пациентов в возрасте >80 лет [216].
ГКМП — это диагноз исключения: фенокопии, вторичные и специфические причины ГЛЖ и гипертрофии ПЖ должны быть исключены.
В ряде случаев специальное лабораторное обследование требуется при возникновении осложнений, индуцированных лекарственной терапией, например, при амиодарон-индуцированном гипотиреозе, амиодарон-индуцированном тиреотоксикозе 1 типа, амиодарон-индуцированном тиреотоксикозе 2 типа, смешанной форме амиодарон-индуцированного тиреотоксикоза — определение содержания антител к гормонам щитовидной железы в крови; исследование уровня общего трийодтиронина в крови; исследование уровня общего тироксина сыворотки крови; исследование уровня тиреотропного гормона в крови. Подробное описание представлено в Разделе 3.1.8.1.
Некоторые показатели, позволяющие предположить конкретный диагноз фенокопии ГКМП, приведены в таблице 5, Приложение А3 и в таблице 6, Приложение А3.
Медико-генетическое консультирование и генетическое обследование
- Медико-генетическое консультирование рекомендуется проводить врачам-генетиками или врачам кардиологами с опытом ведения данной группы пациентов3. Целесообразно участие врача-генетика в работе мультидисциплинарной команды специалистов, занимающихся диагностикой и лечением ГКМП [3][20][217].
ЕОК IC (УДД 5, УУР С)
Комментарии. Медико-генетическое консультирование рекомендовано пациентам с ГКМП и их родственникам, и должно включать в себя обсуждение пользы, рисков и ограничений генетического тестирования. Стратегия лечения должна базироваться как на данных генетического тестирования, так и опираться на результаты всестороннего клинического, инструментального и лабораторного обследования [25].
- Перед проведением генетического тестирования рекомендуется рассмотреть возможность проведения претестового медико-генетического консультирования, а после получения результатов генетического тестирования для корректной интерпретации результатов рекомендуется проводить медико-генетическое консультирование в центрах, специализирующихся на генетическом обследовании и динамическом наблюдении семей с генетически-обусловленными заболеваниями сердца [1][41][218-220].
ЕОК IIаС (УДД 5, УУР С)
Комментарии. В ходе медико-генетического консультирования все пациенты должны быть полноценно осведомлены о смысле и значимости генетического тестирования, его возможных результатах, их клинической значимости, а также в целом о вопросах этиопатогенеза и наследования генетически-обусловленных сердечно-сосудистых заболеваний.
Рекомендации по генетическому тестированию пробандов
- Генетическое тестирование пациентам с подозрением на генетически-обусловленное заболевание сердечно-сосудистой системы рекомендуется выполнять только в сочетании с надлежащим медико-генетическим консультированием [220].
ЕОК IIаС (УДД 5, УУР С)
- Генетическое тестирование при ГКМП рекомендуется выполнять в сертифицированных диагностических лабораториях с экспертными навыками в оценке патогенности генетических вариантов, ассоциированных с первичными КМП, согласно современным рекомендациям [1][3][218-220].
ЕОК IB (УДД 5, УУР C)
- В перечень генов при генетическом тестировании пробандов с ГКМП (включая случаи посмертной ДНК-диагностики) рекомендуется включать гены с уверенно доказанной причинной ролью в отношении ГКМП. В настоящее время это гены MYH7, MYBPC3, TNNI3, TNNT2, TPM1, MYL2, MYL3 и ACTC1 [1][3][57][219].
ЕОК IB (УДД 5, УУР С)
- У пациентов с ГКМП (включая случаи посмертной ДНК-диагностики) при типичной, атипичной клинической картине ГКМП или при подозрении на четко очерченный генетический синдром с ГЛЖ генетическое тестирование с целью уточняющей диагностики рекомендуется проводить с использованием более широкого спектра исследуемых генов (ACTC1, ACTN2, ALPK3, ANKRD1, CSRP3, FHL1, FLNC, GLA, JPH2, LAMP2, MYBPC3, MYH6, MYH7, MYL2, MYL3, MYPN, NEXN, PLN, PRKAG2, PTPN11, RAF1, RIT1, SOS1, TCAP, TNNC1, TNNI3, TNNT2, TPM1, TTR и VCL) [1][3][57][218-220].
ЕОК IB (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность выполнения посмертного генетического исследования образцов законсервированных тканей или ДНК для умерших пациентов с патоморфологически подтверждённой ГКМП, чтобы иметь возможность выполнить каскадный генетический скрининг родственников [3][20][33][181][191].
ЕОК IIаС (УДД 5, УУР С)
Комментарии. Проведение генетического тестирования при ГКМП может носить диагностический и предиктивный характер.
В первом случае генетическая диагностика является частью инструментов диагностического поиска и призвана помочь в подтверждении диагноза ГКМП при наличии стёртой или неполной клинической картины, а также при наличии экстракардиальных проявлений заболевания для исключения специфических причин ГКМП-фенотипа (фенокопий у взрослых и синдромных форм у детей) [3][19][20][27][221][222].
Оценка патогенности каждого найденного в результате тестирования генетического варианта должна проводиться в соответствии с рекомендациями Американской коллегии медицинской генетики (American College of Medical Genetics and Genomics — ACMG) от 2015г, рекомендациями РОМГ (2019), а также рядом их модификаций и дополнений, разработанных для отдельно взятых генов [217][223].
При ГКМП, в дополнение к вышеперечисленным источникам, обязательным документом для интерпретации результатов генетического исследования является руководство по оценке вариантов в гене MYH7 [21].
Рекомендации по генетическому и клиническому тестированию родственников
- Для пробандов с ГКМП, у которых были выявлены варианты с неустановленным клиническим значением (VUS, III класс патогенности), рекомендуется рассмотреть возможность выполнения генетического тестирования больных родственников с ГКМП (сегрегационный анализ) для уточнения класса патогенности варианта [3][20][219][220].
ЕОК IIbС (УДД 5, УУР C)
- В случае, если у пробанда с ГКМП выявлены причинные генетические варианты IV-V класса патогенности (патогенные и вероятно-патогенные), его взрослым родственникам рекомендуется рассмотреть возможность проведения генетического тестирования (каскадного семейного скрининга) для выявления/исключения носительства тех же генетических вариантов, которые были выявлены у пробанда [3][20][21][219][220][224].
ЕОК IIbС (УДД 5, УУР С)
- В случае, если у пробанда с ГКМП выявлены причинные генетические варианты IV-V класса патогенности (патогенные и вероятно-патогенные), его несовершеннолетним родственникам рекомендуется генетическое тестирование (каскадный семейный скрининг) для выявления/исключения носительства тех же генетических вариантов, которые были выявлены у пробанда, начиная с возраста 10-12 лет, если семейный анамнез не требует иного [1][3][218-220].
ЕОК IIаС (УДД 5, УУР С)
- Клиническое обследование, включающее ЭКГ, ЭхоКГ и длительное динамическое наблюдение, рекомендуется родственникам первой степени родства, у которых выявлен тот же причинный генетический вариант (варианты) IV-V класса патогенности (патогенный и вероятно-патогенный), что и у пробанда [1][3][218-220, 225].
ЕОК IB (УДД 5, УУР С)
- Родственников первой степени родства, у которых не обнаружен тот же причинный генетический вариант (варианты) IV-V класса патогенности (патогенный и вероятно-патогенный), что и у пробанда, рекомендуется вывести из дальнейшего динамического наблюдения, но с рекомендацией обратиться за повторным обследованием, если у них разовьются симптомы ГКМП или появятся новые, имеющие отношение к ГКМП клинические данные [1][3][218-220].
ЕОК IС (УДД 5, УУР C)
- Если генетический скрининг пробанду с ГКМП не проводился, клиническое обследование с ЭКГ и ЭхоКГ рекомендуется для родственников первой степени родства каждые 2-5 лет (или 6-12 мес., если имеются диагностически незначимые аномалии) [1][3][218-220][225].
ЕОК IIаB (УДД 5, УУР С)
Комментарии. Предиктивный генетический скрининг основан на использовании информации о конкретной генетической причине заболевания, идентифицированной у генотип-позитивного пробанда, для определения носительства патогенного/вероятно патогенного варианта у его родственников. Целью данного скрининга является определение необходимости регулярной диспансеризации и прицельного клинического наблюдения при наличии патогенного варианта, а также исключение необходимости такого скрининга при отсутствии носительства этого варианта.
При проведении каскадного скрининга членов семьи пробанда рекомендуется сочетать его с клиническим обследованием сердечно-сосудистой системы (анамнестические данные, объективный осмотр, ЭКГ и ЭхоКГ) (см. таблицу 7, Приложение А3).
- В семьях пробандов с ГКМП, у которых не было выявлено патогенных/вероятно патогенных вариантов (IV-V класса) в генах, ответственных за ГКМП (генотип-негативные), каскадный семейный скрининг с диагностическими целями выполнять не рекомендуется [1][3][218-220].
ЕОК IIIС (УДД 5, УУР С)
- Регулярное динамическое наблюдение и клинический скрининг не рекомендуются генотип-негативным родственникам генотип-позитивных пробандов с ГКМП [1][3][218-220].
ЕОК IIIС (УДД 5, УУР С)
2.4. Инструментальные диагностические исследования
Электрокардиография и мониторирование ЭКГ
Изменения при стандартной ЭКГ могут наблюдаться уже у носителей ГКМП-ассоциированных мутаций (генотип-позитивных/ГЛЖ-негативных), т.е. на догипертрофической стадии ГКМП. К таким признакам относятся RV1<RV2>RV3, изменения реполяризации, регистрация патологического Q-зубца (у детей). Однако при сопоставлении со здоровыми лицами эти изменения, обладая высокой специфичностью (98%), показали низкую чувствительность (25%) [226][227].
У пациентов с "классическим фенотипом" ГКМП в 75-95% случаев ЭКГ в 12 отведениях является аномальной, включая признаки ГЛЖ, регистрацию патологического Q-зубца и изменения реполяризации [180][228][229].
У некоторых пациентов (~5% взрослых и до 3% детей) ЭКГ может быть нормальной. В этой группе клиническое течение заболевания было более благоприятным по сравнению с пациентами, у которых имелись аномалии на ЭКГ [230].
Выделяют несколько паттернов, характерных для "классического фенотипа" ГКМП:
- Патологические Q-зубцы в нижне-боковых отведениях (при этом в отведениях с патологическими Q регистрируются положительные Т — так называемая Q/T-дискордантность) + изменения реполяризации + ГЛЖ (критерии Romhilt-Estes);
- Гигантские симметричные (-)Т-зубцы — при верхушечной ГКМП (транзиторное углубление отрицательных Т может свидетельствовать об ишемии, требующей реваскуляризации) [231];
- "Псевдо-STEMI" паттерн (подъем сегмента ST и/или высокие (+)Т в 2-х и более последовательных отведениях при отсутствии блокады левой ножки пучка Гиса) [180];
- Депрессия сегмента ST;
- Неспецифические изменения сегмента ST и зубца Т на ЭКГ [232][233].
Фрагментация комплекса QRS (fQRS) у пациентов с ГКМП может свидетельствовать о наличии очагов фиброза в миокарде. Кроме того, fQRS может служить хорошим маркером-кандидатом для прогнозирования желудочковых нарушений ритма (ЖНР) у пациентов с ГКМП [234][235].
- Регистрация электрокардиограммы рекомендуется всем пациентам при первичном обследовании с подозрением на ГКМП, после постановки диагноза в процессе подбора фармакотерапии, после хирургических и эндоваскулярных вмешательств и при динамическом наблюдении каждые 12-24 мес. [3][180][219][203][230][236-239].
ЕОК IB (УДД 3, УУР B)
- Всем пациентам с ГКМП при ухудшении симптоматики, при подборе фармакотерапии, после хирургических и эндоваскулярных вмешательств, при динамическом наблюдении рекомендуется повторная регистрация ЭКГ с целью выявления нарушений сердечного ритма и проводимости, ишемии миокарда [3][199][203][230][236-238].
ЕОК IB (УДД 3, УУР B)
- Всем пациентам с ГКМП независимо от симптоматики рекомендуется повторная регистрация ЭКГ каждые 1-2 года с целью выявления нарушений сердечного ритма и проводимости, ишемии миокарда [3][199][203][230][236-238].
ЕОК/РКО IIaB (УДД 3, УУР B)
- Регистрация ЭКГ рекомендуется как компонент скрининг-алгоритма у родственников первой степени родства пациентов с ГКМП [3][199][203][230][236-238].
ЕОК IC (УДД 5, УУР С)
Холтеровское мониторирование (ХМ) сердечного ритма при ГКМП
Эпизоды неустойчивой ЖТ входят в шкалу риска ВСС. Существует все больше доказательств того, что такие аритмии у молодых пациентов с ГКМП являются более ценным прогностическим признаком ВСС, чем у пациентов старше 35 лет.
Если у пациента присутствуют симптомы, ХМ сердечного ритма должно продолжаться до тех пор, пока эти симптомы не проявятся во время ношения монитора. У некоторых пациентов с редкими симптомами может потребоваться использование портативных или имплантируемых мониторов. Поэтому пациентам с ГКМП, у которых возникает учащенное сердцебиение или головокружение, рекомендуется проводить длительное (>48 ч) ХМ сердечного ритма.
- ХМ сердечного ритма рекомендуется всем пациентам с ГКМП, в т.ч. асимптомным, с целью выявления нарушений ритма сердца (ФП и ЖТ) и проводимости для стратификации риска ВСС и отбора кандидатов для имплантации ИКД*** [3][127][128][200][203][240-242].
ЕОК нет/РКО IC (УДД 3, УУР B)
- Проведение ХМ сердечного ритма (оптимально продолжительностью 48-72 ч) рекомендуется при первичном клиническом обследовании, при подборе антиаритмической терапии, после хирургических и эндоваскулярных вмешательств и при динамическом наблюдении каждые 12-24 мес. [3][200][203][236][240][243].
ЕОК IIаС (УДД 2, УУР С)
Комментарии. ФП является наиболее распространенным нарушением ритма у пациентов с ГКМП и основным предиктором смертности, связанной с сердечной недостаточностью. Ее частота встречаемости в ГКМП значительно выше, чем у людей аналогичного возраста в общей популяции, составляя от 18% до 28%. Однако истинную частоту встречаемости сложно оценить из-за случаев, когда ФП может оставаться незамеченной. Выявление клинически непроявленной ФП, которая обнаруживается только при длительном ХМ сердечного ритма, имеет важное значение для оценки стратегии лечения и профилактики инсульта, поскольку риск ишемического инсульта у пациентов с ГКМП и ФП выше в 8 раз по сравнению с пациентами на синусовом ритме [1].
- Рекомендуется имплантация петлевого регистратора для долговременной регистрации электрической активности проводящей системы сердца с целью выявления нарушений сердечного ритма у пациентов с жалобами на частые сердцебиения, у которых при длительном мониторировании ЭКГ причина осталась неуточненной [3][137][203][244-247].
ЕОК IIаС (УДД 3, УУР B)
- Пациентам с ГКМП и дополнительными факторами риска ФП (дилатация ЛП, старческий возраст, ХСН III-IV ФК), которые не имеют противопоказаний к назначению антикоагулянтов, рекомендуется рассмотреть возможность выполнения расширенного амбулаторного мониторирования ЭКГ с целью выявления асимптомных пароксизмов ФП при первичном обследовании, в процессе подбора фармакотерапии и при динамическом наблюдении (каждые 12-24 мес.) [203].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
Комментарии. Адекватная оценка нарушений ритма и проводимости критически необходима для стратификации риска ВСС, поэтому в некоторых случаях необходим длительный ЭКГ-мониторинг. Кроме рутинного суточного мониторирования ЭКГ, возможны варианты: 48/72-часовой мониторинг, наружный петлевой регистратор, регистратор событий, имплантируемый петлевой регистратор. ЭКГ-диагностика должна повторяться каждые 12-24 мес., оптимально продолжительностью 48 ч.
Показанием к ХМ сердечного ритма является появление у пациента жалоб на сердцебиение и/или головокружение.
Необходимо учитывать, что нарушения ритма и проводимости могут быть обусловлены проводимой терапией.
ЭКГ-признаки, помогающие в дифференциальной диагностике ГКМП и фенокопий ГКМП, представлены в таблице 8, Приложение А3.
ЭхоКГ
ЭхоКГ-исследование пациентам необходимо выполнять в соответствии с отечественными и зарубежными рекомендациями по эхокардиографии AHA, ASE (American Society of Echocardiography) и EACI (European Association of Cardiovascular Imaging) [1][192][205][248-255].
- Всем пациентам с подозрением на ГКМП для выявления ГЛЖ и внутрижелудочковой обструкции при первичном обследовании рекомендуется трансторакальная ЭхоКГ (ТТ-ЭхоКГ) с провокационной пробой Вальсальвы [178][203][256-261].
ЕОК IB (УДД 4, УУР С)
- Всем пациентам с ГКМП измерение максимальной диастолической толщины миокарда ЛЖ рекомендуется проводить в 2D-режиме по короткой оси ЛЖ во всех сегментах, от базальных до верхушки [110][251][252][256][262-264].
ЕОК IC (УДД 4, УУР С)
- Всем пациентам с ГКМП рекомендуется тщательная оценка диастолической функции ЛЖ, включая трансмитральный кровоток, кровоток в легочных венах, тканевую допплерографию, измерение размера и объема ЛП для стратификации риска ВСС [108][122][178][203][265-269].
ЕОК IC (УДД 4, УУР С)
- Симптомным пациентам с максимальным ГД в ВТЛЖ (в покое или спровоцированным) <50 мм рт.ст. рекомендуется проведение стресс-ТТ-ЭхоКГ для выявления провоцируемой обструкции ВТЛЖ и стресс-индуцируемой МР [84][123][130][178][203][259][260][270-274].
ЕОК IB (УДД 4, УУР С)
- Асимптомным пациентам с максимальным ГД в ВТЛЖ (покоя или индуцированным) <50 мм рт.ст. рекомендуется рассмотреть возможность выполнения стресс-ТТ-ЭхоКГ, если наличие обструкции имеет значение для рекомендаций по образу жизни и назначения лекарственной терапии [84][203][259][270][271].
ЕОК IIbС (УДД 4, УУР С)
- У больных с субоптимальным качеством изображения или с предполагаемой апикальной ГЛЖ или апикальной аневризмой ЛЖ, или атипичным паттерном гипертрофии, рекомендуется выполнение ЭхоКГ с контрастированием полости ЛЖ как альтернатива МРТ сердца [1][255].
ЕОК IIаС (УДД 5, УУР С)
- Интракоронарное контрастирование миокарда при ТТ-ЭхоКГ во время диагностической КАГ рекомендуется пациентам, у которых планируется ЭСА, для идентификации подходящей для аблации септальной ветви коронарной артерии [255][275-278].
ЕОК IB (УДД 4, УУР С)
- Повторные ЭхоКГ-исследования рекомендуются больным ГКМП при изменении клинического статуса, при появлении новой сердечно-сосудистой симптоматики, оценки эффективности проводимой терапии или хирургического/эндоваскулярного лечения для своевременного выявления осложнений и динамики ремоделирования сердца [84][259][260][279].
ЕОК IB (УДД 4, УУР С)
- ЭхоКГ рекомендуется как компонент скрининг-алгоритма членов семьи больного ГКМП, если хотя бы один из них не является генотип-отрицательным и выявлена ассоциированная с заболеванием генная мутация [181][224].
ЕОК IC (УДД 5, УУР C)
Комментарии. Требуется использовать расширенный протокол ЭхоКГ, адаптированный к диагностике ГКМП. Перечень показателей, входящих в протокол ТТ-ЭхоКГ, представлен в таблице 9, Приложение А3.
Заболевания (кроме ОГКМП), при которых может регистрироваться повышение ГД в ВТЛЖ и SAM-синдром (ПСД МК), представлены в таблице 10, Приложение А3.
Для дифференциальной диагностики с фенокопиями и при выборе хирургической тактики при ГКМП могут использоваться дополнительные опции при ЭхоКГ, представлены в таблице 11, Приложение А3.
ЭхоКГ-находки, позволяющие дифференцировать ГКМП и фенокопии ГКМП, представлены в таблице 2, Приложение А3 и таблице 12, Приложение А3.
Рекомендации по чреспищеводной ЭхоКГ при ГКМП
- Интра/периоперационная чреспищеводная ЭхоКГ (ЧП-ЭхоКГ) при СМЭ рекомендуется пациентам для уточнения механизма обструкции ВТЛЖ, контроля хирургической стратегии, оценки постхирургических осложнений и выявления остаточной обструкции ВТЛЖ [253][275][276][280-283].
ЕОК IС (УДД 4, УУР С)
- Рекомендовано выполнение ЧП-ЭхоКГ как альтернативы МРТ для пациентов с ГКМП при выборе вида оперативного вмешательства СМЭ или ЭСА, у которых не ясен механизм обструкции ВТЛЖ или для оценки состояния МК или если регистрируется выраженная МР, предположительно не связанная с SAM-синдромом (ПСД створок), а обусловленная собственными аномалиями МК [1][203][253][275][276][280-283].
ЕОК IIaС (УДД 4, УУР С)
- Пациентам с ГКМП при выполнении ЭСА для корректного определения целевой зоны воздействия рекомендуется интраоперационное ЧП-ЭхоКГ с интракоронарным контрастированием миокарда [255][275-278].
ЕОК IIaC (УДД 4, УУР С)
Проведение провокационной пробы Вальсальвы для диагностики латентной обструкции ВТЛЖ
Пробу Вальсальвы при ТТ-ЭхоКГ следует проводить в положении пациента лежа на левом боку. Пациенту следует напрячь мышцы передней брюшной стенки, что повышает внутрибрюшное и внутригрудное давление. Контроль уровня напряжения целесообразно осуществлять с помощью устройства, представляющего манометр, соединенный с мундштуком; при этом пациента просят удерживать напряжение, чтобы давление на манометре составляло 20-40 мм рт.ст. Во время пробы Вальсальвы регистрируется максимальная скорость кровотока в ВТЛЖ с использованием постоянно-волнового допплера. Если в положении пациента лежа проба отрицательная, то рекомендуется провести пробу в положении сидя и стоя.
МРТ
- МРТ сердца с контрастированием (при отсутствии противопоказаний) рекомендуется выполнить как минимум один раз после постановки диагноза ГКМП для уточнения данных ЭхоКГ (анатомии сердца, функции желудочков), а также выявления и оценки распространенности фиброза миокарда и исключения фенокопий ГКМП и других заболеваний [284][285].
ЕОК IB (УДД 4, УУР С)
Комментарии. Необходимость выполнения МРТ вызвана тем, что ТТ-ЭхоКГ может некорректно оценивать толщину миокарда в некоторых сегментах ЛЖ, особенно в апикальных, не выявлять апикальные аневризмы небольших размеров.
- МРТ сердца с контрастированием (при отсутствии противопоказаний) рекомендуется выполнить пациентам, которым показана редукция МЖП, и у которых ТТ-ЭхоКГ не позволяет определить анатомический механизм обструкции ВТЛЖ, для обоснования выбора метода редукции МЖП [1][286].
ЕОК нет/РКО IC (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность выполнения МРТ сердца с контрастированием (при отсутствии противопоказаний) при подозрении на апикальную или среднежелудочковую форму ГКМП и апикальную аневризму ЛЖ [203].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность выполнения МРТ сердца с контрастированием для пациентов с ГКМП при изменении клинического или гемодинамического статуса, с целью оценки динамики морфо-функциональных изменений ЛЖ (ФВ ЛЖ, максимальная толщина миокарда, развитие апикальной аневризмы) [1].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность выполнения МРТ сердца с контрастированием родственникам пробанда первой линии родства, если постановка диагноза значимо влияет на образ жизни (например, запрещение соревновательного спорта), а при ЭхоКГ имеется низкое качество изображения, или данные пограничные/сомнительные, или есть изменения на ЭКГ, а ЭхоКГ без отклонений от нормы [220][275].
ЕОК нет/РКО IIbC (УДД 5, УУР C)
- Пациентам c предполагаемыми фенокопиями ГКМП (амилоидоз сердца и другие, см. Приложение АЗ, таблицы 1/А3, 5/А3, 7/А3, 11/А3) рекомендуется выполнение МРТ сердца с контрастированием с целью выявления специфических для конкретных фенокопий паттернов [71][75][206][287-291].
ЕОК IIаС (УДД 4, УУР С)
Комментарии. Пациентам с предполагаемым амилоидозом сердца рекомендовано для первоначальной дифференциальной диагностики TTR-амилоидоза и AL-амилоидоза при контрастной МРТ использовать шкалу QALE [292]. Шкала QALE приведена в Приложении Г6 (QALE. Шкала для дифференциальной диагностики ATTR с помощью контрастной МРТ сердца).
- Рекомендуется выполнение МРТ сердца с контрастированием до операции хирургической и нехирургической редукции МЖП для оценки характера и распространенности гипертрофии и фиброза миокарда [70][74][206][287-291].
ЕОК IIаС (УДД 4, УУР С)
- Анализ изображений МРТ сердца и сосудов рекомендуется выполнять специалистам, имеющим опыт в визуализации сердца и оценке заболеваний миокарда2 [3][293-295].
ЕОК IС (УДД 4, УУР С)
- Рекомендуется рассмотреть возможность выполнения МРТ сердца с контрастированием для пациентов с подозрением на ГКМП и сомнительными результатами ТТ-ЭхоКГ с пограничными цифрами толщины миокарда [203].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
Комментарии. МРТ не имеет присущих ЭхоКГ ограничений и является "золотым стандартом" оценки толщины миокарда и объемов ЛЖ и ПЖ (больше точность измерений и воспроизводимость, меньше операторозависимость), поэтому при отсутствии противопоказаний, если позволяют ресурсы и опыт, МРТ должна рассматриваться для пациентов с ГКМП в качестве базового метода исследования [275][294-297].
МРТ также позволяет исследовать структурные изменения в миокарде, т.е. генез, наличие и распространенность миокардиального фиброза. Методика основана на том, что в участках миокарда с фиброзными изменениями выявляется феномен позднего накопления парамагнитного контрастного вещества — задержка вымывания Gd-содержащего контрастного вещества при сканировании сердца через 10-15 мин после его внутривенного введения. Наличие распространенного фиброза является предиктором негативного ремоделирования, развития систолической дисфункции и ХСН, а также относится к дополнительным факторам риска ВСС. При наличии фиброзных изменений в миокарде ЛЖ в количестве ≥15% массы ЛЖ риск ВСС значительно возрастает.
При МРТ выявляются 2 основных паттерна фиброза:
- Выраженно неоднородный интрамуральный фиброз в пределах наиболее утолщенных сегментов, который на гистологическом уровне является отражением прямого действия "причинного" генетического варианта и молекулярного патогенеза, проявляющегося дискомплексацией кардиомиоцитов и мышечных волокон — феномен "disarray", фиброзом разной степени выраженности.
- Зоны фиброза могут быть выявлены в МЖП в передней и/или задней областях, в местах соединения стенок ПЖ и ЛЖ (т.н. "right ventricular insertion points"). Считается, что этот тип фиброза может наблюдаться уже на начальных стадиях заболевания и часто встречается при ГКМП, однако не является абсолютно специфичным для этого заболевания. Такой тип контрастирования может также встречаться при "спортивном сердце" или кардиопатии, вызванной аритмией. Считается, что это интерстициальный фиброз или промежуточный фенотип ПНГ, начальная стадия [112][275][298].
Параметры, которые необходимо оценить при МРТ сердца у пациента с ГКМП, представлены в таблице 13, Приложение А3.
У носителей мутаций в догипертрофической стадии ГКМП при МРТ можно выявить "малые аномалии сердца" — крипты миокарда, аномалии МК, апикальное смещение папиллярных мышц. На доклинической стадии у некоторых пациентов с генотипом(+)/фенотипом(-) могут быть выявлены зоны ПНГ (см. алгоритм диагностики на доклинической стадии) [296][299][300].
При МРТ сердца также выявляются аномалии аппарата МК (см. таблицу 13, Приложение А3).
Кроме значимости в диагностике ГКМП, МРТ сердца играет роль в диагностике фенокопий ГКМП. При амилоидозе зоны ПНГ определяются преимущественно в интрамуральных и субэндокардиальных отделах желудочков. Это накопление не зависит от зон кровоснабжения миокарда, может наблюдаться во всех структурах сердца. Для амилоидоза сердца также характерно наличие жидкости в полости перикарда и утолщение МЖП [290][291].
При болезни Андерсона-Фабри — наличие интрамиокардиального ПНГ чаще всего по заднебоковому сегменту на базальном и среднем уровнях [301]. У спортсменов с ГЛЖ отсутствуют зоны ПНГ (исключения — см. Раздел "ГКМП и ГЛЖ у спортсменов") [302].
КТ/мультиспиральная КТ
- Пациентам с ГКМП, у которых низкое качество ЭхоКГ изображения, а проведение МРТ противопоказано, для оценки толщины миокарда и размеров полостей сердца рекомендуется выполнение ЭКГ-синхронизированной КТ/мультиспиральной КТ (МСКТ) сердца с контрастированием сердца и оценкой толщины миокарда ЛЖ в конечную диастолу [1][203][275][303].
ЕОК IIаС (УДД 5, УУР С)
Комментарии. Измерение толщины миокарда при КТ/МСКТ сердца следует проводить в конечную диастолу.
КТ сердца, кроме анатомических данных сердца, позволяет также визуализировать коронарные артерии, оценивать их проходимость и анатомические особенности, наличие миокардиальных "мышечных мостиков", что играет важную роль в диагностике ИБС, в т.ч. при ГКМП у пациентов старшей возрастной группы. При КТ/МСКТ сердца также выявляются дивертикулы и крипты стенок ЛЖ — признаков ГКМП на ранней стадии развития заболевания.
МСКТ сердца, имеющая высокое пространственное разрешение, позволяет обеспечить точное измерение толщины, массы миокарда, объема желудочков и ФВ. Сравнительное исследование показало высокую точность метода МСКТ, сопоставимую с результатами метода МРТ сердца [304][305].
По сравнению с МРТ, минусом МСКТ является более низкое временное разрешение, лучевая нагрузка на пациента при исследовании, низкая контрастность мягких тканей при оценке позднего контрастирования, что позволяет оценить только крупные зоны фиброза [305].
Сцинтиграфия
- Рекомендуется выполнение сцинтиграфии миокарда с Пирфотех 99 Тс (V09BA03 Технеций 99m-пирофосфат) пациентам с ГКМП, у которых подозревается кардиальный ATTR [181][203][206][288][306][307].
ЕОК IIаВ (УДД 3, УУР B)
Комментарии. Сцинтиграфия миокарда (однофотонная эмиссионная КТ) также может использоваться для инструментальной диагностики ишемии, подтверждения значимости стеноза эпикардиальных коронарных артерий при пограничных значениях степени стеноза при КАГ.
При подозрении на амилоидоз сердца, следующим шагом является дифференциальный диагноз амилоидных ТТР-КМП и поражения сердца при AL-амилоидозе. Исторически золотым стандартом диагностики была эндомиокардиальная биопсия. В настоящее время также доступен неинвазивный подход с помощью сцинтиграфии миокарда с остеотропным радиофармпрепаратом. Этот подход, впервые описанный Gilmore в 2016г, включен в Рекомендации экспертов на основе консенсуса 2019г [308][309].
Сцинтиграфию миокарда с остеотропным радиофармпрепаратом можно проводить с любым из 3 различных фосфонатов, однако в Российской Федерации широко применяется только 99mTc-пирофосфат (пирофосфат технеция). Американское общество ядерной кардиологии (ASNC) недавно выпустило практические рекомендации по визуализации 99m-технеций-пирофосфата, отметив высокую чувствительность и специфичность в выявлении амилоидных ТТР-KMП и возможность дифференцировать ее от других типов амилоидоза сердца без необходимости биопсии.
Существует два подхода к количественному анализу накопления радиофармпрепарата в миокарде: полуколичественный и количественный. Полуколичественный подход включает визуальное сравнение с накоплением в костях (ребрах) через 3 ч:
Степень 0 — нет накопления в сердце и нормальное накопление в костях (ребрах);
Степень 1 — есть накопление в сердце, но меньше, чем накопление в ребрах;
Степень 2 — накопление в сердце равно накоплению в ребрах;
Степень 3 — накопление в сердце больше, чем накопление в ребрах с умеренным или отсутствующим накоплением в ребрах.
При подозрении на амилоидоз сердца степень накопления в миокарде 2 или 3 (плоскостная сцинтиграфия и однофотонная эмиссионная КТ), в сочетании с анализами для исключения AL-амилоидоза, подтверждает диагноз ATTR-КМП.
Важно отметить, что при наличии какого-либо планарного накопления следует выполнить однофотонную эмиссионную томографию, чтобы убедиться, что наблюдаемое накопление находится в миокарде, а не в кровяном депо или прилегающих костных структурах.
Альтернативно, количественный подход включает исследуемую область, расположенную над миокардом, и исследуемую область аналогичного размера, расположенную над контрлатеральным легким. Соотношение накопления в исследуемой области сердца к контрлатеральному легкому может определять наличие ATTR-КМП:
- Соотношение >1,5 указывает на ATTR-КМП;
- Соотношение от 1,0 до 1,5 является неопределённым;
- Соотношение <1 не указывает на ATTR-КМП.
Независимо от результатов ядерной сцинтиграфии, это исследование всегда следует сочетать с исследованием на наличие AL-амилоидоза.
Также по данным сцинтиграфии с 99mTc-пирофосфатом возможна точная дифференциальная диагностика AL- и ATTR-амилоидоза сердца (при условии исключения моноклональной гаммапатии неопределенного значения) [68][288].
Позитронная эмиссионная томография
Позитронная эмиссионная томография миокарда (ПЭТ) может использоваться для инструментальной диагностики ишемии, подтверждения значимости стеноза эпикардиальных коронарных артерий при пограничных значениях степени стеноза при коронарной ангиографии [203].
ПЭТ и МРТ являются предпочтительными методами для исследования перфузии при ФН.
ПЭТ может использоваться для исследования коронарной перфузии и метаболизма миокарда (радиофармпрепараты — флудезоксиглюкоза (18F) (АТХ V09IX04 флудезоксиглюкоза (18F)), натрия ацетат (1-11C), Азот-13 (АТХ V09GX Другие радиофармацевтические средства для диагностики сердечно-сосудистой системы), вода (¹⁵O), рубидия (82Rb) хлорид (АТХ V09GX04)) и диагностики автономной дисфункции сердца.
При ГКМП может выявляться нарушение обратного захвата нейромедиаторов и уменьшение плотности бета-адренорецепторов.
КАГ
КАГ является методом выбора диагностики наличия и выраженности обструктивного поражения эпикардиальных коронарных артерий.
- Взрослым пациентам с ГКМП с предотвращенной ВСС (после успешных реанимационных мероприятий), пациентам с устойчивой ЖТ и пациентам со стабильной стенокардией ≥3 ФК (по классификации Канадского сердечно-сосудистого общества — CCS) рекомендуется выполнение инвазивной КАГ или КТ-ангиографии с целью диагностики обструктивного поражения эпикардиальных коронарных артерий [1][3][90][203][310].
ЕОК IС (УДД 5, УУР С)
- Пациентам с ГКМП с типичными болями в грудной клетке (<3 ФК стенокардии по классификации Канадского сердечно-сосудистого общества — CCS), у которых есть промежуточная предтестовая вероятность атеросклеротической ИБС с учетом возраста, пола и факторов риска атеросклероза рекомендуется выполнение КАГ или КТ-ангиография с целью диагностики обструктивного поражения эпикардиальных коронарных артерий [1][3][90][203][303][311].
ЕОК IIаС (УДД 5, УУР С)
- Всем пациентам с ГКМП старше 40 лет рекомендуется выполнение КАГ или КТ-коронарографии до редукции МЖП, независимо от наличия типичного стенокардитического болевого синдрома с целью диагностики обструктивного поражения эпикардиальных коронарных артерий [3][303][312][313].
ЕОК IIаС (УДД 4, УУР С)
Комментарии. Необходимость КАГ диктуется особенностью врачебной тактики. При INOCA у пациентов с ГКМП появляется необходимость в постановке стентов при меньшей, чем принято у пациентов с ИБС, степени стеноза, т.е. при стенозах <50% (см. Раздел "Диагностика ГКМП у отдельных категорий пациентов" и Раздел "Патогенез") [90][91][98][101][314].
Инвазивное измерение давления в полостях сердца
- Рекомендуется выполнение чрезвенозной катетеризации сердца для оценки функции желудочков и давления заклинивания ЛА у пациентов, которым планируется трансплантация сердца или механическая поддержка кровообращения [315-320].
ЕОК IB (УДД 3, УУР B)
- У симптомных пациентов с неопределенными результатами неинвазивной визуализации сердца рекомендуется рассмотреть возможность выполнения чрезвенозной катетеризации сердца (ЛЖ и ПЖ) для оценки тяжести обструкции ВТЛЖ/ВТПЖ и измерения давления наполнения ЛЖ/ПЖ [85].
ЕОК IIbC (УДД 4, УУР С)
Электрофизиологическое тестирование
- Внутрисердечное электрофизиологическое исследование рекомендуется пациентам с документированными персистирующими или периодическими наджелудочковыми тахикардиями (ТП, предсердная тахикардия, атриовентрикулярная узловая риентри тахикардия, тахикардия, опосредованная добавочными проводящими путями) и пациентам с синдромом раннего возбуждения желудочков, для идентификации субстрата аблации и лечения [137][245][321-324].
ЕОК IС (УДД 4, УУР С)
- Для отдельных пациентов с документированными, симптомными, мономорфными устойчивыми (>30 с) ЖТ рекомендуется рассмотреть возможность выполнения внутрисердечного электрофизиологического исследования для идентификации субстрата аблации и лечения [137][323][325][326].
ЕОК IIbC (УДД 4, УУР С)
Комментарии. Пациентам с ГКМП не рекомендовано внутрисердечное электрофизиологическое исследование с программируемой желудочковой стимуляцией в качестве рутинной процедуры для стратификации риска ВСС [3][126][236][325].
Нагрузочные тесты
- Рекомендуется выполнение ЭКГ с ФН (тредмил-тест с мониторированием ЭКГ и АД) для стратификации риска ВСС пациентов с ГКМП, при недоступности эргоспирометрии [3][225][327][328].
ЕОК IIаВ (УДД 4, УУР С)
- Симптомным пациентам с ГКМП, у которых в покое максимальный ГД в ВТЛЖ <30 мм рт.ст., при пробе Вальсальвы ГД <50 мм рт.ст. рекомендуется проведение ТТ-ЭхоКГ в условиях нагрузки (стресс-ЭхоКГ) для определения и количественной оценки динамической обструкции ВТЛЖ [1][192][271][274][329][330].
ЕОК IВ (УДД 3, УУР B)
- Асимптомным пациентам с ГКМП, у которых в покое максимальный ГД в ВТЛЖ <30 мм рт.ст., при пробе Вальсальвы ГД <50 мм рт.ст. рекомендуется выполнение ТТ-ЭхоКГ в условиях нагрузки (стресс-ЭхоКГ) для определения и количественной оценки динамической обструкции ВТЛЖ [1][192][271][274][329][330].
ЕОК IIaC (УДД 5, УУР C)
- У пациентов с ГКМП, у которых не ясен генез симптомов или снижения толерантности к ФН рекомендуется рассмотреть возможность выполнения стресс-теста с ФН перед редукцией МЖП [1].
ЕОК нет/РКО IIbC (УДД 5, УУР C)
- У пациентов с ГКМП, у которых при динамическом наблюдении неясен генез симптомов или снижения толерантности к ФН, рекомендуется рассмотреть возможность выполнения стресс-теста с ФН [1].
ЕОК нет/РКО IIbC (УДД 5, УУР C)
Комментарии. Варианты нагрузочных тестов представлены в таблице 14, Приложение А3.
Вопросы, на которые должна ответить стресс-ЭхоКГ (должны быть отражены в заключении):
- Величина нарастания ГД в ВТЛЖ на пике нагрузки и в восстановительном периоде;
- Реакция АД на нагрузку;
- Индуцируется ли нагрузкой ишемия миокарда ЛЖ;
- Усугубляется ли диастолическая дисфункция (E/A, E/e’);
- Степень изменения МР на фоне стресс-ЭхоКГ (динамическая МР).
Наиболее подходит для стресс-ЭхоКГ у пациентов с ГКМП "лежачий велоэргометр", который позволяет получать ЭхоКГ-изображения на разных ступенях нагрузочной пробы (рекомендуется регистрация показателей на ступени нагрузки 50 Вт, на пике нагрузки и в восстановительном периоде). Использование тредмила и сидячего велоэргометра не позволяет регистрировать ЭхоКГ-показатели в процессе проведения нагрузки, поэтому регистрация проводится немедленно после ее прекращения и в восстановительном периоде. Показано, что максимальный ГД в ВТЛЖ на пике нагрузки и сразу после ее прекращения почти совпадают [271].
При тредмил-тесте применяют протокол Брюса или модифицированный протокол Брюса. При велоэргометрии ступени теста — 50-100-150 Вт.
У пациентов с ГКМП не рекомендуется проводить стресс-ЭхоКГ с добутамином из-за высокого риска индукции ЖНР. Кроме того, добутамин может спровоцировать увеличение ГД в ВТЛЖ у пациентов без ГКМП.
Во время проведения нагрузочного теста регистрируется ЭКГ (постоянно), АД (каждые 2 мин) и изменения клинической симптоматики.
Реакция АД на нагрузку является важной частью нагрузочного тестирования.
Неадекватной реакцией АД считается:
- Гипотензивная (АД на пике нагрузки ниже исходного или если на первых ступенях нагрузки АД несколько повышается, а на пике нагрузки — более чем на 20 мм рт.ст. ниже этого уровня);
- Недостаточный прирост АД на пике нагрузки (<20 мм рт.ст.).
Критерии прекращения нагрузочного теста:
— Достижение субмаксимальной ЧСС;
— Выраженная усталость и одышка;
— Боли в области сердца;
— Гипотензия (снижение АД >20 мм рт.ст. от исходного);
— Жизнеопасные ЖНР [84][192][270-274][330][331].
Эргоспирометрия
- Пациентам с ГКМП с выраженной симптоматикой с систолической и/или диастолической дисфункцией ЛЖ для определения показаний к трансплантации сердца или механической поддержке кровообращения рекомендуется выполнение эргоспирометрии (кардиопульмональное нагрузочное тестирование с одновременным измерением респираторных газов) [3][315-317][319][320][332-335].
ЕОК IB (УДД 3, УУР В)
- Пациентам с ГКМП, независимо от симптоматики, рекомендуется проведение эргоспирометрии (или стандартный тредмил-тест, или велоэргометрию при его отсутствии) с целью оценки тяжести и механизма непереносимости ФН и изменений систолического АД [3][333][336][337].
ЕОК IIаВ (УДД 4, УУР С)
- Рекомендуется выполнение эргоспирометрии (или стандартный тредмил-тест, или велоэргометрия при его отсутствии) у симптомных пациентов, которым планируется СМЭ для определения ограничений по нагрузке [3][333][336][337].
ЕОК IIаС (УДД 4, УУР С)
2.5. Иные диагностические исследования
Биопсия миокарда и абдоминального жира
- Рекомендуется выполнение биопсии миокарда при подозрении на инфильтративные, воспалительные заболевания сердца или болезнях накопления, которые не могут быть подтверждены другими методами [3][73][338][339].
ЕОК IIаС (УДД 4, УУР С)
- Рекомендуется выполнение биопсии абдоминального жира при подозрении на амилоидоз [3][30][289][340][341].
ЕОК IIаВ (УДД 2, УУР B)
Комментарии. Биопсия подкожно жировой клетчатки более информативна при AL-амилоидозе и наследственном ATTR.
Эндомиокардиальная биопсия не требуется, если при сцинтиграфии степень накопления радиофармпрепарата в сердце по шкале Перуджини 2 или 3 и при этом лабораторно исключен AL-амилоидоз.
Эндомиокардиальная биопсия показана, если результаты сцинтиграфии сомнительны (по шкала Перуджини степень накопления 0 или 1), при отрицательном результате биопсии абдоминального жира, отрицательных гематологических тестах и высокой вероятности ATTR.
2.6. Диагностика заболевания у отдельных категорий пациентов
Дифференциальный диагноз ГКМП и ГЛЖ вследствие АГ
На естественное течение ГКМП оказывает влияние наличие факторов кардиометаболического риска (АГ, ожирение/избыточная масса тела), встречаемость которых увеличивается с возрастом [342-346].
В старшей возрастной группе пациентов с доказанной ГКМП встречаемость АГ составляет 70-90%. По определению при ГКМП ГЛЖ не обусловлена нагрузкой давлением, но АГ — это нагрузка давлением, поэтому в случае сочетания ГКМП с АГ требуется модификация критериев ГКМП.
Вероятность ГКМП у пациентов с АГ повышается при наличии одного и более из следующих критериев:
- Указание на семейный анамнез ГКМП или ВСС в молодом возрасте у родственников первой линии родства;
- Несоответствие между выраженной ГЛЖ (максимальная толщина стенок ≥15 мм) и недавно возникшей легкой и умеренной АГ при адекватной приверженности пациента терапии, а также других причин, способных вызвать подобную степень ГЛЖ.
Возможным вариантом критерия ГКМП при сопутствующей АГ является толщина миокарда ЛЖ ≥20 мм; толщина миокарда 15-20 мм представляет "серую зону".
Выбор критерия ГКМП "толщина стенки ЛЖ ≥20 мм" при сопутствующей АГ обусловлен тем, что показано: при перегрузке давлением (АГ, АС или их сочетание) толщина миокарда ЛЖ, как правило, не превышает 20 мм (в некоторых исследованиях превышает 20 мм лишь у единичных пациентов) [98][331][342][343][347-353].
Если выявленная толщина миокарда у пациента в "серой зоне" (15-20 мм), то вывод о диагнозе ГКМП можно сделать только на основании тщательного анализа большого числа факторов: семейный анамнез, длительность АГ, уровень "нагрузки давлением" (эпизодические повышения АД или стабильно повышенное АД), приверженность пациента терапии АГ, наличие изменений ЭКГ/ЭхоКГ до развития АГ, динамика размеров полостей сердца и увеличения толщины стенок ЛЖ при ЭхоКГ/МРТ и др. [52].
Следует также учитывать, что при АГ может наблюдаться асимметричная ГЛЖ — по некоторым данным, до 20% (т.е. соотношение толщины МЖП/толщины задней стенки >1,5) [349][351].
ГКМП и базальная септальная гипертрофия (S-образная МЖП с "выпуклостью" в базальном сегменте)
У пожилых пациентов с S-образной МЖП может выявляться "выпуклость" (англ. bulge) в базальной части перегородки, которая не обусловлена ГКМП. Как правило, у этих пациентов присутствует сопутствующая АГ и/или патология АК (небольшая аортальная регургитация и/или невыраженный АС) [262][263][349][350][354].
Базальная септальная гипертрофия может приводить к увеличению ГД в ВТЛЖ, как правило, не выше 15-20 мм рт.ст. в покое и возрастать до 35 мм рт.ст. при нагрузочных пробах [331].
Схема дифференциального диагноза ГКМП и базальной септальной гипертрофии представлена в таблице 15, Приложение А3.
ГКМП и ИМ 1 и 2 типов
Клинически у пациентов с ГКМП и ишемией миокарда (INOCA — Ischemia with Non-Obstructive Coronary Arteries) может развиваться острый коронарный синдром (ОКС) и ИМ [90][92][104][311].
ИМ при необструктивном поражении эпикардиальных коронарных артерий (ИМБОКА, MINOCA) — это "рабочий диагноз", требующий уточнения причины, лежащей в основе у конкретного пациента.
В генезе ИМ при ГКМП могут обсуждаться следующие патогенетические механизмы:
- INOCA (см. Раздел "Патогенез");
- Ишемия при обструктивном поражении эпикардиальных коронарных артерий — ИБС в старшей возрастной группе пациентов с ГКМП (см. также таблицу 2, Приложение А3).
При ГКМП может развиться ИМ 1 типа, диагностика и лечение которого изложены в соответствующих клинических рекомендациях.
Для исключения/подтверждения обструктивного поражения эпикардиальных коронарных артерий пациентам с ГКМП показана инвазивная КАГ или КТ-ангиография. Одновременно с КАГ пациентам с ГКМП рекомендуется выполнять вентрикулографию сердца, которая выявляет у пациента либо "эпикардиальный паттерн" (зоны нарушения сократимости в пределах стенозированных коронарных артерий), либо "микроваскулярный паттерн" (зоны нарушения сократимости в бассейнах разных коронарных артерий, в т.ч. и без стенозов) [90][92][93][101][102][104][314][355-360].
Данный феномен в отечественной литературе называется ИМБОКА (MINOCA) или ИМ 2 типа. ИМ 2 типа — это ИМ, развивающийся без атеротромбоза, из-за несоответствия между потребностью миокарда в кислороде и его доставкой.
INOCA имеет общий патогенетический механизм как при КМП, так и при фенокопиях ГКМП, например, при амилоидной КМП [71].
ГКМП и ГЛЖ у спортсменов. Рекомендации по занятию спортом, физкультурой, участию в спортивных соревнованиях
Пациентам с ГКМП независимо от возраста, пола, расовой принадлежности, наличия обструкции ВТЛЖ, проведенных ранее операции СМЭ или ЭСА или установки ИКД*** не рекомендовано (противопоказано) участие в спортивных соревнованиях и упражнениях высокой интенсивности [3][20][135][197][241][321][361-364].
ЕОК IIIC (УДД 5, УУР С)
Комментарии. Из-за высокого риска ВСС занятия соревновательными видами спорта высокой интенсивности пациентам с ГКМП противопоказаны.
- Большинству пациентов с ГКМП рекомендуется рассмотреть возможность выполнения физических упражнений легкой и умеренной интенсивности (без систематических тренировок и участия в соревнованиях) для улучшения функционального статуса, физической реабилитации и качества жизни [1][2].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
- Для большинства пациентов с ГКМП рекомендуется рассмотреть возможность участия в спортивных соревнованиях низкой интенсивности после всесторонней оценки рисков и совместного обсуждения с экспертами [1][2].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
- Носителям генетических вариантов IV-V класса (патогенных/вероятно патогенных) при отсутствии фенотипических проявлений рекомендуется рассмотреть возможность участия в спортивных соревнованиях любой интенсивности [1][2].
ЕОК нет/РКО IIbC (УДД 5, УУР С)
- У пациентов с ГКМП не рекомендуется установка ИКД*** только с целью возможности участия в спортивных соревнованиях [1][2].
ЕОК нет/РКО IIIC (УДД 5, УУР С)
Комментарии. Для фенотип-негативных носителей генетических вариантов IV-V класса (патогенных/вероятно патогенных) рекомендации по оптимальному уровню физической активности и характеру физических нагрузок должны быть сформулированы после консилиума с участием мультидисциплинарной команды специалистов (врач-генетик, врач-кардиолог, врач по спортивной медицине, медицинский психолог и др.) на основе рассмотрения выявленной мутации, результатов регулярных и повторных клинических исследований (МРТ с контрастированием, проведение стресс-ТТ-ЭхоКГ), с учетом стратификации риска ВСС на основе европейской и американской моделей.
Необходимо учесть, что в некоторых случаях ТТ-ЭхоКГ может некорректно оценивать толщину стенки ЛЖ. Например, в исследовании Huurman R, et al. почти 25% носителей генотип(+)/фенотип(-) по данным ТТ-ЭхоКГ после проведения МРТ переклассифицированы в генотип(+)/фенотип(+) [284]. Для рекомендации спортсменам по возможности участия в соревнованиях это имеет принципиальное значение.
Спортсмены высокого класса с ГЛЖ и толщиной стенки ЛЖ >13 мм (13-15 мм) составляют лишь небольшую часть (1,5-1,7%). Как правило, это спортсмены с большой массой тела. Именно у этой группы требуется дифференциальный диагноз с ГКМП [241][362][364].
Наиболее часто используемые показатели для дифференциальной диагностики ГКМП и адаптивной ГЛЖ у спортсменов представлены в таблице 16, Приложение А3.
Важным дифференциально-диагностическим признаком является выявление ПНГ при МРТ с контрастированием. Как правило, это свидетельствует в пользу ГКМП, однако отсутствие ПНГ не исключает заболевания. Однако у спортсменов с ГЛЖ, занимающихся аэробными видами спорта (марафонцы, велосипедисты и др.), могут наблюдаться отдельные участки ПНГ малого размера.
Анализируя спортивную ГЛЖ, необходимо также принимать в расчет следующие факторы: вид спорта и интенсивность тренировок, возраст, пол (у мужчин ГЛЖ больше), рост и вес спортсмена. Окончательный вывод о диагнозе ГКМП у спортсмена делается на основе комплексной оценки как можно большего числа показателей.
2.7. Стратификация риска и стратегии первичной и вторичной профилактики внезапной сердечной смерти
Показатели ежегодной смертности от сердечно-сосудистых причин у взрослых пациентов с ГКМП составляют 1-2%. ВСС, ХСН и тромбоэмболические осложнения являются основными причинами.
ВСС — это смерть, наступающая неожиданно и мгновенно из-за кардиальных причин (у пациента без заболевания сердца или с таковым) в течение 1 ч после появления первых симптомов ухудшения общего состояния.
К понятию ВСС не относят случаи насильственной смерти или смерти, возникающей в результате отравления, асфиксии, травмы или другого какого-либо несчастного случая.
Риск ВСС у пациентов с ГКМП без традиционных факторов риска составляет 5,9% за 10 лет [3][132].
- 5-летний риск ВСС рекомендуется оценивать при первичном обследовании пациента с ГКМП и в дальнейшем переоценивать каждые 1-3 года или при изменении клинического статуса [3][129][137][240][365][366].
ЕОК IС (УДД 3, УУР В)
- Шкала HCM Risk-SCD рекомендуется в качестве метода оценки риска внезапной смерти в течение 5 лет для пациентов с ГКМП ≥16 лет без случаев реанимации после эпизодов ЖТ/ФЖ или спонтанной устойчивой ЖТ с потерей сознания или гемодинамическими нарушениями [3][129][131][137][238][239][258][324].
ЕОК IB (УДД 3, УУР B)
Комментарии. Регистрация жизнеугрожающих ЖНР и брадиаритмий осуществляется с помощью поверхностной ЭКГ в покое, при ХМ сердечного ритма, с помощью наружного или имплантируемого записывающего устройства, также — при нагрузочной пробе [238].
Также недавние исследования показали, что регистрация ЭКГ с подъемом точки J и выемкой в конце QRS или наличием J-волны на нисходящей части зубца R ≥1 мм в двух и более отведениях (обычно в нижнелатеральных) за исключением V1-V3, была положительно связана с такими событиями, как ВСС, ЖНР и ФЖ [367].
Независимо от нозологии, подавляющее большинство опасных для жизни желудочковых нарушений сердечного ритма (83,4%) обусловлено электрической нестабильностью миокарда. ВСС чаще обусловлена ФЖ (62,4%), брадиаритмиями (16,5%), ЖТ типа "torsades de pointes" (12,7%) и ЖТ (8,3%).
ЖТ неустойчивая — ЖТ, состоящая как минимум из 3 желудочковых комплексов, с частотой ≥120 и продолжительностью не более 30 сек, которая прекращается самостоятельно. ЖТ может быть мономорфной (неизмененная морфология комплекса QRS в 12 отведениях) и полиморфной (во время ЖТ в 12 отведениях ЭКГ изменяется конфигурация комплекса QRS).
ЖТ устойчивая (мономорфная, полиморфная) — ЖТ продолжительностью >30 сек, зачастую не купирующаяся самостоятельно.
ФЖ — нерегулярный желудочковый ритм (обычно с частотой >300 уд./мин) с выраженной вариабельностью длины цикла, морфологии и амплитуды комплексов QRS.
Существует две модели стратификации риска ВСС:
- На основе традиционных факторов риска (американская модель);
- На основе расчета индивидуальных оценок риска, персонифицированный подход (европейская модель) — шкала HCM Risk-SCD.
Шкала оценки риска ВСС у пациентов с ГКМП (европейская модель) представлена в Приложении Г2.
"Калькулятор" риска ВСС при ГКМП по европейской модели представлен на сайте http://doc2do.com/hcm/webHCM.html.
Шкала оценки риска ВСС у пациентов с ГКМП (американская модель) представлена в Приложении Г3 (см. калькулятор на сайте https://professional.heart.org/en/guidelines-and-statements/hcm-risk-calculator).
Европейская модель прогнозирования риска ВСС HCM Risk-SCD имеет ограничения:
- Не применяется у пациентов старше 80 лет и моложе 16 лет;
- Не применяется у пациентов с фенокопиями ГКМП, ГЛЖ у спортсменов;
- После СМЭ.
После ЭСА может использоваться шкала HCM Risk-SCD (европейская). Модель ASA-SCARE Risk Score для прогнозирования риска ВСС находится в процессе валидации [368].
Проведена модификация формулы расчета с использованием такого фактора, как максимальная толщина стенки ЛЖ (в HCM Risk-SCD Calculator — рекомендовано указывать не более 35 мм) (продолжается апробация новой модели) [240].
Алгоритм первичной и вторичной профилактики ВСС у пациентов с ГКМП представлен в Приложении Б7.
3. Лечение, включая медикаментозную и немедикаментозную терапии, диетотерапию, обезболивание, медицинские показания и противопоказания к применению методов лечения
Лечение ГКМП включает медикаментозную терапию, эндоваскулярные вмешательства, хирургические и нехирургические методы редукции гипертрофированной МЖП, механическую поддержку кровообращения, трансплантацию сердца.
Рекомендации по лечению ГКМП основаны на данных об эффективности и безопасности применяемых фармакологических средств, полученных в основном в наблюдательных исследованиях.
Фармакотерапия при ГКМП в основном улучшает симптоматику и предупреждает осложнения (антикоагулянтная терапия при ФП, кордарон-фармакологическая кардиоверсия и профилактика рецидивов ФП, лечение желудочковых нарушений сердечного ритма и др.) [178][369-371].
Единственными вмешательствами при ГКМП, которые, как полагают, влияют на долгосрочный прогноз, являются СМЭ и имплантация ИКД [366][372-377].
Лечение сопутствующих заболеваний при ГКМП рассмотрено в соответствующих разделах (АГ, стенокардия, ОКС, ХСН).
Коррекцию факторов сердечно-сосудистого риска (дислипидемия, сахарный диабет и т.п.) у больных ГКМП рекомендуется проводить в соответствии с существующими клиническими рекомендациями [378].
3.1. Медикаментозная терапия
3.1.1. Подходы к медикаментозной терапии на гипертрофической стадии ГКМП у бессимптомных пациентов
- Не рекомендуется назначение бета-адреноблокаторов или блокаторов "медленных" кальциевых каналов (недигидропиридиновых блокаторов "медленных" кальциевых каналов (селективные блокаторы кальциевых каналов с прямым действием на сердце: верапамил**, дилтиазем)) пациентам с бессимптомным течением необструктивной ГКМП, т.к. их полезное действие не доказано [1][3][20][39].
ЕОК IIIC (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность назначения бета-адреноблокаторов или верапамила** асимптомным взрослым с обструкцией ВТЛЖ (покоя или индуцируемой) для снижения ГД в ВТЛЖ [3][379][380].
ЕОК IIbC (УДД 4, УУР С)
Комментарии. Симптомный или асимптомный пациент, решает врач после детального обследования.
Эти пациенты нередко имеют ограничение переносимости физических нагрузок, которое усугубляется приемом пищи.
Должен быть решен вопрос об отличии истинного отсутствия симптомов от адаптации за счет образа жизни, путем проведения теста с ФН и оценки биомаркеров ХСН в динамике.
Необходима ежегодная переоценка риска ВСС, включающая ЭКГ, ХМ сердечного ритма, ЭхоКГ.
Алгоритм тактики ведения асимптомных пациентов с ГКМП представлен в Приложении Б1.
3.1.2. Медикаментозная терапия симптомных пациентов с ГКМП
Общие принципы медикаментозной терапии:
- Лечение пациентов с обструктивной и необструктивной формами заболевания имеет существенные различия.
- Лечение должно быть адаптировано к уникальным характеристикам каждого отдельного пациента.
- Лекарственные препараты, традиционно применяемые в терапии ГКМП, являются средствами с отрицательным инотропным действием и направлены на купирование или облегчение симптомов заболевания.
- Правожелудочковая ОГКМП и двухжелудочковая ОГКМП лечатся по тем же принципам, как и при обструкции ВТЛЖ.
3.1.3. Медикаментозная терапия обструкции ВТЛЖ
- У пациентов с ОГКМП лечение любыми лекарственными средствами рекомендуется начинать с минимальных доз и с осторожным их титрованием в течение достаточно долгого времени [1][3][20][39][62][63][379][381].
ЕОК IB (УДД 3, УУР B)
Комментарии. Упрощенный алгоритм диагностики и подходов к лечению обструктивных форм ГКМП представлен в Приложении Б2. Алгоритм фармакотерапии ОГКМП представлен в Приложении Б3.
- У пациентов с обструкцией ВТЛЖ (покоя и индуцируемой) бета-адреноблокаторы с подбором максимальной переносимой дозы рекомендуются в качестве первой линии терапии для уменьшения симптомов [1][3][20][147][379][381-384].
ЕОК IB (УДД 3, УУР B)
Комментарии. Правила и особенности назначения бета-адреноблокаторов представлены в таблице 17, Приложение А3.
- Верапамил** с подбором максимальной переносимой дозы рекомендуется тем пациентам с обструкцией ВТЛЖ (покоя или индуцируемой), которые не переносят бета-адреноблокаторы или имеют противопоказания к их назначению [1][3][20][379][380][385][386].
ЕОК IB (УДД 2, УУР B)
Комментарии. Правила и особенности назначения верапамила** представлены в таблице 18, Приложение А3.
- Рекомендуется рассмотреть возможность назначение дилтиазема с подбором максимальной переносимой дозы симптомным пациентам с обструкцией ВТЛЖ (покоя или индуцируемой), которые не переносят бета-адреноблокаторы, верапамил** или имеют противопоказания к их назначению [1][3][20][379][385].
ЕОК IIaС (УДД 2, УУР B)
Комментарии. Рекомендуемые начальные и целевые дозы при медикаментозной терапии ГКМП представлены в таблице 19, Приложение А3.
Пациентам с ГКМП и среднежелудочковой обструкцией ЛЖ рекомендуются высокие дозы бета-адреноблокаторов (бисопролол**), или верапамила**, или дилтиазема. Ответ на лечение высокими дозами бета-адреноблокаторов, или верапамила**, или дилтиазема у пациентов с ГКМП и среднежелудочковой обструкцией ЛЖ часто неоптимальный. Эта когорта пациентов, как правило, имеет симптомный вариант течения, характеризующийся повышенным риском прогрессии симптомов ХСН и ВСС. Частота выявления аневризмы верхушки ЛЖ варьирует от 10% до 25%. Выработка оптимальной врачебной тактики у таких пациентов должна осуществляться мультидисциплинарной командой [87-89][387-391].
Алгоритм врачебной тактики лечения ХСН при ГКМП представлен в Приложении Б4.
- Пациентам с ОГКМП и острой гипотензией, которые не реагируют на введение жидкости, рекомендуется внутривенное введение фенилэфрина** или других вазоконстрикторов без инотропной активности, отдельно или в комбинации с бета-адреноблокаторами [1][3][20][147][379].
ЕОК IС (УДД 5, УУР С)
- Пациентам с ГКМП и обструкцией ВТЛЖ (покоя или индуцируемой) не рекомендуется применение органических нитратов и ингибиторов фосфодиэстеразы [1][3][20][379].
ЕОК IIIС (УДД 5, УУР С)
- Пациентам с ГКМП и обструкцией ВТЛЖ (покоя или индуцируемой) не рекомендуется применение дигидропиридиновых блокаторов "медленных" кальциевых каналов (селективные блокаторы кальциевых каналов с преимущественным действием на сосуды) производных дигидропиридинов (нифедипин**) [1][3][20][379].
ЕОК IIIС (УДД 5, УУР С)
Комментарии. Основной нежелательный механизм действия органических нитратов и ингибиторов фосфодиэстеразы обусловлен увеличением обструкции ВТЛЖ.
- Пациентам с ГКМП и обструкцией ВТЛЖ (покоя и индуцируемой) не рекомендуется дигоксин** [154][392].
ЕОК IIIC (УДД 5, УУР С)
- Верапамил** не рекомендуется пациентам с ОГКМП в случаях наличия системной гипотензии и выраженной одышки в покое [1][379][382][393].
ЕОК IIIС (УДД 5, УУР С)
3.1.4. Лечение ХСН у больных ГКМП
Распространенность ХСН у пациентов с ГКМП составляет от 17% до 67% в зависимости от ФК [148][394][395].
ХСН у пациентов с ГКМП проявляется двумя фенотипами: с сохраненной ФВ ЛЖ в 85-90% случаев и в 8-10% — с низкой ФВ ЛЖ, которая формируется в более поздней стадии ГКМП или в результате других сопутствующих заболеваний [147][152][183][184].
ХСН распространена у большинства больных с ОГКМП и у 10% пациентов при отсутствии обструкции. Острая сердечная недостаточность при ГКМП встречается редко и может быть вызвана такими состояниями, как тахиаритмия, ИМ, острая или ухудшающаяся МР или сопутствующими заболеваниями [396][397].
- У больных ГКМП при появлении симптомов ХСН рекомендуется проводить диагностику в соответствии с клиническими рекомендациями по ХСН [153].
ЕОК IС (УДД 5, УУР С)
- У больных ГКМП и ХСН независимо от ФВ ЛЖ рекомендуется рассмотреть возможность назначения немедикаментозных рекомендаций (обучение, диета, снижение веса, ограничение соли, ФН) в зависимости от ФК ХСН в соответствии с клиническими рекомендациями по ХСН [153][154].
ЕОК IIbС (УДД 5, УУР С)
- У больных необструктивной ГКМП для лечения ХСН рекомендуется рассмотреть возможность назначения лекарственных препаратов в соответствии с клиническими рекомендациями по ХСН [1][3][148][153][154][398].
ЕОК IIbС (УДД 5, УУР С)
Комментарии. При наличии признаков застоя для избежания гиповолемии рекомендуется осторожное применение низких доз петлевых или тиазидных диуретиков [154]. Верапамил**/дилтиазем рекомендуются у больных ХСН с сохраненной ФВ ЛЖ >50%, если бета-адреноблокаторы противопоказаны, не переносятся или неэффективны [154].
- У пациентов c обструктивной ГКМП и ХСН рекомендуется применение невазодилатирующих бета-адреноблокаторов как терапия первой линии для уменьшения клинических симптомов ХСН и снижения ГД в ВТЛЖ [1][3][148][153][154][384].
ЕОК IIaB (УДД 2, УУР B)
Комментарии. Верапамил**/дилтиазем у пациентов c обструктивной ГКМП и ХСН с сохраненной ФВ ЛЖ >50% могут быть рассмотрены как первая линия, если бета-адреноблокаторы противопоказаны, не переносятся или неэффективны [154].
У пациентов с обструктивной ГКМП и ХСН при наличии признаков застоя рекомендуется рассмотреть возможность назначения низких доз петлевых или тиазидных диуретиков [154].
ЕОК IIbС (УДД 5, УУР С)
Комментарии. Следует избегать условий, при которых происходит уменьшение объема циркулирующей крови (гиповолемия), для предотвращения увеличения ГД в ВТЛЖ.
- У пациентов с обструктивной ГКМП и ХСН ингибиторы ангиотензинпревращающего фермента (иАПФ)/антагонисты рецепторов к ангиотензину II (АРА), дигоксин** не рекомендуются из-за риска увеличения ГД в ВТЛЖ [154][392].
ЕОК IIIС (УДД 5, УУР С)
Комментарии. Спиронолактон** у пациентов ГКМП не улучшает симптоматику ХСН [399].
Препараты, рекомендуемые для лечения ХСН с низкой, промежуточной и сохраненной ФВ ЛЖ [153], такие как ингибиторы натрийзависимого переносчика глюкозы 2 типа, эплеренон, валсартана/сакубитрил**, ивабрадин**, омега-3-полиненасыщенные жирные кислоты, не изучались при обструктивной ГКМП и ХСН. Решение о назначении данных групп препаратов пациентам с обструктивной ГКМП и ХСН может быть принято только мультидисциплинарной командой.
Гиперконтрактильность сердечной мышцы является ключевым патофизиологическим механизмом при ГКМП и основным фактором, определяющим динамическую обструкцию ВТЛЖ. Доступные фармакологические варианты лечения ГКМП не являются специфичными для заболевания. Проводятся клинические исследования лекарственных препаратов с таргетным воздействием на основной патогенетический механизм [400].
3.1.5. Лечение стенокардии у пациентов с ГКМП
Стенокардия/ишемия миокарда является часто встречающимся синдромом у больных ГКМП [401].
Патогенетические механизмы формирования стенокардитического синдрома при ГКМП различны: повышение потребности миокарда в кислороде из-за большей его массы и повышенного давления наполнения [55][402][403]; уменьшение регионального кровотока за счет атеросклероза эпикардиальных коронарных артерий [404]; аномалии коронарного кровообращения и мышечные мостики, способствующие ишемии за счет длительного сдавления и снижения кровотока в ранней диастолической фазе [405]; коронарная микрососудистая дисфункция при отсутствии значимых стенозов эпикардиальных коронарных артерий [406-408].
Частота встречаемости ишемии/стенокардии, связанной с атеросклерозом коронарных артерий, у больных ГКМП составляет в среднем 20%, стенокардии при необструктивной коронарной дисфункции — 51-86% [106][409].
Частота развития ОКС у больных ГКМП при необструктивном поражении коронарных артерий сопоставима с частотой при наличии коронарного атеросклероза [409]. У пациентов с ГКМП и ОКС при необструктивном поражении коронарного русла регистрируется более низкая вероятность смерти по сравнению с пациентами с коронарным атеросклерозом [409].
- Диагностику стенокардии у пациентов с ГКМП рекомендуется проводить в соответствии с клиническими рекомендациями по стабильной стенокардии [410].
ЕОК IС (УДД 5, УУР С)
Медикаментозное лечение синдрома стенокардии у больных ГКМП определяется наличием обструкции ВТЛЖ и патогенетическим механизмом коронарной дисфункции [411].
- У пациентов с необструктивной ГКМП лечение стенокардии рекомендуется проводить в соответствии с клиническими рекомендациями по стабильной стенокардии [410].
ЕОК IС (УДД 5, УУР С)
- У пациентов с обструктивной ГКМП применение иАПФ/АРА не рекомендуется из-за риска увеличения ГД в ВТЛЖ [392].
ЕОК IIIС (УДД 5, УУР С)
- У пациентов с обструктивной ГКМП рекомендуется применение бета-адреноблокаторов как препаратов первой линии для устранения приступов стенокардии и снижения ГД в ВТЛЖ независимо от патогенетического механизма коронарной дисфункции [1][3][93][412][413].
ЕОК IIаB (УДД 2, УУР B)
- У больных обструктивной ГКМП рекомендуется рассмотреть возможность назначения верапамила** или дилтиазема для устранения приступов стенокардии независимо от патогенетического механизма коронарной дисфункции [380][385][414][415].
ЕОК IIbС (УДД 2, УУР В)
Комментарии. Правила и особенности назначения верапамила** представлены в таблице 18, Приложение А3 и таблице 19, Приложение А3.
У больных необструктивной ГКМП верапамил** способен уменьшать ишемию миокарда, в т.ч. безболевую, и улучшать диастолическую функцию ЛЖ [383].
Применение верапамила** или дилтиазема ЛЖ c целью устранения симптомов противопоказано (не рекомендовано) у больных ГКМП и стенокардией при наличии ХСН с низкой ФВ из-за наличия отрицательного инотропного действия, что способствует развитию декомпенсации ХСН [153].
- Не рекомендуется одновременное назначение верапамила** или дилтиазема с ивабрадином** у пациентов с ГКМП со стабильной стенокардией из-за риска развития брадикардии и ФП4 [416].
EOK/РКО IIIC (УДД 1, УУР B)
- У больных обструктивной ГКМП назначение органических нитратов не рекомендуется из-за риска увеличения ГД в ВТЛЖ [412].
EOK IIIB (УДД 5, УУР С)
- У больных обструктивной ГКМП рекомендуется рассмотреть возможность назначения комбинации антиангинальных препаратов (бета-адреноблокаторы, блокаторы "медленных" кальциевых каналов (блокаторы кальциевых каналов), органические нитраты длительного действия (органические нитраты), ивабрадин**, никорандил, ранолазин, триметазидин) для устранения приступов стенокардии в соответствии с клиническими рекомендациями по стабильной ИБС и решением мультидисциплинарной команды [410].
ЕОК IIbС (УДД 5, УУР С)
3.1.6. Лечение ОКС у пациентов с ГКМП
Среди пациентов с ИМ доля пациентов с ГКМП составляет в среднем 0,1% [417]. Среди больных ГКМП у 23% развивается ОКС в течение 11 лет наблюдения [409].
У пациентов с ГКМП чаще развивается ИМ 2 типа без подъема сегмента ST, при котором ниже госпитальная летальность, чем у пациентов без ГКМП [417][418].
Патогенетические механизмы формирования ОКС у пациентов с ГКМП различны: разрыв атеросклеротической бляшки эпикардиальной коронарной артерии регистрируется в 20% случаев [419], тромбоз при необструктивной коронарной дисфункции — в 51% в структуре причин [409].
Патофизиологические механизмы формирования тромбоза в коронарных артериях без атеросклеротического поражения при ГКМП связаны cо сдавлением внутримиокардиальных коронарных артерий и снижением кровотока в них в ранней диастолической фазе, вазоспазмом и эндотелиальной дисфункцией микрососудистого коронарного русла [420].
- У пациентов с необструктивной ГКМП лечение ОКС при наличии разрыва атеросклеротической бляшки коронарных артерий по данным КАГ рекомендуется проводить в соответствии с клиническими рекомендациями по ИМ с подъемом и без подъема сегмента ST [421][422].
ЕОК IС (УДД 5, УУР С)
- У пациентов с необструктивной ГКМП рекомендуется рассмотреть возможность лечения ОКС при необструктивной коронарной дисфункции в соответствии с клиническими рекомендациями по ИМ с подъемом и без подъема сегмента ST [421][422].
ЕОК IIbС (УДД 5, УУР С)
Комментарии. Метаанализы наблюдательных исследований продемонстрировали, что у пациентов с ОКС с необструктивной коронарной дисфункцией применение иАПФ/АРА, бета-адреноблокаторов, статинов, двойной антитромбоцитарной терапии снижает относительные риски больших сердечно-сосудистых событий и/или смертельных исходов [423][424].
Есть мнение, что выбор антитромбоцитарных средств и их терапевтический эффект может варьировать в зависимости от патофизиологических механизмов развития ИМ при необструктивной коронарной дисфункции, но определение их крайне затруднительно в диагностике ОКС [425-427].
- У пациентов с обструктивной ГКМП независимо от патогенетического механизма развития тромбоза рекомендуется рассмотреть возможность лечения ОКС в соответствии с клиническими рекомендациями по ИМ с подъемом и без подъема сегмента ST за исключением иАПФ/АРА из-за риска увеличения ГД в ВТЛЖ при их применении [428].
ЕОК IIbС (УДД 4, УУР С)
3.1.7. Лечение АГ у пациентов с ГКМП
У 37% больных ГКМП регистрируется АГ, что в целом соответствует распространенности в общей популяции [45].
АГ у больных ГКМП не влияет на риск смерти, связанный с ГКМП, но увеличивает риск больших сердечно-сосудистых событий и ХСН [49].
Прогноз пациентов с ГКМП, получающих антигипертензивную терапию, лучше, включая снижение смертности [50].
- Диагностику АГ у пациентов с ГКМП рекомендуется проводить в соответствии с клиническими рекомендациями по АГ [429].
ЕОК IС (УДД 5, УУР С)
- У пациентов ГКМП и АГ рекомендуется достижение целевых показателей АД в соответствии с клиническими рекомендациями по АГ, специальных целевых значений АД не установлено [429].
ЕОК IС (УДД 5, УУР С)
- Пациентам ГКМП и АГ рекомендуются немедикаментозные меры (обучение, диета, снижение массы тела, ограничение соли, ФН) в соответствии с клиническими рекомендациями по АГ [429].
ЕОК IС (УДД 5, УУР С)
- Пациентам с необструктивной ГКМП лечение АГ рекомендуется в соответствии с клиническими рекомендациями по АГ [429].
ЕОК IС (УДД 5, УУР С)
- У пациентов с обструктивной ГКМП и АГ рекомендуется назначение максимально переносимых доз невазодилатирующих бета-адреноблокаторов как терапия первой линии для снижения АД и ГД в ВТЛЖ [1][3][148][383][384].
ЕОК IIaB (УДД 3, УУР B)
- У больных обструктивной ГКМП и АГ рекомендуется рассмотреть возможность назначения верапамила** или дилтиазема, если бета-адреноблокаторы противопоказаны или не переносятся [1][3][148][430][431].
ЕОК IIbC (УДД 4, УУР C)
- Не рекомендуется комбинированное назначение бета-адреноблокаторов с верапамилом** или дилтиаземом у всех пациентов ГКМП и АГ из-за риска суммирования побочных эффектов [432].
ЕОК IIIC (УДД 5, УУР C)
- У больных обструктивной ГКМП и АГ при недостижении целевых показателей АД при использовании максимальных доз бета-адреноблокаторов или верапамила**/дилтиазема рекомендуется рассмотреть возможность применения низких доз тиазидных/тиазидоподобных диуретиков под контролем признаков гиповолемии [1][3][148][429].
ЕОК IIbС (УДД 4, УУР С)
Комментарии. При наличии хронической болезни почек и скорости клубочковой фильтрации <30 мл/мин/1,75 м² у больных ОГКМП и АГ при недостижении целевых показателей АД может быть рассмотрено осторожное применение низких доз петлевых диуретиков под контролем признаков гиповолемии [1][3][148][429].
- У пациентов с обструктивной ГКМП и АГ применение иАПФ/АРА не рекомендуется из-за риска увеличения ГД в ВТЛЖ [392].
ЕОК IIIС (УДД 5, УУР С)
- У больных обструктивной ГКМП не рекомендуется (противопоказано) назначение дигидропиридиновых блокаторов "медленных" кальциевых каналов (селективные блокаторы кальциевых каналов с преимущественным действием на сосуды, антагонисты кальция дигидропиридинового ряда (нифедипин**) из-за риска увеличения ГД в ВТЛЖ [412].
ЕОК IIIC (УДД 5, УУР C)
Комментарии. Препараты, рекомендуемые для лечения АГ, такие как спиронолактон**, валсартан/сакубитрил**, альфа-адреноблокаторы, моксонидин**, не изучались при ОГКМП и АГ с позиций контроля АД [429]. Решение о назначении данных групп препаратов может быть принято мультидисциплинарной командой при резистентности к проводимому антигипертензивному лечению под жестким контролем переносимости и гемодинамики.
3.1.8. Лечение ФП у пациентов с ГКМП
ФП является наиболее частой аритмией при ГКМП, распространенность которой зависит от тяжести заболевания: 22% в общей когорте и до 32% в когорте пациентов с показаниями для имплантации ИКД*** и ЭКС***/двухкамерного ЭКС*** [39][149][243][370][396][433][434].
Частота встречаемости ФП de novo в общей когорте ГКМП составляет ~2% в год [149][370][396].
Задачами фармакотерапии при ГКМП, осложненной ФП, являются купирование приступа, профилактика рецидивов аритмии и тромбоэмболических осложнений. Основные мероприятия по профилактике тромбоэмболических осложнений представлены в таблице 23, Приложение А3.
3.1.8.1. Восстановление синусового ритма и профилактика рецидивов ФП у пациентов ГКМП
- Для выявления бессимптомных или малосимптомных пароксизмов ФП и определения риска ВСС в когорте пациентов с ГКМП, размером ЛП ≥45 мм и с синусовым ритмом рекомендуется проведение 48-часового ХМ сердечного ритма каждые 6-12 мес. [1][3][127][146][150][238][370][435][436].
ЕОК IIaC (УДД 4, УУР C)
Комментарии. Обнаружение ФП с помощью имплантируемого петлевого регистратора представляет собой уникальную возможность для быстрого выявления бес- или малосимптомных пароксизмов ФП с целью профилактики тромбоэмболических осложнений до того, как случился инсульт. Предикторами риска возникновения ФП при ГКМП являются: предсердная КМП, увеличение размера и объема ЛП, повышение уровней NT-proBNP в крови, ХСН III-IV ФК, пожилой возраст, обструкция ВТЛЖ, вовлечение правых отделов сердца, генетические факторы.
- Рекомендуется восстановление синусового ритма путем прямой электрической или фармакологической кардиоверсии с внутривенным введением амиодарона** у пациентов с недавно возникшей (<48 ч) ФП [1][146][150][243][435][437].
ЕОК IIaC (УДД 5, УУР C)
Комментарии. Пациентам с гемодинамической нестабильностью на фоне пароксизма ФП рекомендована экстренная электрическая кардиоверсия по тем же правилам, как и пациентам без ГКМП.
Гемодинамически стабильным пациентам без предшествующей антикоагулянтной подготовки кардиоверсия может быть проведена только в случае, если длительность текущего пароксизма не превышает 48 ч. У пациентов с бессимптомными пароксизмами ФП, а также в ситуациях, когда пациент затрудняется назвать длительность текущего пароксизма и не получает антикоагулянтную терапию постоянно, рекомендуется воздержаться от незамедлительного восстановления синусового ритма.
В этой ситуации возможно применение двух стратегий ведения.
Первая стратегия: проведение ранней кардиоверсии после ЧП-ЭхоКГ, не выявившей тромбы в полостях предсердий. Антикоагулянтная поддержка во время процедуры восстановления синусового ритма обязательна.
Вторая стратегия: при невозможности проведения ЧП-ЭхоКГ или выявлении тромбов в полостях предсердий при ЧП-ЭхоКГ следует проводить позднюю кардиоверсию после 3 нед. антикоагулянтной терапии (после контрольной ЧП-ЭхоКГ, обязательной в случае наличия тромбов в полостях предсердий при первом обследовании).
Принимая во внимание тот факт, что ФП у пациентов, страдающих ГКМП, как правило, протекает с выраженной симптоматикой, восстановление синусового ритма должно рассматриваться не только при недавно возникшей, но и при персистирующей форме ФП, когда восстановление синусового ритма представляется весьма вероятным.
- У пациентов ГКМП после прямой электрической или фармакологической кардиоверсии рекомендуется назначение терапии амиодароном** для профилактики рецидивов ФП [1][146][150][369][370][435][437][438].
ЕОК IIaB (УДД 4, УУР С)
Комментарии. Амиодарон** является самым эффективным антиаритмическим препаратом для профилактики ФП, он безопасен и эффективен у пациентов с ГКМП, осложненной ФП.
В случае, если амиодарон** назначается de novo, начать терапию следует с применения насыщающих доз препарата (насыщающие дозы и темпы насыщения в соответствии с рекомендациями для общей популяции пациентов, страдающих ФП) под регулярным контролем ЧСС и ЭКГ контролем продолжительности PQ и QT. В первые три дня терапии рекомендуется ежедневный ЭКГ контроль. Удлинение интервала QT до значений, превышающих 500 мс, требует снижения дозы или отмены препарата.
Молекула амиодарона** содержит два атома йода, в связи с чем амиодарон** оказывает влияние на метаболизм гормонов щитовидной железы за счёт ингибирования превращения трийодтиронина в общий тироксин (блокирует тироксин-5-дейодиназу). На фоне длительного хронического приёма амиодарона** могут наблюдаться нарушения функции щитовидной железы, как амиодарон-индуцированный гипотиреоз, так и гипертиреоз.
Исходно, до назначения амиодарона**, следует исключить наличие у пациента патологии щитовидной железы (выполнить ультразвуковое исследование щитовидной железы и паращитовидных желез и определить уровень тиреотропного гормона и антител к тиреопероксидазе в крови пациента). При наличии патологии щитовидной железы возможность назначения амиодарона** и/или продолжения терапии амиодароном** должна быть обсуждена с эндокринологом. В процессе лечения амиодароном** на регулярной основе (при отсутствии клинических подозрений на патологию щитовидной железы через 3 мес. от начала терапии и далее не реже 1 раза в 6 мес.) следует определять уровень тиреотропного гормона, при необходимости — выполнять ультразвуковое исследование щитовидной железы и паращитовидных желез, определять свободные трийодтиронин и общий тироксин и их соотношение. Амиодарон-индуцированный гипотиреоз, как правило, не требует отмены препарата. Лечение тироксином рекомендуется всем больным с манифестным амиодарон-индуцированным гипотиреозом. Субклинические формы обычно не требуют его назначения, но за пациентом следует осуществлять наблюдение с определением уровня гормонов щитовидной железы каждые 4-6 мес. Ведение пациентов с амиодарон-индуцированным тиреотоксикозом зависит от типа гипертиреоза. Различают амиодарон-индуцированный тиреотоксикоз 1 типа (развивается при наличии автономных активных узлов щитовидной железы или латентной болезни Грейвса), амиодарон-индуцированный тиреотоксикоз 2 типа (развивается вследствие деструктивного тиреоидита из-за цитотоксического эффекта амиодарона) и смешанную форму амиодарон-индуцированного тиреотоксикоза, для которой характерно сочетание обоих механизмов. Появление амиодарон-индуцированного тиреотоксикоза в большинстве случаев требует отмены препарата. При амиодарон-индуцированном тиреотоксикозе 1 типа показана терапия антитиреоидными препаратами, при амиодарон-индуцированном тиреотоксикозе 2 типа — глюкокортикоидами. Их комбинация рекомендуется при смешанном варианте амиодарон-индуцированного тиреотоксикоза. Решение о продолжении или отмене амиодарона при амиодарон-индуцированном тиреотоксикозе должно приниматься индивидуально совместно специалистами-кардиологами и эндокринологами с учетом пользы и риска [439-441].
Соталол** может использоваться в качестве альтернативного антиаритмического препарата в лечении ФП у пациентов ГКМП, особенно в случае имплантации ИКД***, хотя клинический опыт его применения ограничен. В то же время следует учитывать существенно более низкую эффективность соталола** в сравнении с амиодароном** и более выраженные проаритмогенные эффекты. Как и в случае назначения амиодарона**, терапия соталолом** требует регулярного контроля ЧСС, PQ и QT.
- Бета-адреноблокатор или верапамил** или дилтиазем рекомендуются для контроля частоты сокращений желудочков у пациентов с ГКМП, постоянной или персистирующей ФП [1][3][126][146][150][369][370][435][437][438].
ЕОК IC (УДД 5, УУР C)
Комментарии. Доказательная база, подтверждающая эффективность бета-адреноблокаторов, верапамила** или дилтиазема у пациентов, страдающих ГКМП, осложнённой ФП, отсутствует. Лечение бета-адреноблокаторами, верапамилом** или дилтиаземом должно осуществляться под контролем ЧСС и атриовентрикулярной проводимости.
- Рекомендуется рассмотреть возможность назначения низких доз дигоксина** у пациентов с необструктивной ГКМП, страдающих постоянной формой ФП и ХСН II-IV ФК с ФВ ЛЖ <50%, для контроля ЧСС [1][3][146][147][150][153][154][370][435].
ЕОК IIbC (УДД 5, УУР C)
Комментарии. Доказательная база, подтверждающая эффективность дигоксина** у пациентов, страдающих необструктивной ГКМП, осложнённой ФП, отсутствует. Индивидуальная доза дигоксина** определяется оптимальной концентрацией препарата в сыворотке крови (0,5-0,9 нг/мл), обеспечивающей наилучшее соотношение эффективности и безопасности [150].
Начальные и целевые дозы препаратов при лекарственной терапии ГКМП представлены в таблице 19, Приложение А3.
3.1.8.2. Профилактика тромбоэмболических осложнений у пациентов с ГКМП и ФП
- Антагонисты витамина K (варфарин**, целевое международное нормализованное отношение (МНО) 2,0-3,0) или прямые оральные антикоагулянты (ПОАК) (дабигатрана этексилат** или ривароксабан** или апиксабан**) рекомендуются всем пациентам с ГКМП при отсутствии противопоказаний, у которых развилась персистирующая, постоянная или пароксизмальная форма ФП, для профилактики тромбоэмболических осложнений [1][3][146][150][243][371][435][442-446].
ЕОК IC (УДД 2, УУР А)
Комментарии. Необходимо помнить об эмбриотоксичности варфарина** (см. Раздел "ГКМП у беременных").
Меньше данных по антикоагулянтной терапии при ТП, но риск тромбоэмболий при нём считается таким же, как при ФП.
- Рекомендуется оценка риска кровотечений при назначении ПОАК (прямых ингибиторов фактора Xa или ингибиторы тромбина прямые) в сочетании с ингибиторами агрегации тромбоцитов (антиагреганты кроме гепарина) или без них c помощью шкалы HAS-BLED [1][3][146][150][370][371][435][437][442][443][446][447].
ЕОК IIaB (УДД 4, УУР С)
Комментарии. 3 и более баллов по шкале HAS-BLED (не валидирована для пациентов с ГКМП) указывает на высокий риск кровотечений. У таких пациентов должны быть приняты меры предосторожности с лабораторным и клинико-инструментальным контролем (коагулограмма (ориентировочное исследование системы гемостаза); активированное частичное тромбопластиновое время; определение МНО). Прежде всего необходимо провести поиск потенциального субстрата кровотечения перед назначением ПОАК. Рекомендуемые лабораторные анализы целесообразно повторять по мере необходимости, но не реже 1 раза в год [146][150].
Шкала HAS-BLED — см. Приложение Г5.
Рекомендации по поиску потенциального субстрата кровотечения — см. таблицу 21, Приложение А3.
Так как патология почек ассоциируется не только с высоким риском тромботических осложнений, но и с высоким риском кровотечений, для обеспечения безопасной антикоагулянтной терапии требуется регулярный контроль креатинина сыворотки крови и расчёт клиренса креатинина по формуле Кокрофта-Голта без стандартизации к площади поверхности тела для выбора оптимальной дозы ПОАК [150].
Рекомендуемая частота обязательных анализов крови на креатинин у пациентов — см. таблицу 20, Приложение А3.
- Если пациент с ГКМП, осложненной ФП, не может принимать подобранную дозу варфарина** из-за побочных действий или невозможности поддерживать терапевтический уровень антикоагуляции (МНО 2,0-3,0), или осуществлять мониторинг МНО, рекомендуется использовать ПОАК (дабигатрана этексилат** или ривароксабан**, или апиксабан**) [1][3][146][150][243][371][435][442-446].
ЕОК IB (УДД 2, УУР А)
Комментарии. Варфарин** или дабигатрана этексилат** или ривароксабан** или апиксабан** следует назначать независимо от количества баллов, полученных пациентом по шкале CHA2DS2-VASc даже после одного эпизода ФП. Шкала CHA2DS2-VASc — см. Приложение Г4.
- Во всех случаях ГКМП, осложненной ФП, рекомендуется пожизненная терапия варфарином** (МНО 2,0-3,0) или ПОАК (дабигатрана этексилатом** или ривароксабаном** или апиксабаном**), даже если синусовый ритм был восстановлен и стойко удерживается [1][3][146][150][243][371][435][442-446].
ЕОК IC (УДД 2, УУР А)
- Пациентам с ГКМП, осложненной ФП без выраженного увеличения ЛП, в случаях рефрактерной к фармакотерапии симптоматики или невозможности использования антиаритмических препаратов или их неэффективности рекомендуется выполнение катетерных процедур [1][3][146][150][435].
ЕОК IIaB (УДД 5, УУР С)
Комментарии. Инвазивные методы лечения ФП — см. Раздел 3.2.
3.2. Хирургическое и интервенционное лечение гипертрофической кардиомиопатии
3.2.1. Редукция МЖП
При ОГКМП хирургический метод лечения является "золотым стандартом".
Для изолированной миоэктомии средние показатели госпитальной летальности составляют <2%, эффективность — более чем у 90% пациентов, частота осложнений — <5%.
- Редукция МЖП рекомендуется пациентам с ОГКМП с симптомами ХСН или с повторными обмороками, несмотря на оптимальную медикаментозную терапию [1][3][89][121][377][448][449].
ЕОК IВ (УДД 4, УУР С)
Комментарии. Под ОГКМП рассматриваются следующие варианты обструкции: ГД в ВТЛЖ (в покое или максимально провоцируемый) ≥50 мм рт.ст., в т.ч. при двухуровневой обструкции (среднежелудочковая обструкция или обструкция на уровне хорд); двухжелудочковая обструкция (ГД в ВТЛЖ в покое или максимально провоцируемый ≥50 мм рт.ст.; ГД в ВТПЖ >16 мм рт.ст. в покое). Вазовагальные обмороки у больного следует исключить (см. Приложение Б8).
- Рекомендуется рассмотреть возможность выполнения редукции МЖП в опытных центрах у пациентов с ОГКМП и ХСН II ФК при наличии дополнительных клинических факторов: тяжелая ЛГ III-IV ФК, связанная с обструкцией ВТЛЖ или МР; расширение полости ЛП с одним и более симптомными эпизодами ФП в анамнезе; молодые люди с очень высоким ГД (>100 мм рт.ст.) в ВТЛЖ в покое [1][450-460].
ЕОК IIbB (УДД 4, УУР С)
Комментарии. Редукция МЖП осуществляется с помощью СМЭ — хирургической миэктомии по Морроу (Morrow) в условиях ИК (А16.10.003.23 Миэктомия по Морроу (Morrow) в условиях ИК) с иссечением зоны асимметричной гипертрофии с использованием чрезаортального доступа; с иссечением гипертрофированной мышечной ткани в зоне обструкции из конусной части ПЖ; иссечение мышечной ткани в зоне гипертрофии при сочетанной обструкции выводных отделов обоих желудочков сердца; с иссечением гипертрофированной мышечной ткани в сочетании с пластикой выходных отделов обоих желудочков сердца; иссечение мышечной ткани в зоне гипертрофии с реконструкцией полостей желудочков сердца; с иссечением мышечной ткани в зоне гипертрофии в сочетании с пластикой МК; с иссечением мышечной ткани в зоне гипертрофии в сочетании с протезированием клапанов сердца; с иссечением мышечной ткани в зоне гипертрофии в сочетании с аортокоронарным шунтированием (A16.10.031.003 Иссечение мышечной ткани в зоне гипертрофии при сочетанной обструкции выводных отделов обоих желудочков сердца, A16.10.031.001 Иссечение зоны асимметричной гипертрофии с использованием чрезаортального доступа, A16.10.031.005 Иссечение мышечной ткани в зоне гипертрофии с реконструкцией полостей желудочков сердца) или ЭСА. Определяющим фактором для достижения хороших результатов СМЭ и ЭСА является опыт клиники, который должен измеряться более чем 50 процедурами, выполняемыми в год, и более чем 20 процедурами, выполняемыми сердечно-сосудистым или рентген-эндоваскулярным хирургом [3][121][461-467].
Редукция МЖП должна выполняться опытным специалистом, работающим в мультидисциплинарной команде экспертов в лечении ГКМП.
Показания к редукции МЖП представлены в Приложении Б10.
Алгоритм диагностики и врачебной тактики при синкопальных состояниях представлен в Приложении Б8.
Алгоритм выбора хирургического/эндоваскулярного вмешательства у пациентов с ГКМП представлен в Приложении Б5) (см. также рекомендации к МРТ).
Алгоритм выбора метода редукции МЖП при ГКМП представлен в Приложении Б6.
Сравнение СМЭ и ЭСА представлено в Приложении Б11.
- Пациентам ГКМП с показаниями к редукции МЖП и имеющим показания для других хирургических вмешательств (аномалии папиллярных мышц, ухудшающие обструкцию в ВТЛЖ, аномалии створок МК, тяжелая МР не SAM-ассоциированная, ФП, многососудистое поражение коронарных артерий или другие сопутствующие заболевания, требующие хирургического лечения) рекомендуется выполнение хирургической миоэктомии в опытных центрах, как более предпочтительный метод, чем ЭСА [1][3][376][465][466].
ЕОК IВ (УДД 2, УУР В)
Комментарии. Миэктомия по Морроу (Morrow) в условиях ИК трансаортальным доступом устраняет обструкцию ВТЛЖ, вызванную гипертрофированной МЖП, однако не устраняет аномалии МК, вносящие вклад в нарастании ГД ВТЛЖ и развитие МР (SAM-ассоциированной) [468].
Messmer BJ, et al. усовершенствовали миоэктомию по Morrow, расширив область резекции гипертрофированной МЖП в апикальном направлении к основанию папиллярной мышцы [469].
При выявлении двухуровневой обструкции (увеличенный ГД в ВТЛЖ и на уровне средней части полости ЛЖ) миоэктомия может быть расширена до середины полости ЛЖ и вокруг основания папиллярных мышц (A16.10.031.003 Иссечение мышечной ткани в зоне гипертрофии при сочетанной обструкции выводных отделов обоих желудочков сердца, A16.10.031.001 Иссечение зоны асимметричной гипертрофии с использованием чрезаортального доступа, A16.10.031.005 Иссечение мышечной ткани в зоне гипертрофии с реконструкцией полостей желудочков сердца).
В специализированных центрах, имеющих наибольший опыт по лечению пациентов с ГКМП, используется трансапикальный доступ, направленный на снижение ГД и уменьшение симптомов у пациентов со среднежелудочковой ОГКМП. В редких случаях при двухуровневой обструкции ЛЖ используют комбинированный трансапикальный + трансаортальный доступ или правожелудочковый и трансаортальный доступы [87][389][470-472].
При среднежелудочковой ОГКМП, при отсутствии выраженных аномалий МК может быть выполнена миоэктомия из ПЖ трансвентрикулярным или транспредсердным доступом. Этот хирургический доступ имеет преимущество перед трансаортальным доступом у пациентов молодого возраста с выраженной гипертрофией МЖП вследствие более низкого риска развития атриовентрикулярных блокад [473][474].
При выявлении двухжелудочковой обструкции (увеличенный ГД в ВТЛЖ >50 мм рт.ст. и увеличенный ГД в ВТПЖ >16 мм рт.ст.) может применяться комбинированный доступ: трансаортальным доступ и доступ со стороны ПЖ.
В специализированных центрах, имеющих наибольший опыт по лечению пациентов с ГКМП, при выявлении двухжелудочковой обструкции, при отсутствии аномалий подклапанных структур МК миоэктомия может быть выполнена из ПЖ трансвентрикулярным или транспредсердным доступом [121][462][475][476].
Аномалии структур аппарата МК, ассоциированные с ГКМП, должны быть устранены во время операции с целью снижения ГД в ВТЛЖ без замены МК.
Показателями эффективности процедуры миоэктомии при ЭхоКГ являются:
- Контакт передней створки МК и МЖП (SAM-syndrome) отсутствует;
- Остаточный ГД в ВТЛЖ при провокации должен быть не >20 мм рт.ст.;
- Отсутствие выраженной резидуальной МР <5%.
Пожелания пациента (после подробного обсуждения вариантов лечения) имеют значение для принятия окончательного решения.
Выбор метода редукции МЖП должен основываться на тщательном обследовании пациента и обсуждении мультидисциплинарной командой специалистов.
- Пациентам с ГКМП, которым показано выполнение редукции МЖП, первичное изолированное протезирование МК не рекомендуется с целью устранения обструкции ВТЛЖ [1].
ЕОК IIIB (УДД 5, УУР С)
Комментарии. Протезирование МК сопровождается худшим отдаленным прогнозом в сравнении с его реконструкцией. Протезирование МК в дополнении к миоэктомии значительно повышает госпитальную летальность [477][478].
- У пациентов с ОГКМП и максимальной толщиной МЖП <17 мм рекомендуется рассмотреть возможность выполнения открытого кардиохирургического вмешательства на МК и его подклапанном аппарате с целью устранения обструкции ВТЛЖ (иссечение мышечной ткани в зоне гипертрофии в сочетании с пластикой МК) [1][3][479][480].
ЕОК IIbС (УДД 2, УУР С)
Комментарии. В 2015г Ferrazzi P, et al. описал результаты техники "неглубокой миоэктомии и резекции вторичных хорд" у пациентов с ОГКМП и относительно тонкой перегородкой. Была продемонстрирована эффективность метода в снижении ГД в ВТЛЖ с 82±43 мм рт.ст. до 9±5 мм рт.ст. [481]. Эта методика была воспроизводимой и востребованной и также заслуженно получила развитие в Российской Федерации [465][480].
Также группой авторов под руководством Богачева-Прокофьева А. В. было продемонстрировано, что дополнительное к миоэктомии вмешательство на МК более эффективно позволяет устранить SAM-ассоциированную МР [465].
Этой же группой авторов было продемонстрировано, что протезирование МК в сравнении с реконструкцией МК сопровождается худшим отдаленным прогнозом и большим количеством тромбоэмболических осложнений [464].
Veselka J, et al. продемонстрировал, что ЭСА пациентам с МЖП ≤16 мм сопровождается такой же эффективностью с точки зрения редукции ГД ВТЛЖ; большим числом имплантаций постоянных ЭКС, но лучшим прогнозом, нежели пациенты с МЖП >16 мм [448].
- У больных с апикальной и смешанной формами необструктивной ГКМП с клиническими симптомами стенокардии или одышки на уровне 3-4 ФК ХСН, сохраняющимися, несмотря на проводимую максимальную медикаментозную терапию, а также ХСН с сохраненной ФВ ЛЖ и малым размером полости ЛЖ (индекс КДО ЛЖ <50 мл/м², индекс УО ЛЖ <30 мл/м²), рекомендуется рассмотреть возможность выполнения операции по ремоделированию полости ЛЖ (СМЭ) трансапикальным, трансаортальным или комбинированным доступом опытными хирургами в специализированных центрах для улучшения симптомов заболевания [482-484].
ЕОК нет/РКО IIbС (УДД 2, УУР С)
Комментарии. Таким образом, ЭСА также может быть рассмотрена как альтернативная опция у пациентов с "тонкой" перегородкой.
Специфического обезболивания при хирургических и инвазивных вмешательствах пациентам с ГКМП не требуется.
3.2.2. Инвазивные методы лечения ФП пациентов с ГКМП
- У пациентов с ОГКМП, которым не показана редукция МЖП и другое вмешательство на клапанах или коронарных артериях, рекомендуется рассмотреть возможность выполнения радиочастотной аблации аритмогенных зон, если ФП не может быть предотвращена антиаритмической терапией, или ЧСС не контролируется лекарственными препаратами, или связана с непереносимостью или побочными действиями лекарственных препаратов [3][126][146][370][435].
ЕОК IIbС (УДД 5, УУР С)
- У пациентов с ОГКМП, осложнённой ФП, рефрактерной к фармакотерапии, рекомендуется выполнение операции Maze ("Лабиринт") либо ее модификацию с применением радиочастотной и криоаблации при выполнении хирургической миоэктомии для контроля ритма [1].
ЕОК IIaB (УДД 5, УУР С)
Комментарии. В настоящий момент нет доказательств, что процедура "Лабиринт" у пациентов с ОГКМП, подвергающихся хирургической миоэктомии, улучшает отдаленную выживаемость [485].
Тем не менее данное вмешательство может способствовать длительному сохранению синусового ритма у этой когорты больных [486].
Если операция "Лабиринт" показана, то выполняться она должна как сопутствующая, после консилиума мультидисциплинарной команды, хирургом, имеющим опыт выполнения подобного вмешательства.
В центрах, использующих операцию "Лабиринт" (модификация III и IV), отмечают, что у пациентов с ГКМП это дополнительное вмешательство при хирургической миоэктомии является безопасным и эффективным.
Хирургическое лечение ФП у пациентов с ГКМП менее успешно, чем без ГКМП.
Предикторами неэффективности лечения ФП при ГКМП являются: выраженность гипертрофии и диастолической дисфункции ЛЖ, дилатация предсердий, длительность и тип ФП.
Наличие сопутствующей органической патологии, выбор метода и схема хирургической изоляции, а также опыт хирурга определяют успешность процедуры хирургического лечения ФП у пациентов с ГКМП.
При катетерной аблации пациентам с ГКМП и ФП чаще требуется проведение повторных процедур.
Ремоделирование предсердий, зависимое от ГКМП, может повлиять на исход, даже если процедура изначально успешна.
3.2.3. Рекомендации по практическим аспектам имплантации ИКД***
Алгоритм первичной и вторичной профилактики ВСС у пациентов с ГКМП представлен в Приложении Б7.
Шкала оценки риска ВСС у пациентов с ГКМП (европейская модель) представлена в Приложении Г2.
Шкала оценки риска ВСС у пациентов с ГКМП (американская модель) представлена в Приложении Г3.
Американская модель позволяет оценивать риск ВСС у пациентов с низким/средним риском.
Наличие распространенного фиброза, оцениваемого по ПНГ при МРТ (≥15% от массы ЛЖ), является предиктором риска ВСС при ГКМП. Этот показатель не входит в европейскую модель стратификации риска, однако, если у пациента низкий или средний риск ВСС (<6%), а при МРТ площадь фиброза ≥15% от массы ЛЖ — это является дополнительным аргументом в пользу установки ИКД*** [129][487].
Шкалы не применимы к пациентам ГКМП после СМЭ за счет того, что устраняются ключевые параметры расчета, такие как ГД в ВТЛЖ, толщина МЖП, происходит ремоделирование ЛЖ и т.п. Тем не менее требуется дальнейшая оценка рисков ВСС после хирургического лечения с целью определения показаний к ИКД.
Модель HCM Risk-SCD может быть использована для прогнозирования ВСС у пациентов, перенесших ЭСА [365].
- У пациентов с ГКМП, перенесших остановку сердца по причине ЖТ или ФЖ, или при наличии эпизодов спонтанной устойчивой ЖТ, приводящей к потере сознания или нарушениям гемодинамики, при ожидаемой продолжительности жизни >1 года рекомендуется установка ИКД*** [3][129][136][137][322][323][488].
ЕОК IB (УДД 5, УУР С)
Комментарии. Для верификации аритмии в отдельных случаях может выполняться инвазивное электрофизиологическое исследование.
- У пациентов с ГКМП пятилетний риск внезапной смерти рекомендуется оценивать при первоначальном обследовании пациента, а также каждые 1-2 года или при изменении клинического статуса [3][129][137][240][365][366].
ЕОК IС (УДД 4, УУР С)
- Рекомендуется выполнение установки ИКД*** у пациентов ГКМП с предполагаемым 5-летним риском внезапной смерти ≥6% и ожидаемой продолжительностью жизни >1 года после подробного клинического обследования с оценкой риска последующих осложнений и влияния ИКД*** на образ жизни, социально-экономический статус и психологическое здоровье [129][137][240][279][365].
ЕОК IIaB (УДД 3, УУР A)
- Рекомендуется выполнение установки ИКД*** с целью первичной профилактики ВСС пациентам ГКМП в возрасте 16 лет и старше с промежуточным 5-летним риском ВСС (≥4 — <6%) и:
(а) значительным ПНГ при МРТ (≥15% массы ЛЖ); или
(b) ФВ ЛЖ <50%; или
(c) аневризмой верхушки ЛЖ [2][129][137][489].
ЕОК IIаB (УДД 4, УУР С)
- Рекомендуется рассмотреть возможность установки ИКД*** с целью первичной профилактики ВСС при ГКМП пациентам в возрасте 16 лет и старше с предполагаемым 5-летним риском ВСС ≥4 — <6% без дополнительных факторов риска [137].
ЕОК IIbB (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность установки ИКД*** с целью первичной профилактики пациентам ГКМП в возрасте 16 лет и старше с низким расчетным 5-летним риском ВСС (<4%) и
(a) значительным процентом ПНГ при МРТ (≥15% массы ЛЖ); или
(b) ФВ ЛЖ <50%; или
(c) ЛЖ апикальной аневризмой [137].
ЕОК IIbB (УДД 5, УУР С)
- Рекомендуется рассмотреть возможность выполнения радиочастотной аблации аритмогенных зон в опытных центрах отдельным тщательно отобранным пациентам ГКМП и рецидивирующими, симптоматическими устойчивыми мономорфными пароксизмами ЖТ или частыми срабатываниями ИКД*** в связи с устойчивыми мономорфными пароксизмами ЖТ, при неэффективности антиаритмических препаратов, их непереносимости или наличии к ним противопоказаний [137].
ЕОК IIbС (УДД 5, УУР С)
3.2.4. Рекомендации по имплантации вспомогательных левожелудочковых устройств
- У некоторых пациентов ГКМП с терминальной стадией ХСН, которые являются кандидатами для трансплантации сердца, рекомендуется рассмотреть возможность имплантации устройств механической поддержки кровообращения на период нахождения в листе ожидания5 [274][315][490].
ЕОК IIbС (УДД 4, УУР С)
Комментарии. В мировой практике 50% операций по пересадке сердца выполняются на фоне предшествующей имплантации устройств механической поддержки кровообращения [316]. Но опыт использования устройств вспомогательного кровообращения у пациентов с ГКМП ограничен. В одном из систематических обзоров было установлено, что использование подобных систем у пациентов с ГКМП сопровождалось большим риском периоперационной и краткосрочной летальности, правожелудочковой недостаточности, инфекций, кровотечений, инсульта, почечной недостаточности и аритмии в сравнении с пациентами с дилатационной и ишемической КМП [491]. Тем не менее некоторые ретроспективные исследования продемонстрировали отсутствие разницы в исходах между этими когортами [492][493].
Пациенты с ГКМП традиционно считались не пригодными для имплантации устройств вспомогательного кровообращения из-за малой полости ЛЖ и относительно сохранной ФВ. Несколько серий случаев продемонстрировали, что использование устройств с непрерывным потоком сопровождается приемлемыми результатами, особенно у пациентов с большими размерами полости ЛЖ (>46-50 мм) [492][494].
3.2.5. Трансплантация сердца у пациентов с ГКМП
- У пациентов с ГКМП, имеющих ФВ ЛЖ <50% и симптомы ХСН II-IV ФК, или неустранимые желудочковые аритмии, несмотря на оптимальную терапию, рекомендуется выполнение ортотопической трансплантации сердца при наличии показаний и отсутствии противопоказаний для ее выполнения5 [1][154][155][190][316][318][320][495].
ЕОК IIaB (УДД 4, УУР С)
Комментарии. При 3-4 стадии ГКМП по Olivotto присоединяются дополнительные морфофункциональные фенотипы согласно классификации MOGE(s): дГКМП; дилатационная стадия ГКМП (ГКМП+ДКМП) или рГКМП [67].
Трансплантация сердца может быть жизненно важной стратегией лечения при ГКМП в конечной стадии заболевания.
Плохой краткосрочный прогноз у пациентов с дилатационной стадией ГКМП предполагает целесообразность более раннего рассмотрения агрессивных методов лечения, поскольку "окно возможностей" может быть небольшим, особенно у пациентов с семейным анамнезом развития дилатационной стадии ГКМП.
Развитие дилатации ЛЖ у больных ГКМП следует верифицировать на основании динамики размеров ЛЖ. Даже "нормальные" размеры ЛЖ могут означать "дилатационную стадию" при увеличении конечно-диастолического размера/КДО ЛЖ (при условии корректного измерения).
Посттрансплантационная выживаемость у пациентов с ГКМП сходна с таковой при трансплантации сердца вследствие других причин5 [318][320].
- У пациентов с ГКМП с ФВ ЛЖ ≥50% и симптомами ХСН III-IV ФК, вызванной диастолической дисфункцией, резистентной к лекарственной терапии, при высоком риске неблагоприятного исхода редукции МЖП или коррекции клапанной патологии, рекомендуется рассмотреть возможность выполнения ортотопической трансплантации сердца при наличии показаний и отсутствии противопоказаний5 [1][154][155][190][316][318][320][495].
ЕОК IIbС (УДД 4, УУР С)
Комментарии. Тяжелая ХСН с сохраненной ФВ ЛЖ может наблюдаться при ГКМП с рестриктивным фенотипом согласно классификации MOGE(s).
Итоговый алгоритм врачебной тактики в зависимости от стадии ГКМП и варианта клинического течения представлен в Приложении Б9.
3.2.6. Тактика ведения беременности при ГКМП
- При беременности пациенткам с ГКМП рекомендуется проведение стратификации материнского риска, используя модифицированную классификацию Всемирной организации здравоохранения (ВОЗ) материнских сердечно-сосудистых осложнений [496-500].
ЕОК IС (УДД 5, УУР С)
Комментарии. В идеале оценка риска должна проводиться до зачатия. Беременные с ГКМП согласно модифицированной классификации материнских сердечно-сосудистых осложнений классифицируются во II-III ФК ВОЗ, однако, согласно данной классификации, пациентки не разделяются в зависимости от наличия или отсутствия обструкции ВТЛЖ, что является существенным недостатком данной классификации. Симптомные пациентки с обструктивной формой ГКМП и ГД >100 мм рт.ст. в ВТЛЖ могут быть соотнесены по гемодинамике и возможным осложнениям во время беременности и родов с пациентками с тяжелым симптомным АС, относящимся к IV классу ФК ВОЗ и требующие оперативного лечения основного заболевания перед планированием беременности. Согласно приказу № 736 от 03.12.2007: ГКМП с выраженной обструкцией ВТЛЖ, ВТПЖ или обоих желудочков и ГКМП без обструкции ВТЛЖ со сложными нарушениями сердечного ритма являются показаниями к прерыванию беременности на любом сроке беременности.
- Пациенткам с ГКМП с ГД в ВТЛЖ >50 мм рт.ст. и ГКМП без обструкции ВТЛЖ со сложными нарушениями сердечного ритма рекомендуется проведение мультидисциплинарного консилиума о возможности планирования беременности и/или пролонгирования беременности6.
ЕОК нет/РКО IC (УДД 5, УУР C)
- Осмотр пациенток с обструктивной формой ГКМП или сложными нарушениями ритма сердца во время беременности рекомендуется проводить не менее 1 раза в мес. врачом-терапевтом и/или врачом-кардиологом для своевременного выявления осложнений течения беременности со стороны сердечно-сосудистой системы [496][500][501].
ЕОК нет/РКО IC (УДД 5, УУР C)
- Осмотр пациенток с ГКМП без обструкции ВТЛЖ и без сложных нарушений ритма сердца во время беременности рекомендуется проводить не менее 1 раза в 2 мес. врачом-терапевтом и/или врачом-кардиологом, для своевременного выявления осложнений течения беременности со стороны сердечно-сосудистой системы [500][501].
ЕОК нет/РКО IC (УДД 5, УУР C)
Комментарии. Во время осмотра обязательна оценка появления новых симптомов, оценка ЧСС, оценка эффективности проводимой терапии в случае ее наличия.
- У пациенток с ОГКМП рекомендуется рассмотреть возможность продолжения терапии бета-адреноблокаторами, если они принимали их до беременности [496][498-500][502].
ЕОК IIаС (УДД 3, УУР С)
- Терапию бета-адреноблокатором рекомендовано начать беременной женщине с ГКМП и симптомами обструкции ВТЛЖ или нарушениями ритма сердца [496][498-500][502].
ЕОК IIaС (УДД 5, УУР С)
- При терапии бета-адреноблокатором рекомендовано контролировать состояние и темп роста плода [496-500][502][503].
ЕОК IС (УДД 5, УУР С)
- При непереносимости бета-адреноблокаторов у беременной женщины с ГКМП и симптомами обструкции ВТЛЖ или нарушениями ритма сердца рекомендуется назначение препарата второй линии — верапамила** [3][496][500][504].
ЕОК нет/РКО IС (УДД 5, УУР С)
- Беременным с ГКМП при развитии ФП рекомендовано выполнение кардиоверсии с оптимальной защитой от облучения [145][146][497][500][505][506].
ЕОК IIaС (УДД 4, УУР С)
- Беременным с ГКМП и ФП для профилактики тромбоэмболических осложнений рекомендована антикоагулянтная терапия [146][496][498][500][502][504][506].
ЕОК IС (УДД 5, УУР С)
Комментарии. Рекомендуемые режимы антикоагулянтной терапии при ГКМП у беременных с ФП и опасности, связанные с терапией варфарином**, представлены в таблице 22 (Приложение А3). Выбор препарата — гепарин** (низкомолекулярный 2 раза в день с дозировкой рассчитанной по весу) или варфарин** — возможен со 2 триместра беременности до 36-37 нед., с поддержанием целевого МНО 2-3 [146].
- Назначение дабигатрана этексилата** или ривароксабана**, или апиксабана** не рекомендуется во время беременности [146][496][498][500][502][506].
ЕОК IIIC (УДД 5, УУР С)
- Рекомендовано рассмотреть возможность терапии варфарином** при ФП у беременных со 2 триместра и с обязательной заменой на низкомолекулярный гепарин с 36-37 нед. беременности [146][496][498-500][506].
ЕОК IB (УДД 5, УУР С)
- Беременным с ГКМП без тяжелой обструкции, в случае приема ПОАК с заменой варфарина** на низкомолекулярный гепарин перед родами (МНО <1,5) и без тяжелой ХСН рекомендовано родоразрешение через естественные родовые пути [496][498][500][503][505].
ЕОК IС (УДД 5, УУР С)
Комментарии. Врачебная тактика ведения беременности и родоразрешения представлена в Приложении Б12.
Выбор медицинского учреждения для ведения беременных и родоразрешения представлен в Приложении Б13.
Ограничения в выборе методов диагностики у беременных представлены в таблице 23 (Приложение А3).
При ведении беременности и родов интересы матери должны доминировать.
Большинство женщин с неосложненной ГКМП относятся по модифицированной классификации ВОЗ материнского риска к классу II (ВОЗ II). Часть симптомных пациенток относится к ВОЗ III; они должны наблюдаться в специализированных учреждениях (см. табл. 23). Женщины с ГКМП, осложненной ХСН и дисфункцией ЛЖ (дилатационная стадия или присоединение рестриктивного фенотипа), относятся к классу IV материнского риска, и им беременность противопоказана. При выраженной симптомной обструкции ВТЛЖ (также относятся к классу IV ВОЗ) беременность может стать возможной после предварительной коррекции обструкции ВТЛЖ.
Терапию бета-адреноблокатором (метопролол**, резервный — бисопролол**) беременным с ГКМП необходимо осуществлять под контролем ЧСС и АД, т.к. чрезмерное снижение АД может привести к уменьшению маточно-плацентарного кровотока и задержке внутриутробного развития плода [3][20][496].
Контрацепция у женщин с бессимптомной или малосимптомной ГКМП не имеет каких-либо особенностей по сравнению со здоровыми.
Если ГКМП осложнилась ХСН и ФП, то следует с осторожностью использовать пероральные контрацептивы из-за риска тромбоэмболий; возможно их использование при адекватной антикоагулянтной терапии [3][20][496][500][503].
- Имплантацию ИКД*** для профилактики ВСС у женщин с высоким риском ВСС рекомендуется выполнять перед планированием беременности [129][137][240][279][365][500].
ЕОК нет/РКО IIaB (УДД 4, УУР С)
- Рекомендуется оценивать необходимость установки ИКД*** для профилактики ВСС во время беременности по европейской шкале (HCM Risk-SCD) [129][137][240][279][365][500][507].
ЕОК нет/РКО IIaB (УДД 4, УУР С)
- Рекомендуется выполнение установки ИКД*** во время беременности при высоких рисках ВСС с учетом оптимальных сроков беременности после 8 нед. с оптимальной защитой от облучения [129][137][240][279][365][500][507].
ЕОК нет/РКО IIaB (УДД 4, УУР С)
4. Медицинская реабилитация, медицинские показания и противопоказания к применению методов реабилитации
Специальных рекомендаций по реабилитации пациентов с ГКМП не существует. После хирургического или эндоваскулярного вмешательства пациентам с ГКМП проводятся такие же реабилитационные мероприятия, как и пациентам с другой сердечно-сосудистой патологией, перенесшим хирургические или эндоваскулярные вмешательства.
5. Профилактика и диспансерное наблюдение, медицинские показания и противопоказания к применению методов профилактики
Профилактики ГКМП как заболевания не существует.
Профилактические мероприятия у пациентов с ГКМП заключаются в профилактике основных осложнений заболевания, которые представлены в таблице 24, Приложение А3.
Общие рекомендации по образу жизни пациенту с ГКМП представлены в Приложении В.
Диспансерное наблюдение пациентов с ГКМП
Пациенты с ГКМП нуждаются в пожизненном наблюдении для выявления изменений в симптоматике и предупреждения осложнений.
На начальном этапе медикаментозного лечения плановые повторные визиты к врачу желательно проводить через 6, 9, 12 мес. (при необходимости чаще) для оценки переносимости, эффективности и безопасности лечения, а также контроля выполнения врачебных рекомендаций. При недостаточной эффективности и плохой переносимости проводимого медикаментозного лечения рекомендована замена используемого лекарственного препарата с последующим контролем проводимого лечения.
- Всем пациентам с ГКМП, включая носителей патологических мутаций без фенотипических проявлений болезни и пациентов с бессимптомным течением заболевания, рекомендовано динамическое наблюдение (врач-терапевт, врач общей практики), в ходе которого оценивается характер и выраженность клинических, морфологических и гемодинамических нарушений и определяется лечебная стратегия [3][20][130][382][508-511].
ЕОК IB (УДД 5, УУР С)
- У клинически стабильных пациентов рекомендуются повторные ТТ-ЭхоКГ каждые 1-2 года [3][20][130][157][230][243][275][279][382][508-511].
ЕОК IС (УДД 5, УУР С)
- Повторные ЭхоКГ-исследования рекомендуются пациентам с ГКМП с изменениями в клиническом статусе или появлением новых сердечно-сосудистых проявлений [3][20][130][157][230][243][275][279][382][508-511].
ЕОК IB (УДД 5, УУР С)
- 48-часовое ХМ сердечного ритма рекомендуется каждые 12-24 мес. клинически стабильным пациентам, каждые 6-12 мес. пациентам с синусовым ритмом и размером ЛП ≥45 мм или при появлении новых жалоб на сердцебиение [3][20][127][240][243][370][512].
ЕОК IС (УДД 5, УУР С)
- Рекомендовано рассмотреть возможность проведения нагрузочного тестирования каждые 2-3 года для клинически стабильных пациентов и каждый год — при прогрессировании симптомов [3][20][272][275][333].
ЕОК IIbС (УДД 5, УУР C)
- Рекомендовано рассмотреть возможность проведения МРТ сердца каждые 5 лет для клинически стабильных пациентов и каждые 2-3 года — пациентам с прогрессированием заболевания [3][275][513].
ЕОК IIbС (УДД 5, УУР С)
- Полное обследование, включающее ЭКГ и ТТ-ЭхоКГ и ХМ сердечного ритма, рекомендуется в течение 1-3 мес. и 6-12 мес. после проведения редукции МЖП [3][225].
ЕОК IC (УДД 5, УУР С)
Комментарии. Неотъемлемой частью мероприятий при лечении и динамическом наблюдении за пациентами с ГКМП должно быть повышение их образовательного уровня. Если даже врач разработает оптимальную программу лечения для каждого конкретного пациента, провести ее в жизнь будет весьма сложно при наличии низкой мотивации к лечению. Все применяемые методы лечения и профилактики должны быть обсуждены и согласованы с пациентом. При выборе режима назначения препарата необходимо учитывать образ жизни пациента. Все рекомендации, даваемые пациенту, должны быть ясными, четкими и соответствовать его интеллектуальному уровню.
Для некоторых пациентов, которым устных рекомендаций недостаточно, следует рассмотреть возможность продублировать их в письменном виде для обеспечения осознанного участия пациента в лечебно-профилактическом процессе и повышения эффективности лечения [3][20].
6. Организация медицинской помощи
- Пациентам с неочевидным диагнозом, тяжелыми симптомами или повышенным риском связанных с заболеванием осложнений рекомендуется рассмотреть возможность обследования и лечения у специалистов мультидисциплинарной команды, экспертов в ведении ГКМП [1][3][20][34][42][67][184][429][514-516].
ЕОК IIbС (УДД 5, УУР C)
- Независимо от выраженности симптомов рекомендуется регулярное обследование пациентов и, при возможности, родственников первой степени родства [1][3][20][21][33][57][130][157][217][230][243][279][382][433][508][509][511].
ЕОК IС (УДД 5, УУР С)
- Всем пациентам с ГКМП рекомендуется обследование и лечение в центрах с мультидисциплинарной командой специалистов, с опытом диагностики и лечения заболеваний миокарда [1][3][20][34][42][52][67][184][429][514-516].
ЕОК IIaС (УДД 5, УУР С)
Показания к плановой госпитализации:
— Уточнение причины ГЛЖ неясного генеза и необходимость в специальных методах исследования (исключение фенокопий ГКМП);
— Использование диагностических процедур, проведение которых невозможно или нецелесообразно в условиях поликлиники;
— Трудности в подборе медикаментозной терапии для коррекции синдромов (из-за сочетания патологий ГКМП/ОГКМП + АГ, ГКМП + сахарный диабет 2 типа, синдром стенокардии);
— Назначение бета-адреноблокаторов, верапамила** рекомендуется начинать в условиях стационара с малых доз, проводить титрование до максимально переносимых доз под контролем самочувствия и ЭКГ;
— Рефрактерность к проводимой в полном объеме фармакотерапии и наличие показаний к СМЭ, ЭСА, ЭКС.
Показания к экстренной госпитализации:
— Прогрессия ХСН, требующая интенсивной терапии;
— Отек легких;
— Инсульт;
— Опасные для жизни нарушения сердечного ритма и проводимости, требующие интенсивной терапии;
— Синкопальные состояния;
— ОКС;
— Предотвращенная ВСС.
Показания к выписке пациента из стационара:
— При плановой госпитализации показанием к выписке пациента с ГКМП является улучшение клинической симптоматики на фоне проводимой фармакотерапии, имплантации ИКД***, ЭКС***/двухкамерного ЭКС***, эндоваскулярного/хирургического лечения (СМЭ, ЭСА);
— При экстренной госпитализации показанием к выписке пациента с ГКМП является коррекция нарушений ритма и проводимости, в т.ч. фатальных, отсутствие осложнений, требующих интенсивной терапии, и стабилизация ХСН;
— Нормализация показателей (целевые уровни АД, гликемии, липидограммы) при, соответственно, АГ, сахарном диабете 1 или 2 типа, дислипидемии, если ухудшение в течение этих заболеваний явилось основанием для плановой или экстренной госпитализации пациентов с ГКМП в сочетании с коморбидной патологией;
— При синдроме стенокардии показанием для выписки пациента с ГКМП является достижение стабилизации состояния пациента с ГКМП на фоне фармакотерапии, эндоваскулярного/хирургического лечения;
— Установление диагноза фенокопий ГКМП, выписка/перевод пациента в специализированные отделения для этиопатогенетического лечения (например, в гематологическое отделение при AL-амилоидозе с изолированным/преимущественным поражением сердца).
Иные организационные технологии
Целесообразно создание территориальных регистров пациентов с ГКМП.
При анализе работы лечебно-профилактического учреждения с пациентами с ГКМП целесообразно оценивать следующие показатели:
— соотношение ГКМП и фенокопий ГКМП, этиологический спектр фенокопий ГКМП;
— соотношение обструктивных и необструктивных форм ГКМП;
— соотношение семейных и спорадических случаев заболевания;
— частоту госпитализаций в связи с прогрессированием ХСН, ФП, ОКС, случаи ВСС;
— потребность в ЭКГ, ЭхоКГ, МРТ, КТ, КАГ для выполнения рекомендаций по динамическому наблюдению и обследованию пробанда и родственников пациентов первой линии родства;
— смертность (%), осложнения (%) за год, 3 года, 5 лет;
— частоту выявления факторов кардиометаболического риска (АГ, дислипидемия, ожирение/избыточный вес, сахарный диабет 1 и 2 типа) в разных возрастных группах ГКМП [52];
— результаты мониторирования потенциально модифицируемых факторов: антропометрических данных (индекс массы тела, окружность талии), показателей липидного профиля, уровня гликемии в разных возрастных группах пациентов.
7. Дополнительная информация (в том числе факторы, влияющие на исход заболевания или состояния)
Другими важными целями при лечении ГКМП являются:
- Коррекция всех потенциально модифицируемых факторов риска (курение, дислипидемия, гипергликемия, ожирение);
- Лечение сопутствующих заболеваний в соответствии с национальными клиническими рекомендациями (ИБС, АГ, сахарный диабет, хроническая болезнь почек).
Критерии оценки качества первичной медико-санитарной помощи взрослым при ГКМП
|
№ п/п |
Критерий качества |
Оценка выполнения |
|
1 |
Выполнен анализ крови биохимический общетерапевтический (калий, аланинаминотрансфераза, аспартатаминотрансфераза, креатинин, глюкоза) при первичном обращении и динамическом наблюдении не реже 1 раза в 12 мес. |
Да/Нет |
|
2 |
Выполнена регистрация электрокардиограммы при первичном обращении и динамическом наблюдении не реже 1 раза в 12 мес. |
Да/Нет |
|
3 |
Выполнена эхокардиография при первичном обращении и динамическом наблюдении не реже 1 раза в 12 мес. |
Да/Нет |
|
4 |
Выполнено холтеровское мониторирование сердечного ритма при первичном обращении и динамическом наблюдении не реже 1 раза в 12 мес. |
Да/Нет |
|
5 |
Выполнена стратификация материнского риска с использованием модифицированной классификации Всемирной организации здравоохранения материнского риска беременным пациенткам |
Да/Нет |
|
6 |
Выполнена стратификация риска по шкале HCM Risk-SCD, по результатам стратификации при наличии медицинских показаний к имплантации имплантируемого кардиовертера-дефибриллятора выполнена консультация (направлен на консультацию) врача-кардиолога и/или врача-сердечно-сосудистого хирурга |
Да/Нет |
|
7 |
Назначено лечение бета-адреноблокаторами или недигидропиридиновыми блокаторами "медленных" кальциевых каналов (селективные блокаторы кальциевых каналов с прямым действием на сердце) и/или ингибиторами ангиотензинпревращающего фермента или антагонистами рецепторов ангиотензина II или диуретиками (при отсутствии медицинских противопоказаний) |
Да/Нет |
|
8 |
Выполнено лечение бета-адреноблокаторами или блокаторами кальциевых каналов и/или ингибиторами ангиотензинпревращающего фермента или антагонистами рецепторов ангиотензина II или диуретиками (при отсутствии медицинских противопоказаний) |
Да/Нет |
|
9 |
Выполнена постановка пациента на диспансерное наблюдение |
Да/Нет |
Критерии оценки качества специализированной медицинской помощи взрослым при ГКМП
|
№ п/п |
Критерий качества |
Оценка выполнения |
|
1 |
Выполнены ЭКГ и ТТ-ЭхоКГ |
Да/Нет |
|
2 |
Выполнено МРТ сердца с контрастированием, КТ сердца с контрастированием при наличии медицинских показаний и при отсутствии противопоказаний |
Да/Нет |
|
3 |
Выполнено ХМ сердечного ритма |
Да/Нет |
|
4 |
Выполнены анализы: общий (клинический) анализ крови и общий анализ мочи, анализ крови биохимический общетерапевтический (включая холестерин, триглицериды, калий, натрий, аспартатаминотрансферазу, аланинаминотрансферазу, мочевину, креатинин, билирубин, глюкозу) |
Да/Нет |
|
5 |
Проведена стратификация риска у пациентов с ГКМП со средним и низким риском ВСС, а также у пациентов с ОГКМП, перенесших СМЭ (американская модель, европейская модель, шкала HCM Risk-SCD) В зависимости от медицинских показаний и при отсутствии медицинских противопоказаний выполнена МРТ с контрастированием гадолинием. Определены показания к ИКД*** в зависимости от медицинских показаний и при отсутствии медицинских противопоказаний |
Да/Нет |
|
6 |
Проведена стратификация риска у пациентов с ГКМП и высоким риском ВСС, а также у пациентов с ОГКМП, перенесших ЭСА (европейская модель, шкала HCM Risk-SCD) Определены показания к ИКД*** в зависимости от медицинских показаний и при отсутствии медицинских противопоказаний |
Да/Нет |
|
7 |
Проведена терапия бета-адреноблокатором, или недигидропиридиновым блокатором "медленных" кальциевых каналов (селективные блокаторы кальциевых каналов с прямым действием на сердце) в режиме монотерапии или в режиме комбинированной терапии (сочетание с иАПФ, или блокаторами рецепторов ангиотензина II, и/или диуретиками) в зависимости от медицинских показаний и при отсутствии медицинских противопоказаний |
Да/Нет |
|
8 |
Выполнена консультация врача-генетика беременной с ГКМП или при планировании беременности |
Да/Нет |
|
9 |
Пациент с ГКМП находится под диспансерным наблюдением в поликлинике |
Да/Нет |
Сокращения: ВСС — внезапная сердечная смерть, ГКМП — гипертрофическая кардиомиопатия, иАПФ — ингибиторы ангиотензинпревращающего фермента, ИКД — имплантируемый кардиовертер-дефибриллятор, КТ — компьютерная томография, МРТ — магнитно-резонансная томография, ОГКМП — обструктивная гипертрофическая кардиомиопатия, СМЭ — септальная миоэктомия, ТТ-ЭхоКГ — трансторакальная эхокардиография, ХМ — холтеровское мониторирование сердечного ритма, ЭКГ — электрокардиография, ЭСА — этаноловая септальная аблация.
1. Hypertrophic Cardiomyopathy Gene Curation Expert Panel — ClinGen | Clinical Genome Resource. https://clinicalgenome.org/affiliation/40008/.
2. European Reference Networks in the Field of Rare Diseases: State of the Art and Future Directions. Third Report. http://www.eucerd.eu/?post_type=document&p=1204.
3. Профстандарт 02.054 | Врач-генетик | Профессиональные стандарты 2023. https://classinform.ru/profstandarty/02.054-vrach-genetik.html.
4. European Medicines Agency recommends measures to reduce risk of heart problems with Corlentor/Procoralan (ivabradine) | European Medicines Agency. https://www.ema.europa.eu/en/news/european-medicines-agency-recommends-measures-reduce-risk-heart-problems-corlentorprocoralan.
5. Бельских Л.В., Гичкун О.Е., Гордеев М.Л. и др. Трансплантация сердца и механическая поддержка кровообращения. Национальные клинические рекомендации. 2016.
6. Приказ Министерства здравоохранения и социального развития РФ от 03.12.2007 № 736 “Об утверждении перечня медицинских показаний для искусственного прерывания беременности” (в ред. приказа Минздравсоцразвития России от 27 декабря 2011 г. № 1661н).
Приложение А1. Состав Рабочей группы по разработке и пересмотру клинических рекомендаций
Президиум Рабочей группы
- Бокерия Л. А., академик РАН, д.м.н., профессор (Москва), Ассоциация сердечно-сосудистых хирургов
- Шляхто Е. В., академик РАН, д.м.н., профессор (Санкт-Петербург), Российское кардиологическое общество
- Габрусенко С. А., д.м.н., профессор (Москва), Российское кардиологическое общество
- Гудкова А. Я., д.м.н. (Санкт-Петербург), Российское кардиологическое общество
- Козиолова Н. А., д.м.н., профессор (Пермь), Российское кардиологическое общество
Другие члены Рабочей группы
- Александрова С. А., к.м.н. (Москва), Ассоциация сердечно-сосудистых хирургов
- Алехин М. Н., д.м.н., профессор (Москва), Российское кардиологическое общество
- Афанасьев А. В., д.м.н. (Новосибирск), Ассоциация сердечно-сосудистых хирургов
- Богатырева М. М-Б., к.м.н., доцент (Магас)
- Богачев-Прокофьев А. В., д.м.н. (Новосибирск), Ассоциация сердечно-сосудистых хирургов
- Богданов Д. В., д.м.н., профессор (Челябинск), Российское кардиологическое общество
- Берсенева М. И., к.м.н., доцент (Москва), Российское кардиологическое общество
- Гордеев М. Л., д.м.н., профессор (Санкт-Петербург), Ассоциация сердечно-сосудистых хирургов
- Дземeшкевич С. Л., д.м.н., профессор (Москва), Ассоциация сердечно-сосудистых хирургов
- Евтушенко А. В., д.м.н. (Кемерово), Ассоциация сердечно-сосудистых хирургов
- Заклязьминская Е. В., д.м.н. (Москва), Российское общество медицинских генетиков
- Зенченко Д. И., к.м.н. (Волгоград), Российское кардиологическое общество
- Иртюга О. Б., д.м.н., доцент (Санкт-Петербург), Российское кардиологическое общество
- Каплунова В. Ю., д.м.н. (Москва), Российское кардиологическое общество
- Каштанов М. Г., к.м.н. (Екатеринбург), Ассоциация сердечно-сосудистых хирургов
- Костарева А. А., д.м.н., профессор (Санкт-Петербург), Российское кардиологическое общество, Российское общество медицинских генетиков
- Крутиков А. Н., к.м.н. (Санкт-Петербург), Российское кардиологическое общество
- Маленков Д. А. (Москва), Ассоциация сердечно-сосудистых хирургов
- Новикова Т. Н., д.м.н., доцент (Санкт-Петербург), Российское кардиологическое общество
- Рудь С. Д., к.м.н., доцент (Санкт-Петербург), Российское кардиологическое общество
- Рыбка М. М., д.м.н., профессор (Москва), Ассоциация сердечно-сосудистых хирургов
- Саидова М. А., д.м.н., профессор (Москва), Российское кардиологическое общество
- Стрельцова А. А. (Санкт-Петербург), Российское кардиологическое общество
- Стукалова О. В., к.м.н., доцент (Москва), Российское кардиологическое общество
- Чмелевский М. П. (Санкт-Петербург), Российское кардиологическое общество
- Шапошник И. И., д.м.н., профессор (Челябинск), Российское кардиологическое общество
- Шлойдо Е. А., к.м.н. (Санкт-Петербург), Ассоциация сердечно-сосудистых хирургов
Члены Рабочей группы подтвердили отсутствие финансовой поддержки/конфликта интересов. В случае сообщения о наличии конфликта интересов член(ы) Рабочей группы был(и) исключен(ы) из обсуждения разделов, связанных с областью конфликта интересов.
Приложение А2. Методология разработки клинических рекомендаций
Вследствие того, что Российское кардиологическое общество (РКО) входит в состав Европейского общества кардиологов (ЕОК), и члены РКО также являются членами ЕОК, все европейские рекомендации формируются с участием российских экспертов, которые являются соавторами рекомендаций. Таким образом, существующие рекомендации ЕОК отражают общее мнение ведущих российских и европейских кардиологов.
В связи с этим формирование национальных рекомендаций проводилось на основе рекомендаций ЕОК с учетом национальной специфики, особенностей обследования, лечения, доступности той или иной медицинской помощи. По этой причине в ходе разработки российских клинических рекомендаций РКО использованы международные классы показаний рекомендаций, позволяющие оценить необходимость выполнения тезиса рекомендаций и уровни достоверности доказательств данных классов (табл. 1/А2 и 2/А2).
В тех случаях, когда в европейских рекомендациях отсутствовали классы и уровни доказательности, но по мнению экспертов РКО данные тезисы являлись крайне необходимыми для выполнения или, наоборот, абсолютно не рекомендованы к применению, эксперты РКО, основываясь на правилах формирования классов показаний согласно рекомендациям Европейского общества кардиологов, сами проставляли классы и уровни. В данной ситуации обозначение ЕОК заменено на РКО — классы и уровни, проставленные экспертами РКО.
Кроме того, добавлена новая система шкал УДД и УУР для лечебных, реабилитационных, профилактических вмешательств и диагностических вмешательств (табл. 3/А2, 4/А2 и 5/А2), введенная в 2018г ФГБУ ЦЭККМП Минздрава РФ. Таким образом, в тексте клинических рекомендаций, разрабатываемых экспертами РКО, одновременно использованы две шкалы (табл. 1/А2, 2/А2, 3/А2, 4/А2, 5/А2).
Представленные Рекомендации разработаны на основе Российских рекомендаций по диагностике и лечению ГКМП 2016г, рекомендаций по диагностике и лечению ГКМП Европейского общества кардиологов 2014г, созданных на основе многолетнего опыта и большого количества исследований по различным аспектам диагностики и лечения ГКМП. В Рекомендациях изложены основные аспекты патогенеза, клинического течения, методы диагностики и принципы лечения пациентов с ГКМП с учетом индивидуальных особенностей пациента.
Целевая аудитория данных клинических рекомендаций
- Врач-кардиолог.
- Врач-терапевт.
- Врач общей практики.
- Врач сердечно-сосудистый хирург.
- Врач функциональной диагностики.
- Врач рентгенолог.
- Врач ультразвуковой диагностики.
- Врач радиолог.
- Врач-генетик.
Таблица 1/А2
Классы показаний согласно рекомендациям ЕОК
|
Класс рекомендаций |
Определение |
Предлагаемая формулировка |
|
I |
Доказано или общепризнанно, что диагностическая процедура, вмешательство/лечение являются эффективными и полезными |
Рекомендовано/показано |
|
II
IIa
IIb |
Противоречивые данные и/или мнения об эффективности/пользе диагностической процедуры, вмешательства, лечения Большинство данных/мнений в пользу эффективности/пользы диагностической процедуры, вмешательства, лечения Эффективность/польза диагностической процедуры, вмешательства, лечения установлены менее убедительно |
Целесообразно применять
Можно применять |
|
III |
Данные или единое мнение, что диагностическая процедура, вмешательство, лечение бесполезны/неэффективны, а в ряде случаев могут приносить вред |
Не рекомендуется применять |
Таблица 2/А2
УДД согласно рекомендациям ЕОК
|
Уровни достоверности доказательств |
|
|
A |
Данные многочисленных рандомизированных клинических исследований или метаанализов |
|
B |
Данные получены по результатам одного рандомизированного клинического исследования или крупных нерандомизированных исследований |
|
C |
Согласованное мнение экспертов и/или результаты небольших исследований, ретроспективных исследований, регистров |
Таблица 3/А2
Шкала оценки УДД для методов диагностики (диагностических вмешательств)
|
УДД |
Расшифровка |
|
1 |
Систематические обзоры исследований с контролем референсным методом или систематический обзор рандомизированных клинических исследований с применением метаанализа |
|
2 |
Отдельные исследования с контролем референсным методом или отдельные рандомизированные клинические исследования и систематические обзоры исследований любого дизайна, за исключением рандомизированных клинических исследований, с применением метаанализа |
|
3 |
Исследования без последовательного контроля референсным методом или исследования с референсным методом, не являющимся независимым от исследуемого метода или нерандомизированные сравнительные исследования, в т.ч. когортные исследования |
|
4 |
Несравнительные исследования, описание клинического случая |
|
5 |
Имеется лишь обоснование механизма действия или мнение экспертов |
Сокращение: УДД — уровни достоверности доказательств.
Таблица 4/А2
Шкала оценки УДД для методов профилактики, лечения и реабилитации (профилактических, лечебных, реабилитационных вмешательств)
|
УДД |
Расшифровка |
|
1 |
Систематический обзор РКИ с применением метаанализа |
|
2 |
Отдельные РКИ и систематические обзоры исследований любого дизайна, за исключением РКИ, с применением метаанализа |
|
3 |
Нерандомизированные сравнительные исследования, в т.ч. когортные исследования |
|
4 |
Несравнительные исследования, описание клинического случая или серии случаев, исследования "случай-контроль" |
|
5 |
Имеется лишь обоснование механизма действия вмешательства (доклинические исследования) или мнение экспертов |
Сокращения: РКИ — рандомизированное клиническое исследование, УДД — уровни достоверности доказательств.
Таблица 5/А2
Шкала оценки УУР для методов профилактики, диагностики, лечения и реабилитации (профилактических, диагностических, лечебных, реабилитационных вмешательств)
|
УУР |
Расшифровка |
|
A |
Сильная рекомендация (все рассматриваемые критерии эффективности (исходы) являются важными, все исследования имеют высокое или удовлетворительное методологическое качество, их выводы по интересующим исходам являются согласованными) |
|
B |
Условная рекомендация (не все рассматриваемые критерии эффективности (исходы) являются важными, не все исследования имеют высокое или удовлетворительное методологическое качество и/или их выводы по интересующим исходам не являются согласованными) |
|
C |
Слабая рекомендация (отсутствие доказательств надлежащего качества: все рассматриваемые критерии эффективности (исходы) являются неважными, все исследования имеют низкое методологическое качество и их выводы по интересующим исходам не являются согласованными) |
Сокращение: УУР — уровни убедительности рекомендаций.
Порядок обновления клинических рекомендаций
Механизм обновления клинических рекомендаций предусматривает их систематическую актуализацию — не реже чем 1 раз в 3 года или при появлении новой информации о тактике ведения пациентов с данным заболеванием. Решение об обновлении принимает Минздрав России на основе предложений, представленных медицинскими некоммерческими профессиональными организациями. Сформированные предложения должны учитывать результаты комплексной оценки лекарственных препаратов, медицинских изделий, а также результаты клинической апробации новых методов лечения.
Приложение А3. Справочные материалы, включая соответствие показаний к применению и противопоказаний, способов применения и доз лекарственных препаратов, инструкции по применению лекарственного препарата
- Приказ Минздрава России от 15 ноября 2012г № 918н "Об утверждении Порядка оказания медицинской помощи больным с сердечно-сосудистыми заболеваниями".
- Приказ Минздрава России от 10 мая 2017г № 203н "Об утверждении критериев оценки качества медицинской помощи".
- Приказ Минздрава России от 15 июля 2016г № 520н "Об утверждении критериев оценки качества медицинской помощи".
- Приказ Минздрава России от 28.02.2019 № 103н "Об утверждении порядка и сроков разработки клинических рекомендаций, их пересмотра, типовой формы клинических рекомендаций и требований к их структуре, составу и научной обоснованности включаемой в клинические рекомендации информации" (Зарегистрирован 08.05.2019 № 54588).
Таблица 1/А3
Молекулярный патогенез специфических причин ГКМП (по ЕОК 2014) [3]
|
Нозология (фенокопия ГКМП) |
Молекулярный патогенез и возможности этиопатогенетическая терапии в Российской Федерации |
|
AL-амилоидоз |
При AL-амилоидозе клон малигнизированных плазматических клеток синтезирует в большом количестве легкие цепи (каппа или лямбда) иммуноглобулинов. Увеличение концентрации белка-предшественника выше некоторого порогового значения может автоматически приводить к началу фибриллогенеза и отложению амилоида в тканях. При этом в 5% случаев диагностируют преимущественное поражение сердца амилоидозом |
|
Ненаследственный и наследственный ATTR |
В основе молекулярного патогенеза ненаследственного и наследственного ATTR лежат конформационные изменения и дестабилизация тетрамера транстиретина. Дестабилизация транстиретина приводит к неправильному фолдингу белка и агрегации вариантных мономеров транстиретина с образованием токсичных промежуточных амилоидогенных продуктов и амилоидных фибрилл. Эти механизмы могут нарушаться с возрастом, что объясняет повышение риска развития немутантного ненаследственного ATTR у лиц пожилого и старческого возраста. Тафамидис рекомендуется пациентам с генетически подтвержденной ТТР амилоидной КМП и симптомами I или II класса по NYHA для уменьшения симптомов, числа госпитализаций в связи с сердечно-сосудистыми проявлениями и смертности. Тафамидис рекомендуется пациентам с приобретенной ТТР амилоидной КМП и симптомами I или II класса по NYHA для уменьшения симптомов, числа госпитализаций в связи с сердечно-сосудистыми проявлениями и смертности [154]. — МНН Тафамидис 20 мг — Активное вещество — тафамидис меглюмин — ATTR полиневропатия без кардиальных проявлений — МНН Тафамидис 61 мг — Активное вещество-тафамидис — ATTR кардиомиопатия независимо от других проявлений |
|
Болезнь Андерсона-Фабри |
Мутация в гене GLA (описано >400), кодирующем фермент á-галактозидазу А (á-Gal A), приводит к значительному снижению активности фермента, вовлеченного в метаболизм сфингогликолипидов [6]. Это приводит к накоплению негидролизованного субстрата блокированной ферментной реакции и сопровождается увеличением числа лизосом в клетках, нарушением нормального функционирования этих клеток и их гибелью. Разработана этиопатогенетическая терапия. В Российской Федерации зарегистрировано 2 препарата: Агалсидаза альфа и Агалсидаза бета |
|
Наследственные синдромы с ГКМП-фенотипом у подростков и молодых взрослых, связанные с мутациями в гене PRKAG2 |
PRKAG2 кодирует цАМФ-активируемую протеинкиназу-ã2. Данный белок определяет внутриклеточную аккумуляцию гликогена и нарушения его функции могут приводить к псевдогипертрофии кардиомиоцитов и задержке инволюции эмбриональных проводящих путей в миокарде. При этом наблюдается частое сочетание ГКМП-фенотипа и синдрома Вольфа- Паркинсона-Уайта |
|
Болезнь Данона |
Молекулярный механизм развития болезни Данона основан на дефекте в LAMP-2 белке, который опосредует накопление гликогена в кардиомиоцитах и приводит к псевдогипертрофии миокарда. Когда существует генетический обусловленный дефицит белка LAMP2. наблюдается неправильная аутофагическая деградация белков. Аутофагическая активность связана с патогенезом разнообразных болезней. Существует мнение, что болезнь Данона обусловлена наследственными нарушениями процесса аутофагии |
|
Атаксия Фридрейха |
Молекулярный патогенез атаксии Фридрейха до сих пор является предметом дискуссий. Однако на настоящий момент установлено участие белка фратаксина в поддержании гомеостаза железа в клетке и то, что его недостаточность приводит к множественному ферментному дефициту, митохондриальной дисфункции и окислительному повреждению |
|
RAS-патии (синдром Нунан и синдром LEOPARD) |
Мутации в генах, кодирующих компоненты и регуляторы RAS/MAPC сигнального пути (RAS/митоген-активируемая протеинкиназа) вызывают множественные наследственные пороки развития. RAS/MAPC сигнальный путь ответственен за пролиферацию, дифференцировку, старение и апоптоз клеток и обеспечивающей этим нормальное развитие клеток и тканей организма в целом в эмбриональном и постнатальном периодах |
Сокращения: ГКМП — гипертрофическая кардиомиопатия, КМП — кардиомиопатия, МНН — международное непатентованное название, ТТР — транстиреиновый, ATTR — транстиреиновый амилоидоз, NYHA — Нью-Йоркская ассоциация сердца.
Таблица 2/А3
Факторы риска развития ИМ 2 типа у пациентов с ГКМП
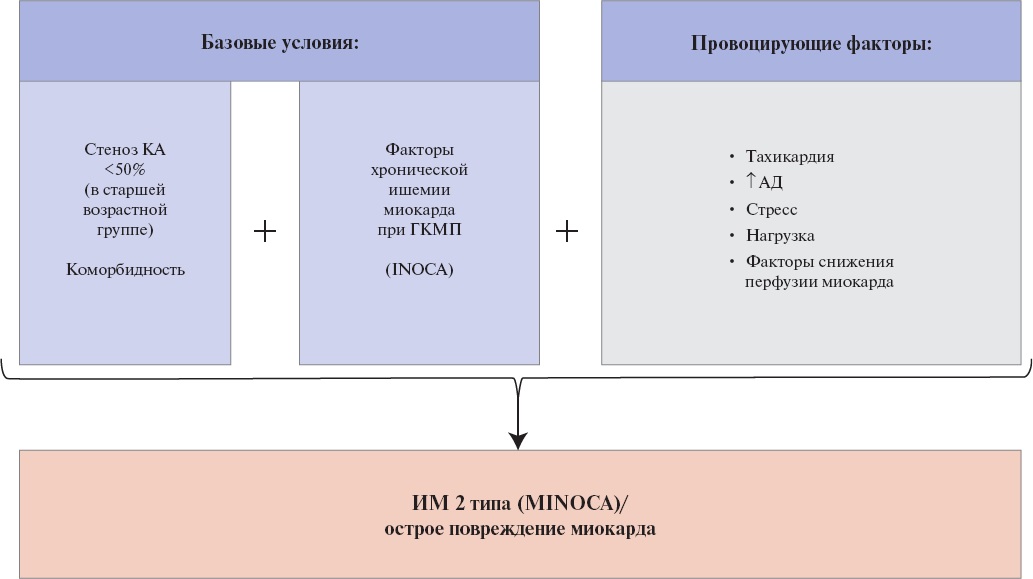
Сокращения: АД — артериальное давление, ГКМП — гипертрофическая кардиомиопатия, ИМ — инфаркт миокарда, КА — коронарная артерия, INOCA — ischemia with non-obstructive coronary arteries (ишемия без обструкции коронарных артерий), MINOCA — myocardial infarction with non-obstructive coronary arteries (инфаркт миокарда без обструкции коронарных артерий).
Таблица 3/А3
Клинические особенности наиболее часто встречающихся морфологических подтипов ГКМП (адаптировано из [87][179][517])
|
Характеристика |
Гипертрофия базальной части МЖП (субаортальная) |
Двояковыпуклая МЖП |
Верхушечная ГКМП |
Среднежелудочковая обструктивная ГКМП |
|
Обструкция |
Характерна обструкция ВТЛЖ |
Чаще отсутствие обструкции ВТЛЖ (может встречаться двухуровневая обструкция ЛЖ: на уровне ВТЛЖ и среднежелудочковая) и 2-желудочковая |
Отсутствие обструкции ВТЛЖ |
Среднежелудочковая обструкция ЛЖ (может встречаться двухуровневая обструкция ЛЖ: на уровне ВТЛЖ и среднежелудочковая) |
|
МРТ |
Менее выраженный фиброз |
Обширные области фиброза |
Менее выраженный фиброз |
Обширные области фиброза |
|
Генетика |
Чаще генотип (-) |
Чаще генотип (+) |
Чаще генотип (-) |
Чаще генотип (-) |
|
Характеристика ГКМП |
Чаще несемейная форма Многофакторное заболевание Дифференцированный диагноз с ТТР КМП |
Семейная ГКМП |
Чаще несемейная форма Многофакторное заболевание |
? |
|
Коморбидность |
— АГ — Повышенный ИМТ |
Менее характерна |
— АГ — Повышенный ИМТ — Дислипидемия |
? |
|
Наличие верхушечной аневризмы |
Отсутствует |
Отсутствует |
В 10-20% случаев |
Более чем в 20% случаев |
|
Особенности верхушечной ГКМП: Различают 2 формы верхушечной ГКМП: — изолированная верхушечная гипертрофия; — смешанный вариант (сочетание среднежелудочковой и верхушечной гипертрофии с преобладанием верхушечной) [518][519]. Верхушечная ГКМП имеет особый паттерн ЭКГ, который включает в себя: — наличие глубоких негативных зубцов T (≥1 mV (≥10 mm)); — вольтажные критерии ГЛЖ, инверсия волны Т; — выше частоту возникновения фибрилляции предсердий [520]. Дифференциальный диагноз верхушечной ГКМП необходимо проводить с: • болезнью Фабри (при болезни Фабри могут наблюдаться 4 морфологических фенотипа: 1) без утолщения стенок ЛЖ; 2) концентрическая ГЛЖ; 3) асимметричная ГЛЖ (гипертрофия МЖП); 4) преобладание верхушечной ГЛЖ) [521]. • "спортивным" сердцем [520]. • апикальным смещением папиллярных мышц. Клиническая оценка и двухмерная трансторакальная ЭхоКГ не могут в достаточной степени дифференцировать эти состояния, поэтому диагностика верхушечной ГКМП должна включать в себя контрастную ЭхоКГ или МРТ [522] |
||||
Сокращения: АГ — артериальная гипертензия, ВТЛЖ — выходной тракт левого желудочка, ГКМП — гипертрофическая кардиомиопатия, ГЛЖ — гипертрофия левого желудочка, ИМТ — индекс массы тела, КМП — кардиомиопатия, ЛЖ — левый желудочек, МЖП — межжелудочковая перегородка, МРТ — магнитно-резонансная томография, ТТР — транстиреиновый, ЭКГ — электрокардиография, ЭхоКГ — эхокардиография.
Таблица 4/А3
Упрощенная модель клинических вариантов течения ГКМП
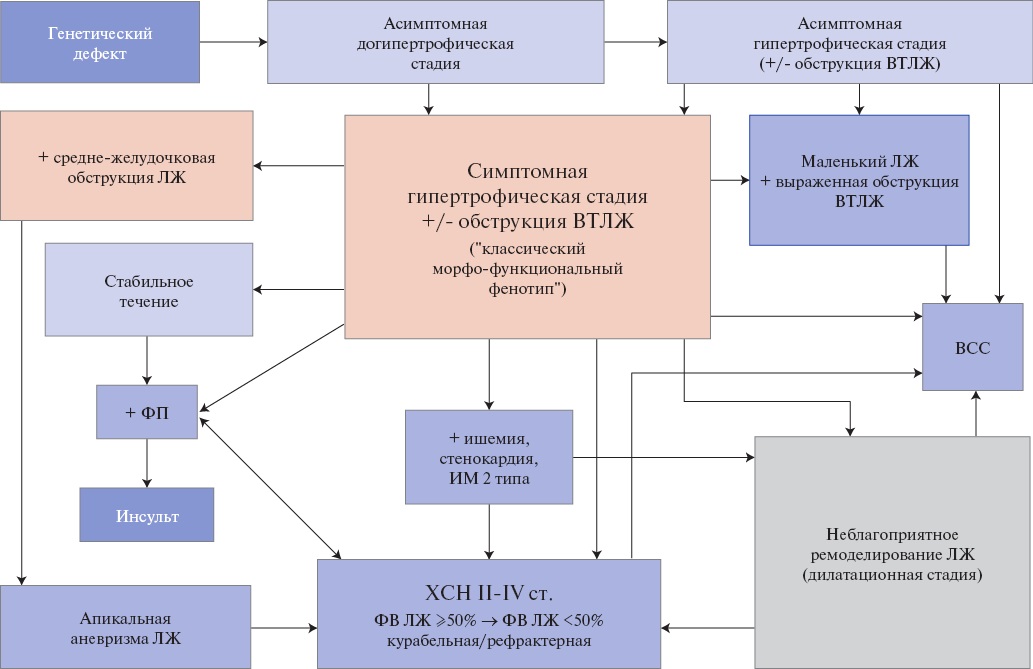
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГКМП — гипертрофическая кардиомиопатия, ИМ — инфаркт миокарда, ЛЖ — левый желудочек, ФВ — фракция выброса, ФП — фибрилляция предсердий, ХСН — хроническая сердечная недостаточность.
Таблица 5/А3
Изменения лабораторных тестов, позволяющие заподозрить некоторые фенокопии ГКМП (адаптировано из [3])
|
Тест |
Заболевания (фенокопии ГКМП) |
|
Гемоглобин |
При анемии усиливаются боли в грудной клетке и одышка, и ее следует исключать при изменении симптоматики. Анемия, вызывая тахикардию, может способствовать увеличению ГД в ВТЛЖ. Снижение кислород-транспортной функции крови может является дополнительным фактором ишемии миокарда |
|
Функция почек |
У пациентов с тяжелой левожелудочковой ХСН может быть нарушена функция почек. Снижение СКФ и протеинурия могут наблюдаться при амилоидозе, болезни Андерсона-Фабри и митохондриальных болезнях |
|
BNP и NT-proBNP |
Диагностика ХСН на ранней стадии. Мониторинг тяжести ХСН и ответа на терапию при фенокопиях ГКМП (например, кардиальном амилоидозе) |
|
Сердечный тропонин |
Повышен: — у пациентов с ГКМП, особенно при прогрессировании симптомов ГКМП, — при развитии ИМ 2 или 1 типа, — при некоторых фенокопиях ГКМП (например, кардиальном амилоидозе) |
|
Определение концентрации свободных легких цепей иммуноглобулинов (k и ë) в крови и моче |
При подозрении на AL-амилоидоз сердца |
|
Исследование костного мозга |
При подозрении на амилоидоз сердца |
|
Трансаминазы печени |
Печеночные тесты могут быть измененными при митохондриальных болезнях, болезни Данона |
|
Креатинфосфокиназа |
Креатинфосфокиназа плазмы возрастает при болезни Данона и митохондриальных болезнях, десминопатиях |
|
Активность á-галактозидазы А в плазме/лейкоцитах у мужчин >30 лет |
У мужчин с болезнью Андерсона-Фабри низкая (<10% от нормального уровня) или неопределяемая активность á-галактозидазы A. У женщин с болезнью Андерсона-Фабри уровень фермента в плазме и лейкоцитах часто в пределах нормы, поэтому при клиническом подозрении требуется генетическое тестирование |
|
Глюкоза натощак |
Может быть повышена при некоторых митохондриальных болезнях |
|
Оценка функции щитовидной железы |
Должна быть определена в момент постановки диагноза и мониторироваться каждые 6 мес. у пациентов с ГКМП, получающих амиодарон** |
|
Лактат плазмы |
Увеличен у некоторых пациентов при митохондриальных болезнях |
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, ИМ — инфаркт миокарда, СКФ — скорость клубочковой фильтрации, ХСН — хроническая сердечная недостаточность, BNP — мозговой натрийуретический пептид, NT-proBNP — N-концевой промозговой натрийуретический пептид.
Таблица 6/А3
Клинические особенности и инструментальные находки, позволяющие предположить диагноз фенокопии ГКМП (адаптировано из [203])
|
Фенокопия |
Методы |
Находки |
|
Болезнь Данон |
Клиническая симптоматика |
Как правило в детском возрасте, крайне редко — позднее начало. Скелетная миопатия, нарушения зрения, умственная отсталость. У женщин при поздней манифестации, может быть изолированная кардиальная форма |
|
ЭКГ |
Может быть предвозбуждение желудочков |
|
|
ЭхоКГ |
Массивная концентрическая ГЛЖ |
|
|
МРТ |
Чаще концентрическая ГЛЖ, с распространённым ПНГ преимущественно в средних и апикальных отделах ЛЖ. Характерно нарастание степени ПНГ от базальных отделов к апикальным, более выраженное вовлечение субэндокардиальных отделов |
|
|
Другие |
Х-связанное доминантное наследование. Для постановки диагноза — исследование креатинкиназы, биопсия мышц, генетическое тестирование (мутация в гене LAMP2) |
|
|
PRKAG2-синдром |
Клиническая симптоматика |
Проксимальная миопатия, миалгия, эпилепсия, раннее развитие АГ |
|
ЭКГ |
Предвозбуждение желудочков, блокады ножек пучка Гиса. Фибрилляция предсердий, трепетание предсердий. Выраженная синусовая брадикардия, атриовентрикулярная блокада, синоатриальная блокада |
|
|
ЭхоКГ |
Разная степень увеличения толщины миокарда ЛЖ. Систолическая и диастолическая дисфункция ЛЖ |
|
|
МРТ |
ГЛЖ от минимальной асимметричной без ПНГ в начальных стадиях, до выраженной с распространенным ПНГ в поздних стадиях |
|
|
Другие |
Аутосомно-доминантное наследование. Выявление мутаций в гене PRKAG2 |
|
|
Атаксия Фридрейха |
Клиническая симптоматика |
Прогрессирующая атаксия, потеря глубоких рефлексов, моторная слабость, дизартрия, сахарный диабет |
|
ЭКГ |
Снижение амплитуды или инверсия зубца Т. Наджелудочковые и желудочковые аритмии |
|
|
ЭхоКГ |
В динамике: концентрическое ремоделирование ЛЖ → концентрическая ГЛЖ (реже эксцентрическая ГЛЖ) → дилатация ЛЖ с систолической дисфункцией. "Блестящая" текстура миокарда |
|
|
МРТ |
На ранних стадиях — концентрическое ремоделирование/ГЛЖ. На поздних стадиях — заместительный фиброз |
|
|
Другие |
Аутосомно-рецессивный тип наследования. Исследование сывороточного уровня альфа-токоферола. МРТ головного мозга |
|
|
Болезнь Андерсена-Фабри |
Клиническая симптоматика |
Полисистемное поражение: нейропатия, изменения кожи (ангиокератомы), протеинурия, прогрессирующая хроническая почечная недостаточность. Сердце — болезнь мелких коронарных артерий |
|
ЭКГ |
Признаки ГЛЖ, изменения реполяризации, нарушение проводимости. Предвозбуждение желудочков. Предсердные и желудочковые аритмии |
|
|
ЭхоКГ |
Концентрическая или асимметричная ГЛЖ. Нарушение релаксации ЛЖ, нормальная ФВ ЛЖ. Может быть истончение миокарда задне-боковой стенки ЛЖ в поздней стадии. Гипертрофия правого желудочка. Кажущееся увеличение площади папиллярных мышц (относительно площади ЛЖ). Дилатация восходящей аорты |
|
|
МРТ |
Симметричная ГЛЖ, с наличием ПНГ в базальных отделах задне-боковой стенки ЛЖ в интрамиокардиальных отделах. Характерно снижение времени Т1 ниже нормы при Т1 картировании миокарда |
|
|
Другие |
Х-связанное рецессивное наследование. Исследование активности á-галактозидазы А. У мальчиков манифестирует в детском возрасте. У женщин может быть позднее начало |
|
|
Кардиальный амилоидоз |
Клиническая симптоматика |
ХСН с сохранной ФВ. Нарушения ритма. При ATTR — периферическая нейропатия, синдром запястного канала. Наследственная форма ТТР амилоидной КМП вызвана мутацией в гене транстиретина может проявиться в возрасте 30-40 лет [523] |
|
ЭКГ |
В зависимости от степени накопления амилоида — низкий вольтаж QRS (аномальные соотношения вольтаж/масса), нарушения проводимости, наджелудочковые аритмии |
|
|
ЭхоКГ |
Концентрическая ГЛЖ, иногда толщина МЖП > задней стенки ЛЖ. Дилатация предсердий. Утолщение створок клапанов. Небольшой гидроперикард. В начальных стадиях нормальная сократимость ЛЖ, не выраженные нарушения наполнения ЛЖ. В поздних стадиях — рестриктивный тип наполнения ЛЖ, снижение сократимости. Снижение скоростей s’, e’ и a’ при тканевой допплерографии (все <5 см/с), снижение глобальной продольной деформации ЛЖ с относительной сохранностью деформации верхушки ЛЖ (симптом "вишня в верхушке") позволяет заподозрить ATTР-KMП [308] |
|
|
МРТ |
ГЛЖ желудочков, иногда стенок предсердий. Субэндокардиальное и трансмуральное ПНГ с относительной невовлеченностью верхушки ЛЖ. Увеличение внеклеточного объема >27-28%, повышение времени Т1 выше нормы при Т1 картировании миокарда |
|
|
Другие |
При AL-амилоидозе — исследование моноклональных белков ê и ë в крови и моче. При ATTR — сцинтиграфия костей с бисфосфонатами. Биопсия миокарда или абдоминального жира. Увеличение уровня тропонина и NT-proBNP |
Сокращения: АГ — артериальная гипертензия, ГЛЖ — гипертрофия левого желудочка, КМП — кардиомиопатия, ЛЖ — левый желудочек, МЖП — межжелудочковая перегородка, МРТ — магнитно-резонансная томография, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ТТР — транстиреиновый, ФВ — фракция выброса, ХСН — хроническая сердечная недостаточность, ЭКГ — электрокардиография, ЭхоКГ — эхокардиография, ATTR — транстиреиновый амилоидоз, NT-proBNP — N-концевой промозговой натрийуретический пептид.
Таблица 7/А3
Диагностика у родственников пробанда, носителей мутаций генотип(+)/фенотип(-) в догипертрофической стадии (адаптировано из [524])
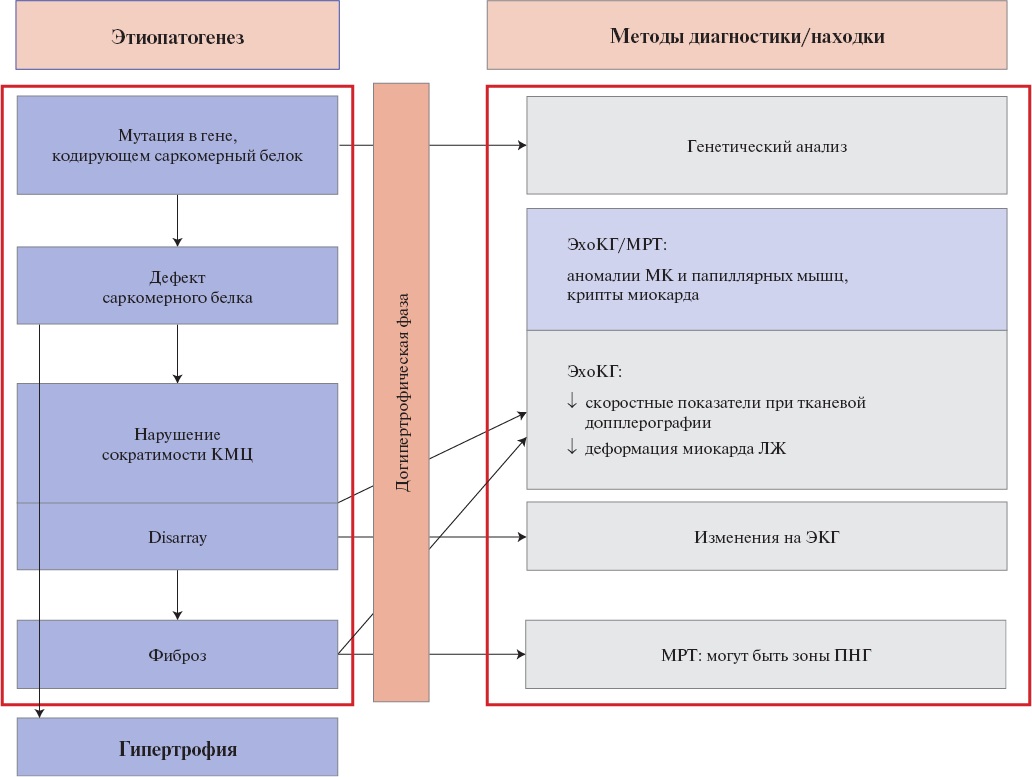
Сокращения: КМЦ — кардиомиоцит, ЛЖ — левый желудочек, МК — митральный клапан, МРТ — магнитно-резонансная томография, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ЭКГ — электрокардиография, ЭхоКГ — эхокардиография.
Таблица 8/А3
Электрокардиографические аномалии, позволяющие предположить конкретный диагноз фенокопии ГКМП или морфологический вариант ГКМП (по Rapezzi C, et al., 2013 [206])
|
Особенности |
Комментарий |
|
Короткий PR-интервал/раннее возбуждение |
Раннее возбуждение желудочков — частый феномен болезней накопления (болезни Помпе, PRKAG2 и Данона) и митохондриальных болезней (MELAS, MERFF). Короткий PR-интервал без раннего возбуждения желудочков встречается при болезни Андерсона-Фабри |
|
Атриовентрикулярная блокада |
Прогрессирующее замедление атриовентрикулярного проведения часто встречается при митохондриальных заболеваниях, некоторых болезнях накопления (включая болезнь Андерсона-Фабри), амилоидозе, десминопатиях, а также у пациентов с мутациями в гене PRKAG2 |
|
Выраженная ГЛЖ (индекс Соколова >50) |
Чрезвычайно большой вольтаж QRS типичен для болезней Помпе и Данона, но может быть результатом только раннего возбуждения желудочков |
|
Низкий вольтаж QRS (или нормальный вольтаж, несмотря на увеличение толщины стенки ЛЖ) |
Низкий вольтаж QRS в отсутствие перикардиального выпота, ожирения и болезни легких редко наблюдается при ГКМП (за исключением случаев стадии декомпенсации), но характерен для пациентов с AL-амилоидозом и реже — при транстиретиновом амилоидозе. Дифференциальный диагноз между ГКМП и кардиальной формой амилоидоза: аномальное соотношение (низкий вольтаж при толщине стенки ЛЖ ≥12 мм) характерно для кардиального амилоидоза (чувствительность 75%, специфичность 67%) |
|
Вектор QRS от -90° до -150° |
Наблюдается у пациентов с синдромом Нунан, имеющих выраженную базальную гипертрофию, распространяющуюся на выходной тракт правого желудочка |
|
Гигантский негативный зубец T (>10 мм) |
Гигантский негативный зубец T в прекордиальных и/или переднелатеральных отведениях свидетельствует о вовлечении верхушки ЛЖ |
|
Патологический зубец Q (>40 мс и/или >25% глубины R-волны и/или глубина >3 мм хотя бы в двух отведениях, кроме aVR) |
Аномально глубокий зубец Q в переднелатеральных отведениях, обычно с положительной Т-волной, ассоциирован с асимметричной гипертрофией ЛЖ. Аномальная продолжительность зубца Q (≥40 мс) ассоциирована с областями фиброзного замещения |
|
Сводчатая элевация сегмента ST в латеральных грудных отведениях |
У некоторых пациентов с апикальной или дистальной гипертрофией развиваются апикальные аневризмы, иногда ассоциированные с фиброзом миокарда. Малых размеров аневризмы выявляются только при МРТ сердца, ЭхоКГ с контрастированием или вентрикулографии, часто ассоциированы с элевацией сегмента ST в латеральных грудных отведениях |
Сокращения: ГКМП — гипертрофическая кардиомиопатия, ГЛЖ — гипертрофия левого желудочка, ЛЖ — левый желудочек, МРТ — магнитно-резонансная томография, ЭхоКГ — эхокардиография.
Таблица 9/А3
Параметры протокола ТТ-ЭхоКГ-исследования у пациента с ГКМП (адаптировано из [180][275])
|
Параметры |
Комментарии |
|
Толщина миокарда ЛЖ (в 16 сегментах ЛЖ) Количество гипертрофированных сегментов ЛЖ |
— Измерение толщины стенок ЛЖ следует проводить в конечно- диастолическую фазу, предпочтительно — в парастернальной позиции по короткой оси ЛЖ (желательно толщину миокарда в гипертрофированных сегментах оценивать в нескольких проекциях, но измерения в апикальных сканах переоценивают толщину миокарда из-за ограничений бокового разрешения). — Избегать включения в толщину миокарда ПЖ-трабекул. — Критичные показатели: максимальная толщина стенки ЛЖ (стратификация риска ВСС) и толщина стенки в месте митрально-септального контакта (выбор СМЭ-ЭСА) |
|
Тип гипертрофии ЛЖ Паттерн морфологии МЖП |
Асимметричная, симметричная, апикальная, средне-желудочковая, другие отделы ЛЖ. Морфология МЖП: двояковыпуклая, сигмовидная (S-образная), гипертрофия всей МЖП |
|
Толщина миокарда ПЖ |
Оценивают в базальных, срединных и апикальных сегментах (нормальные размеры <5 мм в изображении парастернальном по длинной оси на уровне хорд трикуспидального клапана). Избегать включения эпикардиального жира в измерение миокарда ПЖ |
|
Текстура миокарда ЛЖ |
"Блестящий", гранулярность (для исключения фенокопий ГКМП). Наличие крипт миокарда (при МРТ более точная диагностика) |
|
Измерение размеров и определение объемов ЛЖ |
КДР*, КСР, КДО и КСО |
|
Измерение размеров ПЖ |
В парастернальной и апикальной позиции |
|
Измерение размеров и определение объемов ЛП и ПП |
Увеличение ЛП относится к дополнительным факторам риска ВСС |
|
Оценка толщины межпредсердной перегородки |
Для исключения фенокопий ГКМП (амилоидоз) |
|
Визуальная оценка кинетики миокарда ЛЖ и ПЖ |
Выявление зон ишемии/перенесенного ИМ |
|
Визуальная оценка клапанов (МК, АК, ТК, ЛК) Измерение длины передней створки МК Оценка SAM-синдрома |
Особое внимание — МК: — наличие передне-систолического движения створок МК, наличие митрально-септального контакта (важная характеристика ГКМП, но также может наблюдаться не при ГКМП у пациентов с маленьким ЛЖ независимо от наличия ГЛЖ, при гиповолемии, после кардиоторакальных хирургических вмешательств); — есть ли удлинение (избыточность) створок МК, наличие и степень пролабирования створок МК. По степени выраженности SAM-синдрома выделяют: — небольшое ПСД МК — нет септально-митрального контакта; — умеренное — митрально-септальный контакт <30% длительности систолы; — выраженный SAM-синдром — митрально-септальный контакт >30% длительности систолы |
|
Папиллярные мышцы |
Количество, есть ли дислокация |
|
Наличие и степень обструкции ВТЛЖ или срединно-желудочковой обструкции |
— Регистрация кровотока через АК/ВТЛЖ — паттерн допплеровского спектра и величина ГД в ВТЛЖ. — Следует использовать следующие формулы для расчета ГД в ВТЛЖ: уравнение Бернули ∆p=4×Vmax, если можно точно измерить скорость кровотока в пути оттока ЛЖ; формула клиники Мейо "∆p=((4×Vmax МР)+pЛП)–системное систолическое АД", если наличие выраженной митральной регургитации не позволяет точно измерить скорость кровотока в пути оттока ЛЖ (рЛП — давление в левом предсердии, используется константа — 20 мм рт.ст.). — Необходимо убедиться, что регистрируется только кровоток в ВТЛЖ и не "захватывается" ток митральной регургитации. — Если в покое ГД в ВТЛЖ <30 мм рт.ст., следует провести провокационную пробу Вальсальвы. — У некоторых пациентов величина ГД в ВТЛЖ больше в положении сидя и стоя, чем лежа, поэтому необходимо измерение ГД и в положении пациента стоя. Если в положении лежа у пациента проба Вальсальвы отрицательна, то необходимо провести пробу также в положении пациента стоя |
|
Есть ли обструкция выходного тракта ПЖ |
Регистрация скорости кровотока в ВТПЖ и на уровне средних сегментов ПЖ |
|
Оценка клапанной регургитации, особенно МР |
При МР, обусловленной ПСД МК, ток, как правило, направлен латерально и кзади, а степень МР пропорциональна выраженности ПСД и митрально-септальному контакту. Если направление тока МР атипично или не пропорциональна ПСД, возможна самостоятельная патология МК; это критично для выбора хирургического или эндоваскулярного метода лечения |
|
Исследование систолической функции ЛЖ и ПЖ |
ФВ ЛЖ часто сверхнормальна, особенно при маленьком ЛЖ, что может не корректно отражать сократимость кардиомиоцитов. Более точны продольный 2D-strain и тканевая допплерография (s’ <4 см/с — предиктор развития ХСН и плохого прогноза). Для ПЖ: TAPSE, 2D-strain стенки ПЖ |
|
Исследование диастолической функции ЛЖ |
Согласно рекомендациям ASE и EACVI (2016) при ГКМП следует оценивать степень диастолической дисфункции. Ключевой параметр диастолической дисфункции ЛЖ — давление наполнения ЛЖ (КДД ЛЖ). Его неинвазивная оценка многофакторна. По рекомендациям ASE и EACVI (2016) при ГКМП вывод о повышении КДД ЛЖ следует, если: 1. ср. E/e’ >14 см/с, 2. разница длительности реверсивной волны А в легочных венах и волны А трансмитрального кровотока (Ar-A) ≥30 мс, 3. индекс объема ЛП ≥34 мл мл/м², 4. пиковая скорость трикуспидальной регургитации >2,8 м/с (СДЛА >35-40 мм рт.ст.). Более подробно об алгоритмах оценки диастолической дисфункции в разных клинических ситуациях — см. рекомендации ASE/EACVI (2016) по исследованию диастолической функции ЛЖ |
|
Оценка продольной деформации ЛЖ (2D-strain) |
С построением сегментарной схемы-мишени ЛЖ (bull’s eye). Паттерны 2D-strain различны при ГКМП и фенокопиях ГКМП |
|
Оценка наличия жидкости в полости перикарда |
Исключение фенокопий ГКМП (характерно для кардиального амилоидоза) |
|
Оценка диаметра и степени коллабирования нижней полой вены |
Необходима для расчета СДЛА |
Примечание: * — при S-образной МЖП КДР следует измерять в 2 вариантах — на уровне базальных сегментов ЛЖ и ближе к срединным сегментам, где он максимален (см. рекомендации ASE 2019).
Сокращения: АД — артериальное давление, АК — аортальный клапан, ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ВТПЖ — выходной тракт правого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, ГЛЖ — гипертрофия левого желудочка, ИМ — инфаркт миокарда, КДД — конечно-диастолическое давление, КДО — конечно-диастолический объем, КДР — конечно-диастолический размер, КСР — конечно-систолический размер, КСО — конечно-систолический объем, ЛЖ — левый желудочек, ЛК — легочный клапан, ЛП — левое предсердие, МЖП — межжелудочковая перегородка, МК — митральный клапан, МР — митральная регургитация, МРТ — магнитно-резонансная томография, ПЖ — правый желудочек, ПП — правое предсердие, ПСД — переднее систолическое движение, СДЛА — систолическое давление в легочной артерии, СМЭ — септальная миоэктомия, ТК — трикуспидальный клапан, ФВ — фракция выброса, ХСН — хроническая сердечная недостаточность, ЭСА — этаноловая септальная аблация, ASE/EACVI — Американское эхокардиографическое общество/Европейская ассоциация по сердечно-сосудистой визуализации.
Таблица 10/А3
Заболевания (кроме ОГКМП), при которых может регистрироваться обструкция ВТЛЖ и SAM-синдром (ПСД МК) (адаптировано из [203])
|
Пожилые пациенты с сочетанием АГ, сигмовидной МЖП и гипердинамичным ЛЖ |
|
Компенсаторная гиперсократимость базальных сегментов ЛЖ при остром верхушечном инфаркте миокарда |
|
КМП такоцубо с гиперсократимостью базальных сегментов ЛЖ |
|
Массивная кальцификация задних сегментов митрального кольца |
|
После хирургических и эндоваскулярных вмешательствах на МК |
|
После протезирования АК у пациентов с ГЛЖ и гипердинамичным ЛЖ |
|
Пожилые пациенты с анемией, гиповолемией, тахиаритмиями, сепсисом |
|
Использование препаратов: инотропы, вазодилататоры, симпатомиметики |
|
Перегрузка давлением ПЖ (обострение ХОБЛ и/или ОРДС) |
|
Фенокопии ГКМП (кардиальный амилоидоз, болезнь Фабри) |
Сокращения: АГ — артериальная гипертония, АК — аортальный клапан, ГКМП — гипертрофическая кардиомиопатия, ГЛЖ — гипертрофия левого желудочка, КМП — кардиомиопатия, ЛЖ — левый желудочек, МЖП — межжелудочковая перегородка, МК — митральный клапан, ОРДС — острый респираторный дистресс-синдром, ПЖ — правый желудочек, ХОБЛ — хроническая обструктивная болезнь легких.
Таблица 11/А3
Дополнительные опции при ЭхоКГ
|
Опция |
Цель использования |
|
Оценка продольной деформации ЛЖ (2D-strain) |
С построением сегментарной схемы-мишени ЛЖ (bull’s eye). Паттерны 2D-strain различны при ГКМП и фенокопиях ГКМП |
|
3D реконструкция |
Оценка морфологии МК для выбора хирургической тактики |
Сокращения: ГКМП — гипертрофическая кардиомиопатия, ЛЖ — левый желудочек, МК — митральный клапан.
Таблица 12/А3
ЭхоКГ особенности, позволяющие предположить диагноз фенокопии ГКМП (адаптировано из [3])
|
Особенности |
Комментарий |
|
Утолщение межпредсердной перегородки |
Амилоидоз |
|
Утолщение створок МК |
Амилоидоз, болезнь Андерсона-Фабри |
|
Гипертрофия свободной стенки ПЖ |
Амилоидоз, миокардит, болезнь Андерсона-Фабри, синдром Нунан |
|
Перикардиальный выпот |
Амилоидоз, миокардит |
|
Увеличение эхогенности миокарда ЛЖ |
Амилоидоз |
|
Концентрическая ГЛЖ |
Митохондриальные болезни, амилоидоз, болезнь Андерсона-Фабри, мутации в гене PRKAG2 |
|
Экстремальная концентрическая ГЛЖ (толщина стенок ≥30 мм) |
Болезнь Данона, болезнь Помпе |
|
Глобальная гипокинезия ЛЖ (с наличием или отсутствием дилатации ЛЖ) |
Митохондриальные болезни, амилоидоз, мутации в гене PRKAG2, Болезнь Данона, миокардит, поздняя стадия ГКМП, болезнь Андерсона-Фабри |
|
Обструкция выходного тракта ПЖ |
Синдром Нунан и ассоциированные синдромы |
Сокращения: ГКМП — гипертрофическая кардиомиопатия, ГЛЖ — гипертрофия левого желудочка, МК — митральный клапан, ЛЖ — левый желудочек, ПЖ — правый желудочек.
Таблица 13/А3
Параметры, которые необходимо оценить при МРТ сердца у пациента с ГКМП
|
Структуры |
Параметры |
|
ЛЖ |
КДО, КСО, КДР, ФВ, масса миокарда |
|
наличие нарушений сегментарного сокращения миокарда ЛЖ |
|
|
ВТЛЖ |
анатомические особенности ВТЛЖ, типа и места обструкции в ЛЖ |
|
величина пиковой скорости/ГД в ВТЛЖ (фазово-контрастная МРТ с кодированием скорости) |
|
|
ПЖ |
КДО, КСО, ФВ, размеры, наличие обструкции в ВТПЖ |
|
Миокард ЛЖ |
— толщина миокарда ЛЖ в диастолу по короткой оси ЛЖ согласно 17-ти сегментарной модели — локализация/распространенность/количество гипертрофированных сегментов ЛЖ — морфологический тип ГКМП (асимметричная, симметричная, апикальная, среднежелудочковая) — паттерн морфологии МЖП (двояковыпуклая, сигмовидная, вся МЖП) |
|
ПНГ |
наличие, паттерн, распространенность ПНГ в % от общей массы миокарда ЛЖ |
|
МР и ТР |
наличие митральной и трикуспидальной регургитации, степень, фракция регургитации |
|
Аппарат МК (створки, хорды, папиллярные мышцы) |
строение, описание аномалий (смещение/"расщепление" головок и гипермобильность папиллярных мышц), связь с обструкцией ВТЛЖ и митральной регургитацией |
|
ЛП и ПП |
размеры |
|
Дополнительные аномалии |
при планировании СМЭ — идентифицирование "крипт" у пациентов с ГКМП с указанием количества и глубины дефектов |
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ВТПЖ — выходной тракт правого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, КДО — конечно-диастолический объем, КДР — конечно-диастолический размер, КСО — конечно-систолический объем, ЛЖ — левый желудочек, ЛП — левое предсердие, МЖП — межжелудочковая перегородка, МК — митральный клапан, МР — митральная регургитация, МРТ — магнитно-резонансная томография, ПЖ — правый желудочек, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ПП — правое предсердие, СМЭ — септальная миоэктомия, ТК — трикуспидальный клапан, ТР — трикуспидальная регургитация, ФВ — фракция выброса.
Таблица 14/А3
Варианты нагрузочных тестов
|
Нагрузочный тест |
Аппаратура для нагрузки |
Показания/цель |
|
Нагрузочный тест с регистрацией ЭКГ и АД |
Тредмил Велоэргометр (реже) |
Стратификация риска ВСС |
|
Стресс-ЭхоКГ |
Тредмил "Лежачий" велоэргометр |
— Диагностика латентной обструкции — Стратификация риска ВСС (динамика АД и ГД) — Индуцируется ли ишемия миокарда — Оценка эффективности проводимой терапии — Планирование диагностических мероприятий у пациентов с болями в области сердца (необходимость коронароангиографии) |
|
Эргоспирометрия |
Тредмил |
При планировании трансплантации сердца |
Сокращения: АД — артериальное давление, ВСС — внезапная сердечная смерть, ГД — градиент давления, ЭКГ — электрокардиография, ЭхоКГ — эхокардиография.
Таблица 15/А3
Схема дифференциального диагноза ГКМП и базальной септальной гипертрофии (адаптировано из [515])
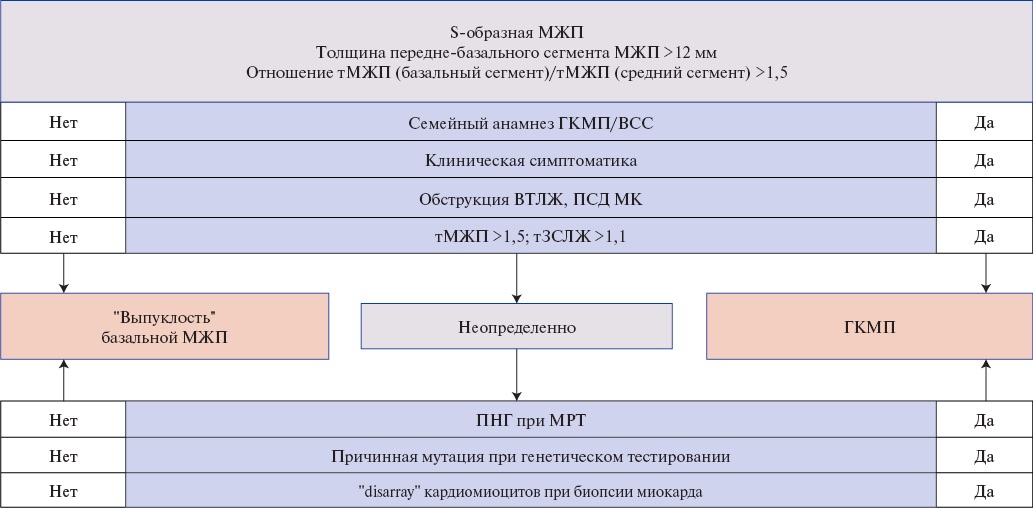
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ВСС — внезапная сердечная смерть, ГКМП — гипертрофическая кардиомиопатия, МЖП — межжелудочковая перегородка, МК — митральный клапан, МРТ — магнитно-резонансная томография, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ПСД — переднее систолическое движение, тЗСЛЖ — толщина задней стенки левого желудочка, тМЖП — толщина межжелудочковой перегородки.
Таблица 16/А3
Дифференциальная диагностика ГКМП и спортивной ГЛЖ
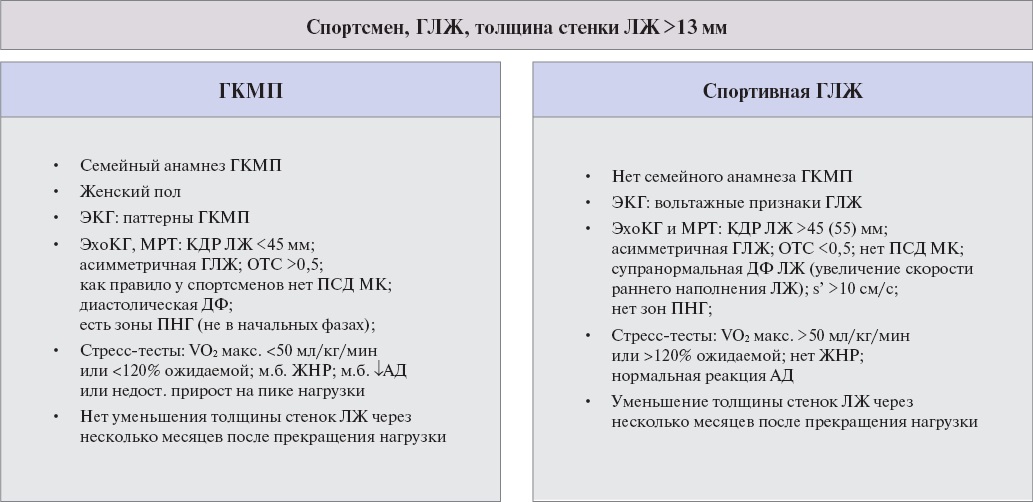
Сокращения: АД — артериальное давление, ГКМП — гипертрофическая кардиомиопатия, ГЛЖ — гипертрофия левого желудочка, ДФ — дисфункция, ЖНР — желудочковые нарушения ритма, КДР — конечно-диастолический размер, ЛЖ — левый желудочек, МК — митральный клапан, МРТ — магнитно-резонансная томография, ОТС — относительная толщина стенки, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ПСД — переднее систолическое движение, ЭКГ — электрокардиография, ЭхоКГ — эхокардиография.
Таблица 17/А3
Правила и особенности назначения бета-адреноблокаторов при ГКМП
|
Бета-адреноблокаторы остаются наиболее эффективной группой лекарственных средств, применяемых в лечении ГКМП |
|
В связи с большей комплаентностью у пациентов рекомендуется отдавать предпочтение селективным бета-адреноблокаторам пролонгированного действия, в частности, бисопрололу**, метопрололу** |
|
Дозу бета-адреноблокатора рекомендуется титровать до достижения ЧСС 55-65 уд./мин под контролем АД и симптомов |
|
Следует помнить о других известных побочных эффектах бета-адреноблокаторов: нарушение проводимости вплоть до полной АВ-блокады, бронхоспазм, вазоконстрикция периферических сосудов, нарушение толерантности к глюкозе, эректильная дисфункция и других |
|
Высокие дозы обычно хорошо переносятся. Побочные эффекты (жалобы в основном на усталость) должны быть тщательно исследованы, чтобы оценить оптимальную индивидуальную дозу для конкретного пациента |
Сокращения: АВ — атриовентрикулярный, АД — артериальное давление, ГКМП — гипертрофическая кардиомиопатия, ЧСС — частота сердечных сокращений.
Таблица 18/А3
Правила и особенности назначения верапамила** при ГКМП
|
Назначение верапамила** рекомендуется начинать в условиях стационара с малых доз — 20-40 мг 3 раза в день с постепенным их повышением при хорошей переносимости до снижения ЧСС в покое до 55-65 уд./мин |
|
Верапамил** обеспечивает симптоматический эффект у 65-80% пациентов, включая случаи рефрактерности к лечению бета-адреноблокаторами |
|
Польза верапамила** ограничена его сосудорасширяющими эффектами, которые у отдельных пациентов могут перевешивать его отрицательный инотропный эффект |
|
Верапамил** предпочтителен для молодых пациентов с легкой и умеренной обструкцией (ГД в ВТЛЖ в покое <50 мм рт.ст.) [382] |
|
Пациентам старше 65 лет необходимо назначение низких доз и титрация препарата под контролем ГД в ВТЛЖ, ЧСС (ЭКГ) и клинических симптомов |
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ЧСС — частота сердечных сокращений, ЭКГ — электрокардиография.
Таблица 19/А3
Начальные и целевые дозы при медикаментозной терапии ГКМП
|
Препарат |
Начальная доза |
Целевая доза |
|
— пропранолол** — метопролол** — атенолол** — бисопролол** — соталол** |
40-80 мг/сут. 25-50 мг/сут. 25-50 мг/сут. 1,25-2,5 мг/сут. 80 мг/сут. |
240 мг/сут. 100-200 мг/сут. 150-200 мг/сут. 10 мг/сут. 160-240 мг/сут. |
|
— верапамил** — верапамил** (пролонгированного действия) — дилтиазем |
60-120 мг/сут. 120 мг/сут. 60-120 мг/сут. |
240-480 мг/сут. 240-480 мг/сут. 180-360 мг/сут. |
Таблица 20/А3
Рекомендуемая частота обязательных анализов крови на креатинин у пациентов, принимающих антикоагулянты
|
Кратность |
Категории пациентов |
|
1 раз в год |
всем пациентам моложе 75 лет с исходным КК ≥60 мл/мин |
|
1 раз в 6 мес. |
пациентам ≥75 лет, особенно со старческой астенией |
|
1 раз в N мес. |
N=КК/10 (применимо, если КК <60 мл/мин) |
|
По требованию |
дополнительное проведение анализов, если возникли какие-либо интеркуррентные заболевания/состояния/прием препаратов, которые могли повлиять на функцию почек |
Сокращение: КК — клиренс креатинина.
Таблица 21/А3
Рекомендованные лабораторные анализы и диагностические обследования для поиска потенциального субстрата кровотечения (перед назначением антикоагулянтов)
|
Обследование |
Цель |
ЕОК |
УУР |
УДД |
|
Общий (клинический) анализ крови развернутый с определением Hb, количества эритроцитов, тромбоцитов* |
Исключение анемии и тромбоцитопении |
Нет |
С |
5 |
|
Анализ крови биохимический общетерапевтический, включая определение активности аланинаминотрансферазы в крови; определение активности аспартатаминотрансферазы в крови; исследование уровня общего билирубина в крови; определение активности щелочной фосфатазы нейтрофилов периферической крови; исследование уровня общего белка в крови |
Исключить патологию печени |
Нет |
С |
5 |
|
Исследование уровня креатинина в крови и в моче с расчетом скорости клубочковой фильтрации и клиренса креатинина по формуле Кокрофта-Голта без стандартизации к площади поверхности тела |
Исключить хроническую болезнь почек, выбрать антикоагулянт в соответствующей дозе |
IA |
А |
1 |
|
МНО |
Для определения класса патологии печени по Чайлд-Пью |
Нет |
С |
5 |
|
Общий (клинический) анализ мочи |
Исключить эритроцитурию и протеинурию |
Нет |
С |
5 |
|
Эзофагогастродуоденоскопия всем пациентам с анамнезом желудочно-кишечных кровотечений, эрозивно-язвенного поражения пищевода, желудка или двенадцатиперстной кишки |
Исключить обострение язвенной болезни и наличие острых эрозий |
Нет |
С |
5 |
|
Колоноскопия пациентам с диагностированной железодефицитной анемией, но отсутствием явных источников кровотечения |
Для исключения патологии толстого кишечника, прежде всего, онкологии |
Нет |
С |
5 |
|
Компьютерная томография или магнитно-резонансная томография головного мозга и интракраниальных артерий пациентам, недавно перенесшим инсульт (в предыдущие 8 нед.), а также при выраженном остаточном неврологическом дефиците и отсутствии данных нейровизуализации |
Исключить геморрагический характер инсульта и сосудистые мальформации |
Нет |
С |
5 |
Примечание: * — назначение антикоагулянтов не рекомендовано при уровне тромбоцитов <20×10⁹/л.
Сокращения: ЕОК — Европейское общество кардиологов, МНО — международное нормализованное отношение, УДД — уровни достоверности доказательств, УУР — уровни убедительности рекомендаций.
Таблица 22/А3
Рекомендуемые режимы антикоагулянтной терапии при ГКМП у беременных с ФП и опасности, связанные с терапией варфарином**
|
Режимы антикоагулянтной терапии |
|
|
Режим 1 |
Постоянная терапия варфарином** за исключением срока 6-12 нед. (отмена должна начинаться с начала 5 нед. с учетом периода полувыведения) с переходом на этот срок на гепарин натрия** (низкомолекулярный) (минимальный риск тромбоза и возможный риск эмбриопатии) |
|
Режим 2 |
Переход на парентеральные прямые антикоагулянты (гепарин натрия**) на весь срок беременности (минимальный риск эмбриопатии, но повышенный по сравнению с терапией варфарином** риск тромбозов) |
|
Опасности, связанные с применением варфарина |
|
|
Период полувыведения варфарина** превышает 60 ч, что необходимо учитывать при определении сроков отмены препарата |
|
|
Некоторые авторы отмечают дозозависимый эмбриотоксический эффект варфарина** — доза <5 мг редко приводит к возникновению эмбриопатии. Однако на практике доза варфарина определяется величиной МНО и не может быть произвольно уменьшена или увеличена |
|
|
Наиболее критическим периодом действия варфарина** является срок 6-12 нед. — максимальная вероятность эмбриотоксического эффекта |
|
|
Вызывая гипокоагуляцию у плода, варфарин** может приводить к нарушениям формирования ЦНС, вызывая внутричерепные кровоизлияния |
|
|
Угнетая синтез витамин-К зависимых факторов, варфарин** существенно влияет на процесс формирования и роста костей плода |
|
|
Результатом эмбриотоксичности варфарина** являются гипоплазия носовых костей, атрофия зрительного нерва, задержка умственного развития, а также замершие беременности, спонтанные аборты и мертворождения |
|
Сокращения: МНО — международное нормализованное отношение, ЦНС — центральная нервная система.
Таблица 23/А3
Ограничения в методах диагностики при беременности
|
Метод |
Ограничения |
УУР |
УДД |
|
ЭКГ |
нет ограничений |
1 |
С |
|
Электро-физиологическое исследование |
может быть выполнено по жизненно важным показаниям |
3 |
С |
|
ЭхоКГ |
ТТ-ЭхоКГ — нет ограничений ЧП-ЭхоКГ — если ТТ-ЭхоКГ недостаточно для постановки диагноза или детализации нарушений |
1 |
С |
|
МРТ |
без использования контраста (гадолиний) может быть выполнена в случае, если ЭхоКГ недостаточно для постановки диагноза |
2 |
С |
|
КТ/МСКТ |
может быть выполнена по жизненно важным показаниям |
3 |
С |
|
Рентгенография органов грудной клетки |
может быть выполнена в случае, если другие методы обследования не могут объяснить генез одышки |
3 |
С |
Сокращения: МРТ — магнитно-резонансная томография, КТ/МСКТ — компьютерная томография/мультиспиральная компьютерная томография, ТТ-ЭхоКГ — трансторакальная эхокардиография, УДД — уровни достоверности доказательств, УУР — уровни убедительности рекомендаций, ЧП-ЭхоКГ — чреспищеводная эхокардиография, ЭКГ — электрокардиография, ЭхоКГ — эхокардиография.
Таблица 24/А3
Основные мероприятия по профилактике осложнений у пациентов с ГКМП
|
Симптом/осложнение ГКМП |
Профилактические мероприятия |
|
ВСС и жизнеугрожающие нарушения ритма |
первичная и вторичная профилактика ВСС — см. Раздел "Стратификация риска ВСС" |
|
Тромбоэмболические осложнения у пациентов с ФП |
по общим принципам тромбопрофилактики при ФП (см. рекомендации по лечению ФП) |
|
Инфекционный эндокардит |
антибиотикопрофилактика рекомендуется только перед процедурами высокого риска пациентам с ГКМП и протезами клапанов сердца, врожденным пороком сердца или если пациент ранее переносил инфекционный эндокардит (см. соответствующие рекомендации). У пациентов с имплантированным ИКД*** профилактика инфекционного эндокардита — по рекомендациям РКО по инфекционному эндокардиту 2022г |
Сокращения: ВСС — внезапная сердечная смерть, ГКМП — гипертрофическая кардиомиопатия, ИКД — имплантируемый кардиовертер-дефибриллятор, ФП — фибрилляция предсердий.
Приложение Б. Алгоритмы ведения пациента
Приложение Б1. Алгоритм тактики ведения асимптомных пациентов с ГКМП
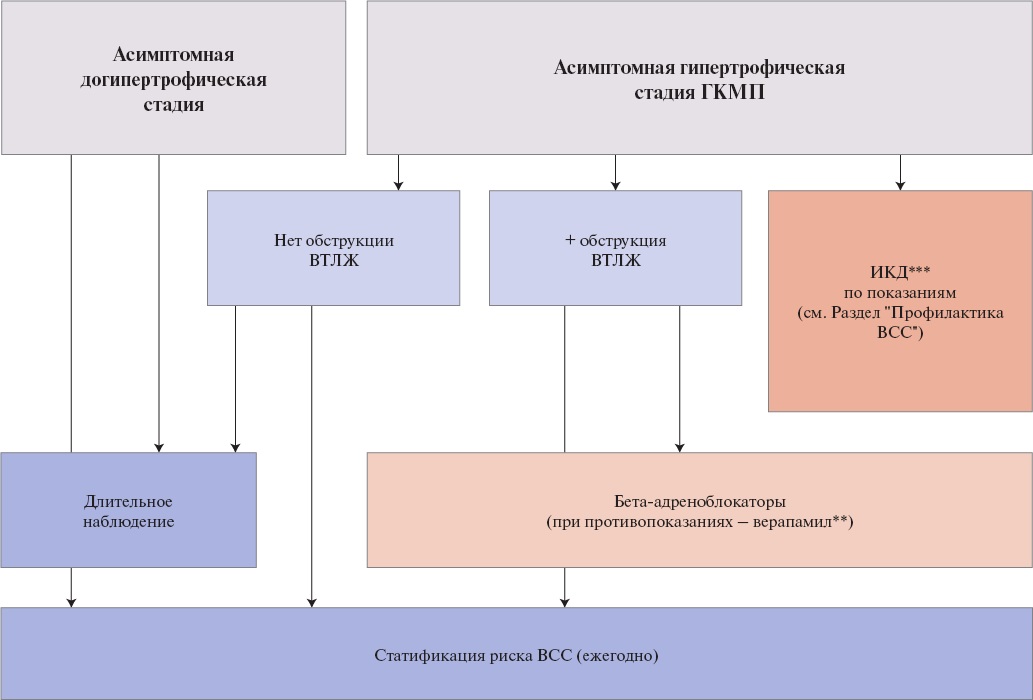
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГКМП — гипертрофическая кардиомиопатия, ИКД — имплантируемый кардиовертер-дефибриллятор.
Приложение Б2. Упрощенный алгоритм диагностики и подходов к лечению пациентов с обструкцией на уровне ВТЛЖ
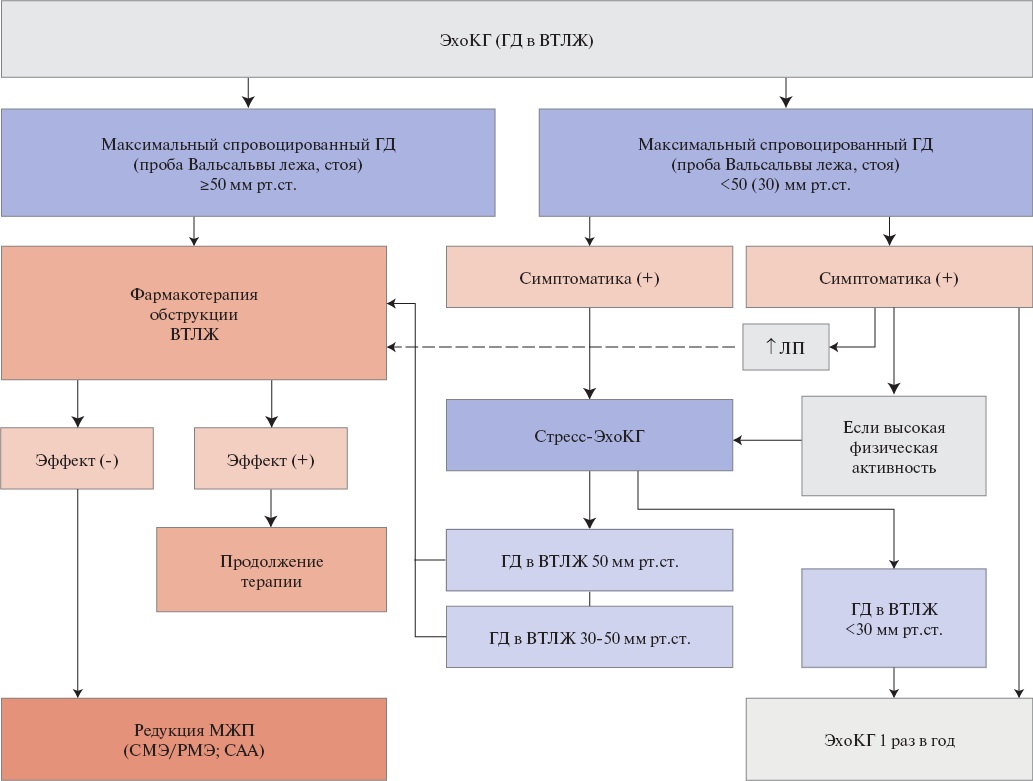
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ЛП — левое предсердие, МЖП — межжелудочковая перегородка, СМЭ — септальная миоэктомия, ЭСА — этаноловая септальная аблация, ЭхоКГ — эхокардиография.
Приложение Б3. Алгоритм фармакотерапии ОГКМП
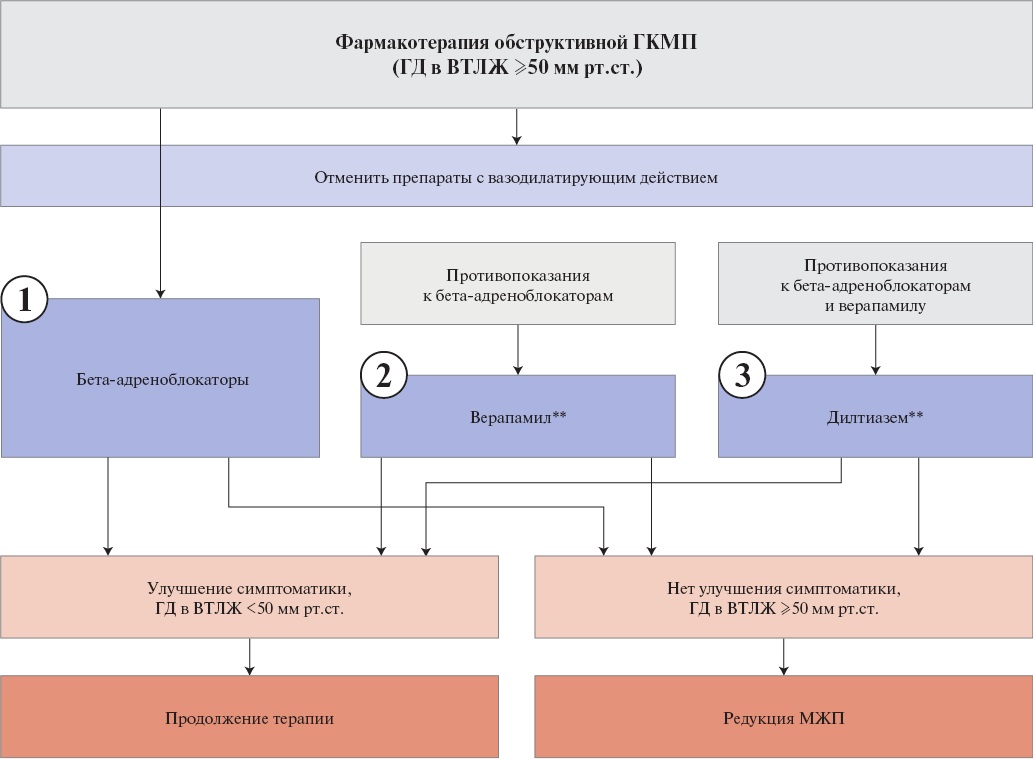
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, МЖП — межжелудочковая перегородка.
Приложение Б4. Алгоритм врачебной тактики лечения ХСН при ГКМП
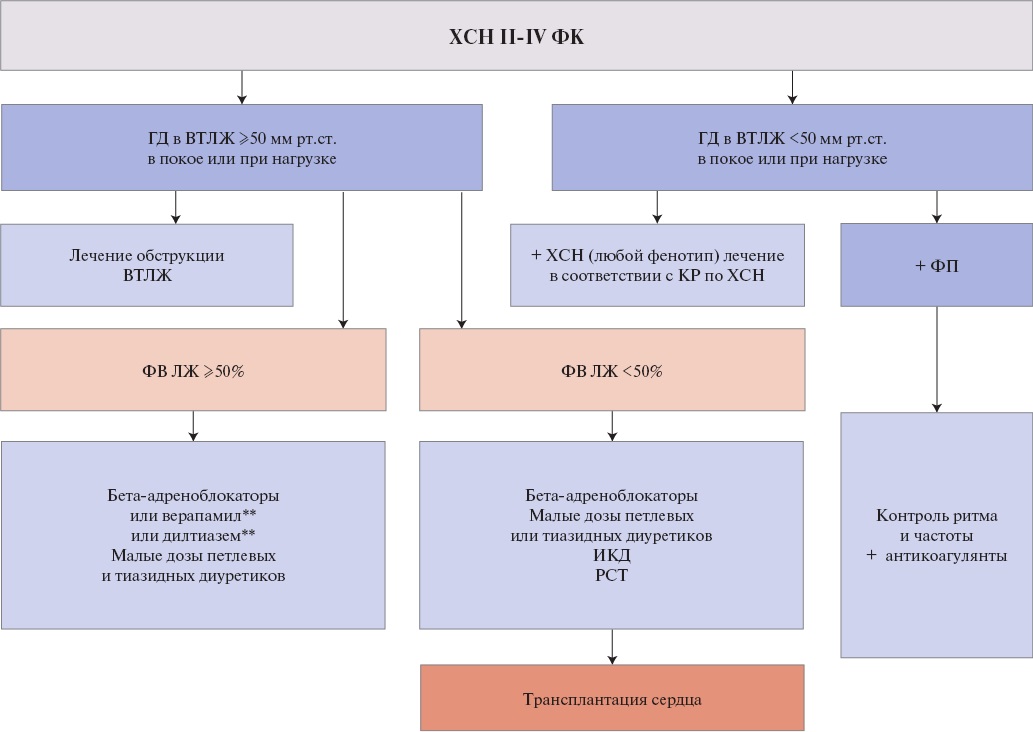
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ИКД — имплантируемый кардиовертер-дефибриллятор, КР — клинические рекомендации, ЛЖ — левый желудочек, РСТ — ресинхронизирующая терапия, ФВ — фракция выброса, ФК — функциональный класс, ФП — фибрилляция предсердий, ХСН — хроническая сердечная недостаточность.
Приложение Б5. Алгоритм выбора хирургического/эндоваскулярного вмешательства у пациентов с ГКМП
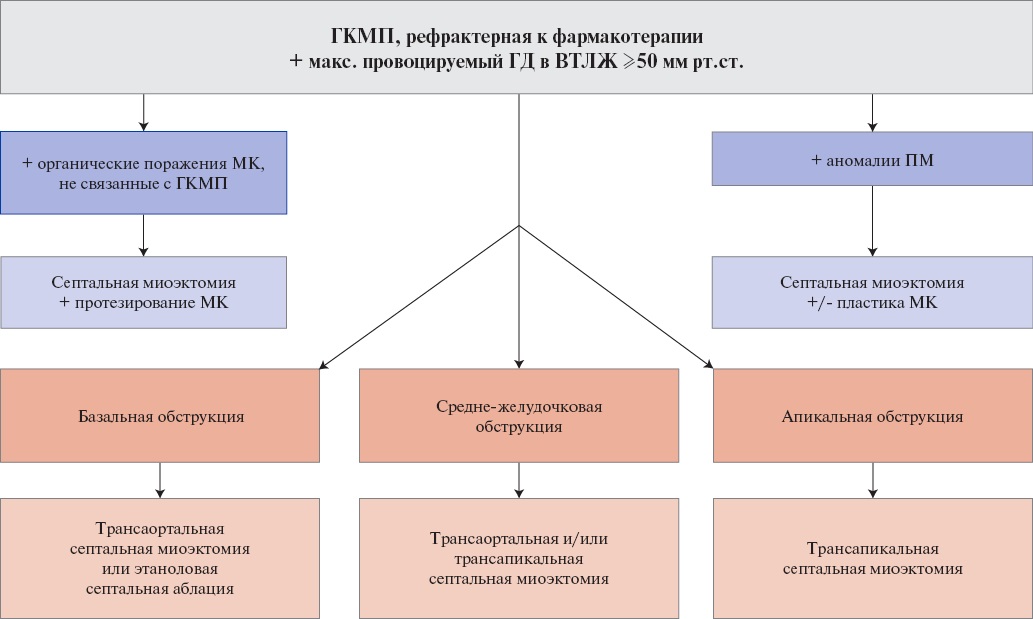
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, МК — митральный клапан, МР — митральная регургитация.
Приложение Б6. Алгоритм выбора метода редукции МЖП
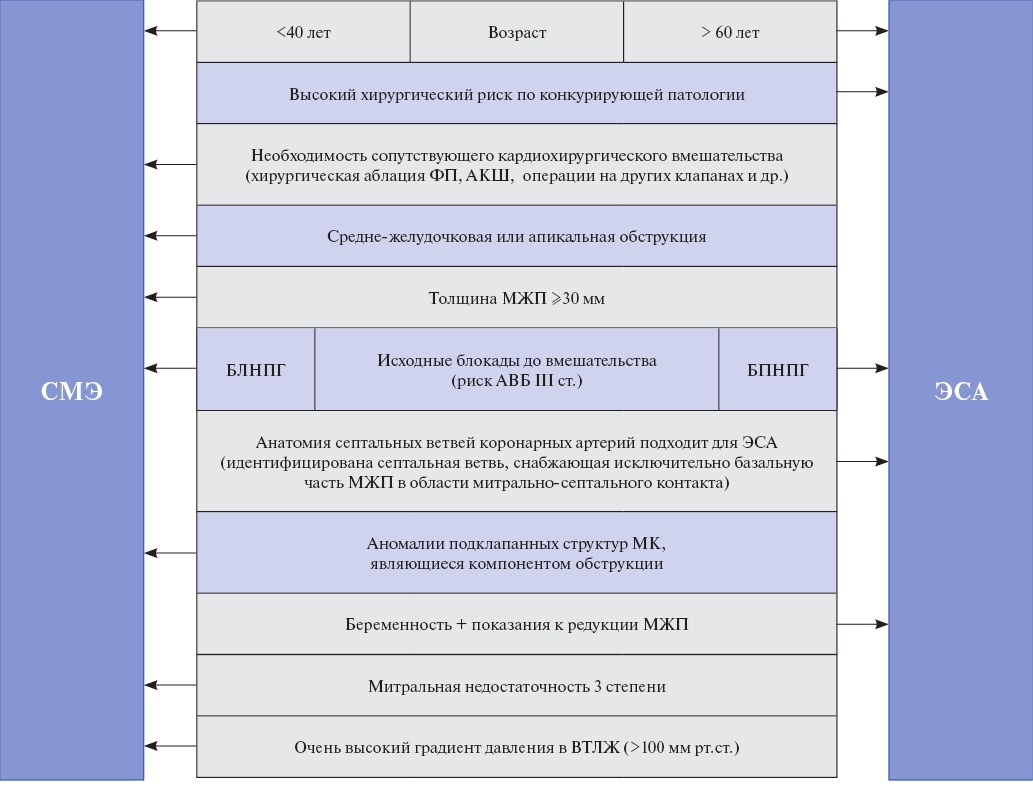
Сокращения: АВБ — атриовентрикулярная блокада, АКШ — аортокоронарное шунтирование, БЛНПГ — блокада левой ножки пучка Гиса, БПНПГ — блокада правой ножки пучка Гиса, ВТЛЖ — выходной тракт левого желудочка, МЖП — межжелудочковая перегородка, МК — митральный клапан, СМЭ — септальная миоэктомия, ФП — фибрилляция предсердий, ЭСА — этаноловая септальная аблация.
Приложение Б7. Алгоритм первичной и вторичной профилактики ВСС у пациентов с ГКМП
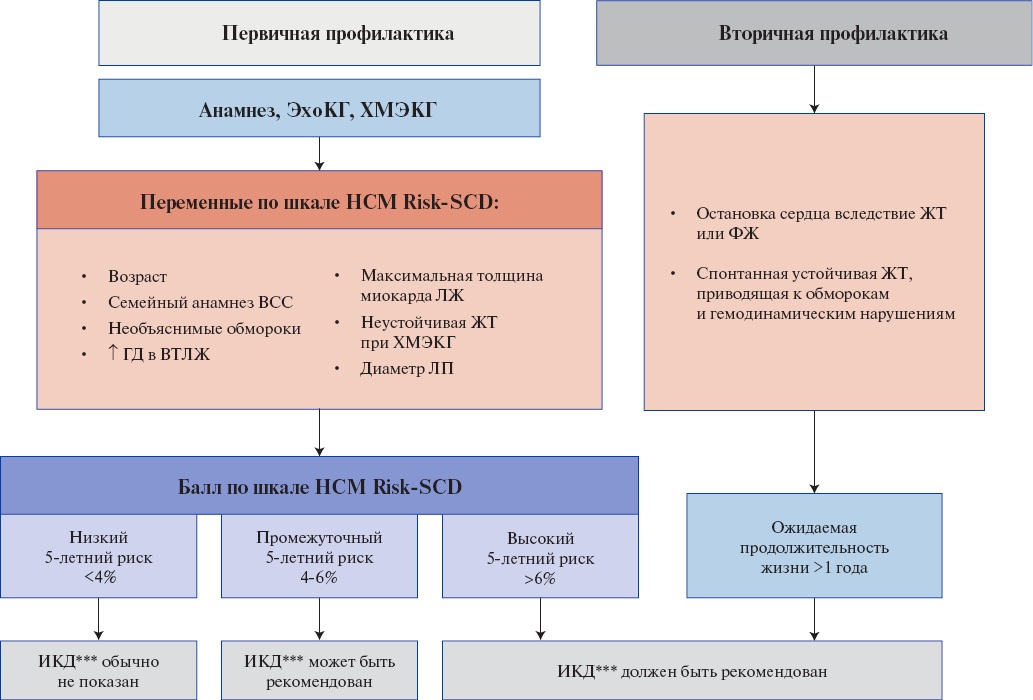
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ЖТ — желудочковая тахикардия, ИКД — имплантируемый кардиовертер-дефибриллятор, ЛЖ — левый желудочек, ЛП — левое предсердие, ФЖ — фибрилляция желудочков, ФП — фибрилляция предсердий, ХМЭКГ — холтеровское мониторирование электрокардиографии, ЭхоКГ — эхокардиография.
Приложение Б8. Алгоритм диагностики и врачебной тактики при синкопальных состояниях
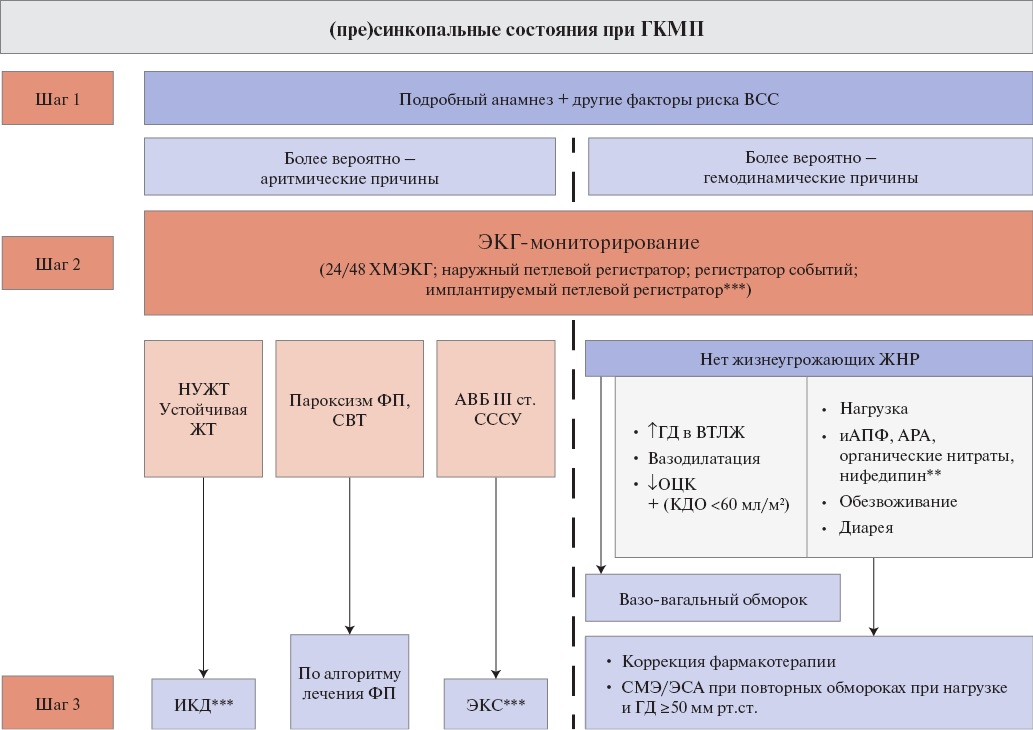
Сокращения: АВБ — атриовентрикулярная блокада, АРА — антагонисты рецепторов к ангиотензину II, ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, ЖНР — желудочковые нарушения ритма, ЖТ — желудочковая тахикардия, иАПФ — ингибиторы ангиотензинпревращающего фермента, ИКД — имплантируемый кардиовертер-дефибриллятор, КДО — конечно-диастолический объем, НУЖТ — неустойчивая желудочковая тахикардия, ОЦК — объем циркулирующей крови, СВТ — суправентрикулярная тахикардия, СМЭ — септальная миоэктомия, СССУ — синдром слабости синусового узла, ФП — фибрилляция предсердий, ХМЭКГ — холтеровское мониторирование электрокардиографии, ЭКГ — электрокардиография, ЭКС — электрокардиостимулятор, ЭСА — этаноловая септальная аблация.
Приложение Б9. Алгоритм врачебной тактики в зависимости от стадии ГКМП и варианта клинического течения
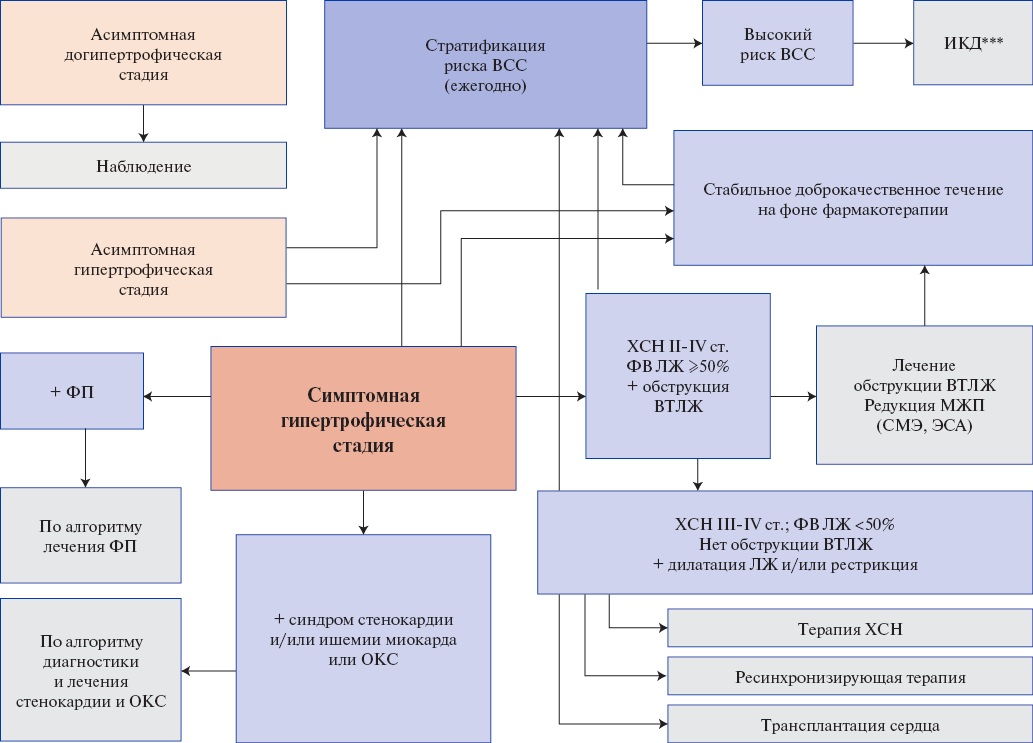
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ИКД — имплантируемый кардиовертер-дефибриллятор, МЖП — межжелудочковая перегородка, ЛЖ — левый желудочек, ОКС — острый коронарный синдром, РСТ — ресинхронизирующая терапия, СМЭ — септальная миоэктомия, ФВ — фракция выброса, ФП — фибрилляция предсердий, ХСН — хроническая сердечная недостаточность, ЭСА — этаноловая септальная аблация.
Приложение Б10. Показания к редукции МЖП (СМЭ/ЭСА)
|
Критерии |
Показания |
|
Клинические |
ХСН III-IV функционального класса NYHA с ФВ ЛЖ ≥50% и/или наличие других тяжелых симптомов (обмороки, предобморочные состояния, синдром стенокардии), существенно ограничивающих повседневную активность, несмотря на оптимальную медикаментозную терапию |
|
Гемодинамические |
Обструктивная форма ГКМП (в покое или индуцируемая) с ГД в ВТЛЖ ≥50 мм рт.ст., которая ассоциирована с гипертрофией МЖП и передне-систолическим движением створки митрального клапана, другими аномалиями аппарата МК (хорды, папиллярных мышц) и рефрактерная к проводимой терапии в полном объеме |
|
Анатомические |
Толщина МЖП, достаточная для безопасного и эффективного выполнения операции или процедуры (по мнению оператора), состояние аппарата МК и подклапанных структур, сочетанные аномалии коронарных артерий |
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, ЛЖ — левый желудочек, МЖП — межжелудочковая перегородка, МК — митральный клапан, ФВ — фракция выброса, ХСН — хроническая сердечная недостаточность, NYHA — Нью-Йоркская ассоциация сердца.
Приложение Б11. Сравнение СМЭ и ЭСА (адаптировано из [392])
|
Критерии |
СМЭ |
ЭСА |
|
Локализация гипертрофированного отдела МЖП |
Субаортальная, среднежелудочковая, апикальная |
Субаортальная Среднежелудочковая (в отдельных Центрах) |
|
Степень гипертрофии |
От >20 мм до экстремальной гипертрофии МЖП >30 мм |
Гипертрофия МЖП <30 мм |
|
Механизм повышения ГД и недостаточность МК |
Не ассоциированное с ПСД МК и ассоциированное с ПСД МК |
Ассоциированное с ПСД МК |
|
Коморбидная патология, требующая хирургического вмешательства |
Подклапанная мембрана, аортальный стеноз, ИБС, многососудистое поражение |
ИБС, однососудистое поражение |
|
Возраст пациентов |
Подростки и молодые взрослые |
Взрослые |
|
Сложность процедуры |
Наиболее часто встречающиеся осложнения СМЭ: дефект МЖП, АВБ и остаточная обструкция ВТЛЖ |
Менее агрессивная |
|
Постпроцедурный риск зависимости от кардиостимулятора |
2-10% До 50% с исходной БПНПГ |
10-20% До 50% с исходной БЛНПГ |
|
Клиническая практика |
>50 лет |
>20 лет |
|
Доступность |
Недостаточная, небольшое количество центров с опытом |
Достаточная, но небольшое количество центров с опытом |
|
Сопоставимые показатели выживаемости и клинико-гемодинамическое улучшение после ЭСА и СМЭ были получены в нерандомизированных обсервационных исследованиях |
||
Сокращения: АВБ — атриовентрикулярная блокада, БЛНПГ — блокада левой ножки пучка Гиса, БПНПГ — блокада правой ножки пучка Гиса, ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ИБС — ишемическая болезнь сердца, МЖП — межжелудочковая перегородка, МК — митральный клапан, ПСД — переднее систолическое движение, СМЭ — септальная миоэктомия, ЭСА — этаноловая септальная аблация.
Приложение Б12. Врачебная тактика ведения беременности и родоразрешения в зависимости от степени обструкции ВТЛЖ (по [495])
|
Степень обструкции ВТЛЖ |
Врачебная тактика |
|
Необструктивная ГКМП (ГД в ВТЛЖ <30 мм рт.ст.) или небольшая степень обструкции |
Пролонгирование беременности может быть разрешено при условии постоянного наблюдения кардиологом (не реже 1 раза в мес.). Госпитализация осуществляется в сроки, рекомендованные для всех пациенток с сердечно-сосудистыми заболеваниями, при необходимости — чаще. Роды через естественные родовые пути |
|
Средняя степень обструкции ВТЛЖ (ГД 30-50 мм рт.ст.) |
Вопрос о вынашивании беременности решается индивидуально: необходимо постоянное наблюдение кардиолога (терапевта) и акушера-гинеколога. Сроки госпитализации те же; также в любой срок при ухудшении состояния и развитии осложнений. Роды проводят через естественные родовые пути с исключением потуг |
|
Тяжелая степень обструкции ВТЛЖ (ГД ≥50 мм рт.ст.) |
Вынашивание беременности и роды категорически противопоказаны. При отказе женщины от прерывания беременности показана госпитализация практически на весь срок беременности. Родоразрешение проводят путем операции кесарева сечения. Использование эпидуральной анестезии с осторожностью из-за опасности артериальной гипотензии |
Сокращения: ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия.
Приложение Б13. Учреждение для ведения беременных с ГКМП
|
ВОЗ II (бессимптомные или малосимптомные пациентки) |
ВОЗ III (симптомные пациентки с ГКМП) |
|
|
Ведение беременных |
Региональный перинатальный центр |
Экспертный центр. Перинатальный центр 3 уровня |
|
Частота осмотров |
1 раз в 2 мес. |
Каждый месяц или 2 раза в мес. |
|
Учреждение для родоразрешения |
Региональный перинатальный центр |
Экспертный центр. Перинатальный центр 3 уровня |
Сокращения: ВОЗ — Всемирная организация здравоохранения, ГКМП — гипертрофическая кардиомиопатия.
Приложение В. Информация для пациентов
Общие рекомендации по образу жизни (адаптировано из [3])
|
Область |
Рекомендации |
|
Нагрузки |
Пациентам следует избегать соревновательного спорта, но по возможности поддерживать обычный образ жизни. В отсутствии симптомов и факторов риска ВСС пациенты с ГКМП могут участвовать в физической активности от небольшой до средней степени интенсивности, в соответствии с рекомендациями кардиолога |
|
Диета |
Пациентам следует стараться поддерживать нормальный вес тела. Прием большого объема пищи может вызвать боли в грудной клетке, особенно у пациентов с обструкцией ВТЛЖ. Целесообразно частое дробное питание. Запоры — частый побочный эффект верапамила**, должны контролироваться диетой и/или слабительными средствами |
|
Профессия |
Большинство пациентов с ГКМП могут продолжать обычную трудовую деятельность. Уровень физических усилий на работе должен соответствовать клиническому статусу пациента. Для некоторых видов деятельности (пилотирование, военная служба) существуют строгие ограничения при приеме на работу |
|
Курение |
Нет данных о связи табакокурения и ГКМП, но пациентам необходимо предоставить информацию о рисках для здоровья, связанных с курением |
|
Сексуальная активность |
У пациентов должна быть возможность обсудить интересующие их вопросы сексуальной активности. Пациенты после установления диагноза часто испытывают беспокойство, депрессию и страх передать заболевание потомству. Пациентам следует знать о влиянии принимаемых лекарственных препаратов на их сексуальную активность. Пациентам следует избегать приема ингибиторов фосфодиэстеразы, особенно при наличии обструкции ВТЛЖ. |
|
Вождение автомобиля |
Большинство пациентов могут получать водительские права и продолжать водить машину, если у них нет инвалидизирующих симптомов |
|
Вакцинация |
При отсутствии противопоказаний рекомендована ежегодная вакцинация от гриппа |
|
Лекарственные препараты |
Пациентам следует знать о принимаемых ими лекарственных препаратах, их побочных эффектах и межлекарственном взаимодействии. По возможности следует избегать приема периферических вазодилататоров, особенно при обструкции ВТЛЖ |
|
Страхование жизни |
Диагноз ГКМП может привести к затруднениям при страховании жизни |
|
Авиаперелеты |
Большинство бессимптомных пациентов или с незначительной симптоматикой могут безопасно совершать авиаперелеты |
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГКМП — гипертрофическая кардиомиопатия.
Приложение Г1-ГN. Шкалы оценки, вопросники и другие оценочные инструменты состояния пациента, приведенные в клинических рекомендациях
Приложение Г1. Шкала прогнозирования вероятности обнаружения генетических вариантов при ГКМП (адаптировано из [54])
Название на русском языке: Шкала прогнозирования вероятности обнаружения генетических вариантов при ГКМП
Оригинальное название (если есть): нет
Тип (подчеркнуть): шкала оценки, индекс, вопросник, другое (уточнить).
Назначение: клинический инструмент для прогнозирования вероятности обнаружения генетических вариантов при ГКМП
Содержание (шаблон):
|
Переменная |
Баллы |
|
|
Возраст, лет |
20 |
0 |
|
20-29 |
-1 |
|
|
30-39 |
-2 |
|
|
40-49 |
-3 |
|
|
50-59 |
-4 |
|
|
60-69 |
-5 |
|
|
70-79 |
-6 |
|
|
80 |
-7 |
|
|
Женщины |
4 |
|
|
Артериальная гипертензия |
-4 |
|
|
"Двояковыпуклая" форма МЖП (англ. "reverse curve") |
5 |
|
|
Соотношение толщины МЖП/задней стенки ЛЖ |
1,46 |
0 |
|
1,47-1,70 |
1 |
|
|
1,71-1,92 |
2 |
|
|
1,93-2,26 |
3 |
|
|
2,27 |
4 |
|
Ключ (интерпретация):
|
сумма баллов ≤2 предсказывает низкую вероятность обнаружения генетических вариантов в причинных генах, наиболее распространенных при ГКМП |
Сокращения: ГКМП — гипертрофическая кардиомиопатия, ЛЖ — левый желудочек, МЖП — межжелудочковая перегородка.
Приложение Г2. HCM Risk-SCD. Шкала оценки риска ВСС у пациентов c ГКМП (европейская модель) (адаптировано из [233][358])
Название на русском языке: HCM Risk-SCD. Шкала оценки риска ВСС у пациентов с ГКМП (европейская модель).
Оригинальное название (если есть): HCM Risk-SCD
Тип (подчеркнуть): шкала оценки, индекс, вопросник, другое (уточнить).
Назначение: клинический инструмент для прогнозирования риска ВСС у пациентов с ГКМП.
Содержание (шаблон):
|
Шкала риска ВСС HCM Risk-SCD (европейская модель) |
|
Показывает лучшие результаты у пациентов ГКМП с высоким риском ВСС |
|
Калькулятор 5-летнего риска ВСС на основе модели, в которой учитываются следующие параметры: 1. Семейная история ВСС 2. Синкопы 3. Неустойчивая желудочковая тахикардия 4. Макс. толщина стенки ЛЖ 5. Возраст 6. Диаметр ЛП 7. ГД в ВТЛЖ |
|
Параметры вносятся в "Калькулятор" на сайте http://doc2do.com/hcm/webHCM.html |
Ключ (интерпретация)
|
ИКД*** показан, если риск ≥6%; ИКД*** может быть рассмотрен, если риск ≥4%, но <6%; ИКД***, как правило, не показан, если риск <4% |
|
Шкала HCM Risk-SCD была валидирована для пациентов с предшествующей редукцией МЖП методом ЭСА [525] |
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГД — градиент давления, ГКМП — гипертрофическая кардиомиопатия, ИКД — имплантируемый кардиовертер-дефибриллятор, ЛЖ — левый желудочек, ЛП — левое предсердие, МЖП — межжелудочковая перегородка, ЭСА — этаноловая септальная аблация.
Приложение Г3. Шкала оценки риска ВСС у пациентов с ГКМП (американская модель) (адаптировано из [489])
Название на русском языке: Шкала оценки риска ВСС у пациентов с ГКМП (американская модель).
Оригинальное название (если есть): нет
Тип (подчеркнуть): шкала оценки, индекс, вопросник, другое (уточнить).
Назначение: клинический инструмент для прогнозирования риска ВСС у пациентов с ГКМП.
Содержание (шаблон):
|
Шкала риска ВСС (американская модель) |
|
|
Факторы риска ВСС |
|
|
Основные факторы риска ВСС |
1. Семейная история ВСС вследствие ГКМП 2. Максимальная толщина стенки ЛЖ ≥30 мм 3. Необъяснимая синкопа в течение последних 6 мес. (этиология синкопы не вазовагальная или обусловленная обструкцией ВТЛЖ) 4. Систолическая дисфункция (ФВ ЛЖ <50%) 5. Апикальная аневризма ЛЖ |
|
Дополнительные факторы риска ВСС |
1. ПНГ при МРТ ≥15% массы ЛЖ 2. НУЖТ ≥3 комплексов с частотой сокращений ≥120 в мин при амбулаторном мониторировании ЭКГ |
Сокращения: ВСС — внезапная сердечная смерть, ВТЛЖ — выходной тракт левого желудочка, ГКМП — гипертрофическая кардиомиопатия, ЛЖ — левый желудочек, МРТ — магнитно-резонансная томография, НУЖТ — неустойчивая желудочковая тахикардия, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ФВ — фракция выброса, ЭКГ — электрокардиография.
Ключ (интерпретация) к имплантации ИКД***:
|
Факторы риска ВСС (американская модель) |
Имплантация ИКД*** |
Класс по AHA/ACC |
|
Предотвращенная ВСС (выжившие вследствие ЖТ или ФЖ) после остановки сердца |
показана |
I |
|
Синкопа, вызванная устойчивой ЖТ или спонтанной гемодинамически значимой ЖТ |
показана |
I |
|
Наличие хотя бы 1 из следующих факторов: 1. Семейная история ВСС вследствие ГКМП 2. 1 или более синкоп в течение последних 6 мес. аритмического генеза 3. Макс. толщина стенки ЛЖ ≥30 мм 4. Апикальная аневризма ЛЖ 5. Систолическая дисфункция (ФВ ЛЖ <50%) |
показана |
IIа |
|
У пациентов без основных факторов риска ВСС, но при наличии дополнительно распространенного ПНГ при МРТ |
рассмотреть возможность |
IIb |
|
У пациентов без основных факторов риска ВСС, но если дополнительно регистрируется НУЖТ при амбулаторном мониторировании ЭКГ |
рассмотреть возможность |
IIb |
Сокращения: ВСС — внезапная сердечная смерть, ГКМП — гипертрофическая кардиомиопатия, ЖТ — желудочковая тахикардия, ИКД — имплантируемый кардиовертер-дефибриллятор, ЛЖ — левый желудочек, МРТ — магнитно-резонансная томография, НУЖТ — неустойчивая желудочковая тахикардия, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества, ФВ — фракция выброса, ФЖ — фибрилляция желудочков, ЭКГ — электрокардиография, AHA — American Heart Association (Американская ассоциация сердца), ACC — American College of Cardiology (Американская коллегия кардиологов).
Приложение Г4. CHA2DS2-VASс. Шкала оценки риска тромбоэмболических осложнений у пациентов с ФП/ТП (адаптировано из [519])
Тип (подчеркнуть): шкала оценки, индекс, вопросник, другое (уточнить).
Назначение: клинический инструмент для прогнозирования риска ишемического инсульта и системного тромбоэмболизма при ФП.
Содержание (шаблон):
|
Фактор риска |
Баллы |
|
Инсульт, транзиторная ишемическая атака или артериальная тромбоэмболия в анамнезе |
2 |
|
Возраст ≥75 лет |
2 |
|
Артериальная гипертензия |
1 |
|
Сахарный диабет |
1 |
|
Застойная сердечная недостаточность/дисфункция левого желудочка (в частности, фракция выброса ≤40%) |
1 |
|
Сосудистое заболевание (инфаркт миокарда в анамнезе, периферический атеросклероз, атеросклеротические бляшки в аорте) |
1 |
|
Возраст 65-74 года |
1 |
|
Женский пол |
1 |
Ключ (интерпретация):
|
Сумма баллов по шкале CHA2DS2-VASc |
Ожидаемая частота инсультов за год |
|
0 |
0% |
|
1 |
1,3% |
|
2 |
2,2% |
|
3 |
3,2% |
|
4 |
4,0% |
|
5 |
6,7% |
|
6 |
9,8% |
|
7 |
9,6% |
|
8 |
6,7% |
|
9 |
15,2% |
Приложение Г5. HAS-BLED. Шкала оценки риска кровотечения (адаптировано из [445][520])
Название на русском языке: HAS-BLED. Шкала оценки риска большого кровотечения в течение 1 года у пациентов с ФП/ТП, получающих антикоагулянтную терапию в сочетании с ингибиторами агрегации тромбоцитов или без.
Оригинальное название (если есть): HAS-BLED
Тип (подчеркнуть): шкала оценки, индекс, вопросник, другое (уточнить).
Назначение: клинический инструмент для прогнозирования риска большого кровотечения в течение 1 года
Содержание (шаблон):
|
Буква |
Фактор риска |
Баллы |
|
H |
Артериальная гипертензия |
1 |
|
A |
Нарушение функции печени или почек |
1 или 2 |
|
S |
Инсульт в анамнезе |
1 |
|
B |
Кровотечения в анамнезе |
1 |
|
L |
Лабильность международного нормализованного отношения |
1 |
|
E |
Возраст (≥65 лет) |
1 |
|
D |
Злоупотребление алкоголем или препаратами, повышающими риск кровотечений |
1 или 2 |
Ключ (интерпретация)
|
Сумма баллов по шкале HAS-BLED |
Риск большого кровотечения в течение 1 года |
|
1-2 |
Низкий риск кровотечения |
|
≥3 |
Высокий риск кровотечения |
Приложение Г6. QALE. Шкала для дифференциальной диагностики ATTR с помощью контрастной МРТ сердца (адаптировано из [285])
Название на русском языке: QALE
Оригинальное название (если есть): QALE Score
Тип (подчеркнуть): шкала оценки, индекс, вопросник, другое (уточнить).
Назначение: клинический инструмент для дифференциальной диагностики ATTR и AL-амилоидоза.
Содержание (шаблон):
|
Оценивается характер ПНГ в стенках левого желудочка на трех уровнях: апикальном, среднем и базальном с присвоением определенного количества баллов в зависимости от паттерна ПНГ как указано на рисунке
|
||
|
Максимальной возможное количество баллов при оценке стенок левого желудочка — 12 (4×3)
|
||
|
Если имеется любое ПНГ в стенках правого желудочка, то к шкале добавляется 6 баллов |
||
|
Общее возможное количество баллов по шкале QALE c учетом вовлечения правого желудочка — 18 (12+6) |
||
|
Дополнительные данные: |
||
|
Семиотика при МРТ |
AL-амилоидоз |
Транстиретиновый амилоидоз |
|
Индексированная масса миокарда ЛЖ |
Умеренно повышена |
Значительно повышена • 100 г/м² |
|
Утолщение межжелудочковой и межпредсердной перегородки |
Менее выражено |
Более выражено |
|
ПНГ |
• Менее выражено • Часто диффузный субэндокардиальный паттерн • QALE <13 баллов |
• Более выражено • Часто диффузный или трансмуральный паттерн накопления • QALE >13 баллов |
|
Нативное Т1 — картирование |
• 1050-1150 мс • Относительно небольшое повышение времени Т1 |
• 1050-1150 мс • Более выраженное повышение времени Т1 |
|
Значение внеклеточного объема ECV |
• Повышение >40% • Относительно небольшое повышение ECV |
• Повышение >40% • Более выраженное повышение ECV |
Сокращения: ЛЖ — левый желудочек, МРТ — магнитно-резонансная томография, ПНГ — позднее накопление гадолиний-содержащего контрастного вещества.
Ключ (интерпретация):
|
Сумма баллов по шкале QALE |
Диагноз |
|
QALE <13 баллов |
AL-амилоидоз |
|
QALE >13 баллов |
Транстиретиновый амилоидоз |
Список литературы
1. Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2020;76(25): e159-240. doi:10.1016/j.jacc.2020.08.045.
2. Ommen SR, Ho CY, Asif IM, et al. Writing Committee Members. 2024 AHA/ACC/AMSSM/ HRS/PACES/SCMR Guideline for the Management of Hypertrophic Cardiomyopathy: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2024;83(23):2324-405. doi:10.1016/j.jacc.2024.02.014.
3. Elliot P, Zamorano JL, Anastasakis A, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: The task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733-79. doi:10.1093/eurheartj/ehu284.
4. Lipshultz SE, Law YM, Asante-Korang A, et al. Cardiomyopathy in Children: Classification and Diagnosis: A Scientific Statement From the American Heart Association. Circulation. 2019;140(1): E9-68. doi:10.1161/CIR.0000000000000682.
5. Bogle C, Colan SD, Miyamoto SD, et al. Treatment Strategies for Cardiomyopathy in Children: A Scientific Statement From the American Heart Association. Circulation. 2023;148(2): Epub ahead of print. doi:10.1161/CIR.0000000000001151.
6. Gurschenkov A, Andreeva S, Zaitsev V, et al. Septal Myectomy in Patients with Hypertrophic Cardiomyopathy and Nonclassical Anderson-Fabry Disease. J Cardiovasc Dev Dis. 2024;11(9):293. doi:10.3390/JCDD11090293.
7. Colan SD, Lipshultz SE, Lowe AM, et al. Epidemiology and cause-specific outcome of hypertrophic cardiomyopathy in children: findings from the Pediatric Cardiomyopathy Registry. Circulation. 2007;115(6):773-81. doi:10.1161/IRCULATIONAHA.106.621185.
8. Monda E, Rubino M, Lioncino M, et al. Hypertrophic Cardiomyopathy in Children: Pathophysiology, Diagnosis, and Treatment of Non-sarcomeric Causes. Front Pediatr. 2021;9:632293. doi:10.3389/FPED.2021.632293.
9. Фетисова С. Г., Мельник О. В., Фомичева Ю. В. и др. Сравнительная информативность применения различных таргетных панелей при генетической диагностике гипертрофической кардиопатии у детей. Трансляционная медицина. 2025;12(1):6-14.
10. Limongelli G, Adorisio R, Baggio C, et al. Diagnosis and Management of Rare Cardiomyopathies in Adult and Paediatric Patients. A Position Paper of the Italian Society of Cardiology (SIC) and Italian Society of Paediatric Cardiology (SICP). Int J Cardiol. 2022;357:55-71. doi:10.1016/J.IJCARD.2022.03.050.
11. Alfares AA, Kelly MA, McDermott G, et al. Results of clinical genetic testing of 2,912 probands with hypertrophic cardiomyopathy: Expanded panels offer limited additional sensitivity. Genet Med. 2015;17(11):880-8. doi:10.1038/gim.2014.205.
12. Ingles J, Sarina T, Yeates L, et al. Clinical predictors of genetic testing outcomes in hypertrophic cardiomyopathy. Genet Med. 2013;15(12):972-7. doi:10.1038/GIM.2013.44.
13. Geisterfer-Lowrance AAT, Kass S, Tanigawa G, et al. A molecular basis for familial hypertrophic cardiomyopathy: a beta cardiac myosin heavy chain gene missense mutation. Cell. 1990;62(5):999-1006. doi:10.1016/0092-8674(90)90274-I.
14. Seidman JG, Seidman C. The genetic basis for cardiomyopathy: from mutation identification to mechanistic paradigms. Cell. 2001;104(4):557-67. doi:10.1016/S00928674(01)00242-2.
15. Seidman CE, Seidman JG. Identifying sarcomere gene mutations in hypertrophic cardiomyopathy: a personal history. Circ Res. 2011;108(6):743-50. doi:10.1161/CIRCRESAHA.110.223834.
16. Liew AC, Vassiliou VS, Cooper R, Raphael CE. Hypertrophic Cardiomyopathy-Past, Present and Future. J Clin Med. 2017;6(12):118. doi:10.3390/JCM6120118.
17. Maron BA, Wang RS, Carnethon MR, et al. What Causes Hypertrophic Cardiomyopathy? Am J Cardiol. 2022;179:74-82. doi:10.1016/j.amjcard.2022.06.017.
18. Maron BJ, Ommen SR, Semsarian C, et al. Hypertrophic cardiomyopathy: present and future, with translation into contemporary cardiovascular medicine. J Am Coll Cardiol. 2014;64(1):83-99. doi:10.1016/J.JACC.2014.05.003.
19. Shlyakhto EV, Semernin EN, Gudkova AYa, Kostareva AA. Primary cardiomyopathies, modern concept. Therapeutic Archive. 2005;77(12):77-83. (In Russ.) Шляхто Е. В., Семернин Е. Н., Гудкова А. Я., Костарева А. А. Первичные кардиомиопатии, современное представление. Терапевтический архив. 2005;77(12):77-83.
20. Gersh BJ, Maron BJ, Bonow RO, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: Executive summary: A report of the American College of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2011;124(24):2761-96. doi:10.1161/CIR.0b013e318223e230.
21. Kelly MA, Caleshu C, Morales A, et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: Recommendations by ClinGen’s Inherited Cardiomyopathy Expert Panel. Genet Med. 2018;20(3):351-9. doi:10.1038/gim.2017.218.
22. Lopes LR, Murphy C, Syrris P, et al. Use of high-throughput targeted exome-sequencing to screen for copy number variation in hypertrophic cardiomyopathy. Eur J Med Genet. 2015;58(11):611-6. doi:10.1016/j.ejmg.2015.10.001.
23. Maron BJ, Maron MS, Maron BA, Loscalzo J. Moving Beyond the Sarcomere to Explain Heterogeneity in Hypertrophic Cardiomyopathy: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73(15):1978-86. doi:10.1016/j.jacc.2019.01.061.
24. Zhou N, Qin S, Liu Y, et al. Whole-exome sequencing identifies rare compound heterozygous mutations in the MYBPC3 gene associated with severe familial hypertrophic cardiomyopathy. Eur J Med Genet. 2018;61(8):434-41. doi:10.1016/j.ejmg.2018.03.001.
25. Давыдова В. Г., Гудкова А. Я., Крутиков А. Н. и др. Клинические, морфологические и генетические характеристики пациентов молодого возраста с гипертрофической кардиомиопатией, имеющих показания к имплантации кардиовертерадефибриллятора. Российский кардиологический журнал. 2024;29(11):5994. doi:10.15829/1560-4071-2024-5994.
26. Kostareva A, Gudkova A, Sjöberg G, et al. Deletion in TNNI3 gene is associated with restrictive cardiomyopathy. Int J Cardiol. 2009;131(3):410-2. doi:10.1016/j.ijcard.2007.07.108.
27. Туральчук М. В., Новик Г. А., Гудкова А. Я. Особенности течения кардиомиопатий с рестриктивным фенотипом, обусловленных мутациями генов сердечного тропонина I и десмина, и алгоритмы их диагностики. Педиатрическая фармакология. 2011;8(4):112-6.
28. Ho CY, Day SM, Colan SD, et al. The burden of early phenotypes and the influence of wall thickness in hypertrophic cardiomyopathy mutation carriers: Findings from the HCMNet study. JAMA Cardiol. 2017;2(4):419-28. doi:10.1001/jamacardio.2016.5670.
29. Tsaturyan AK, Zaklyazminskaya EV, Polyak ME, et al. De Novo Asp219Val Mutation in Cardiac Tropomyosin Associated with Hypertrophic Cardiomyopathy. Int J Mol Sci. 2022;24(1):18. doi:10.3390/IJMS24010018.
30. Ansari-Lari MA, Ali SZ. Fine-Needle Aspiration of Abdominal Fat Pad for Amyloid Detection: A Clinically Useful Test? Diagn Cytopathol. 2004;30(3):178-81. doi:10.1002/dc.10370.
31. Canepa M, Sorensen LL, Pozios I, et al. Comparison of clinical presentation, left ventricular morphology, hemodynamics, and exercise tolerance in obese versus nonobese patients with hypertrophic cardiomyopathy. Am J Cardiol. 2013;112(8):1182-9. doi:10.1016/j. amjcard.2013.05.070.
32. Hodatsu A, Konno T, Hayashi K, et al. Compound heterozygosity deteriorates phenotypes of hypertrophic cardiomyopathy with founder MYBPC3 mutation: Evidence from patients and zebrafish models. Am J Physiol — Hear Circ Physiol. 2014;307(11): H1594-604. doi:10.1152/ajpheart.00637.2013.
33. Charron P, Arad M, Arbustini E, et al. Genetic counselling and testing in cardiomyopathies: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2010;31(22):2715-28. doi:10.1093/eurheartj/ehq271.
34. Finocchiaro G, Magavern E, Sinagra G, et al. Impact of demographic features, lifestyle, and comorbidities on the clinical expression of hypertrophic cardiomyopathy. J Am Heart Assoc. 2017;6(12): e007161. doi:10.1161/JAHA.117.007161.
35. Blagova O, Alieva I, Kogan E, et al. Mixed Hypertrophic and Dilated Phenotype of Cardiomyopathy in a Patient With Homozygous In-Frame Deletion in the MyBPC3 Gene Treated as Myocarditis for a Long Time. Front Pharmacol. 2020;11:579450. doi:10.3389/FPHAR.2020.579450.
36. Pasquale F, Syrris P, Kaski JP, et al. Long-term outcomes in hypertrophic cardiomyopathy caused by mutations in the cardiac troponin T gene. Circ Cardiovasc Genet. 2012;5(1):10-7. doi:10.1161/CIRCGENETICS.111.959973.
37. Maron BJ, Kragel AH, Roberts WC. Sudden death in hypertrophic cardiomyopathy with normal left ventricular mass. Br Heart J. 1990;63(5):308-10. doi:10.1136/HRT.63.5.308.
38. Walsh R, Buchan R, Wilk A, et al. Defining the genetic architecture of hypertrophic cardiomyopathy: re-evaluating the role of non-sarcomeric genes. Eur Heart J. 2017;38(46):3461-8. doi:10.1093/EURHEARTJ/EHW603.
39. Marian AJ, Braunwald E. Hypertrophic cardiomyopathy: Genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ Res. 2017;121(7):749-70. doi:10.1161/CIRCRESAHA.117.311059.
40. Ingles J, Goldstein J, Thaxton C, et al. Evaluating the Clinical Validity of Hypertrophic Cardiomyopathy Genes. Circ Genomic Precis Med. 2019;12(2):57-64. doi:10.1161/CIRCGEN.119.002460.
41. Bagnall RD, Ingles J, Dinger ME, et al. Whole Genome Sequencing Improves Outcomes of Genetic Testing in Patients With Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2018;72(4):419-29. doi:10.1016/J.JACC.2018.04.078.
42. Maron BJ. Clinical Course and Management of Hypertrophic Cardiomyopathy. N Engl J Med. 2018;379(7):655-68. doi:10.1056/NEJMRA1710575.
43. Aslam F, Haque A, Foody JA, Shirani J. The frequency and functional impact of overlapping hypertension on hypertrophic cardiomyopathy: a single-center experience. J Clin Hypertens (Greenwich). 2010;12(4):240-5. doi:10.1111/J.1751-7176.2009.00251.X.
44. Timmis A, Gale CP, Flather M, et al. Cardiovascular disease statistics from the European atlas: inequalities between highand middle-income member countries of the ESC. Eur Hear Journal Qual Care Clin Outcomes. 2018;4(1):1-3. doi:10.1093/EHJQCCO/QCX045.
45. Lopes LR, Losi M-A, Sheikh N, et al. Association between common cardiovascular risk factors and clinical phenotype in patients with hypertrophic cardiomyopathy from the European Society of Cardiology (ESC) EurObservational Research Programme (EORP) Cardiomyopathy/Myocarditis registry. Eur Hear Journal Qual Care Clin Outcomes. 2022;9(1):42-53. doi:10.1093/EHJQCCO/QCAC006.
46. De La Rosa A, Shah M, Shiota T, et al. Comparing echocardiographic characteristics in genotype positive-phenotype positive hypertrophic cardiomyopathy and hypertensive left ventricular hypertrophy. Eur Hear Journal Cardiovasc Imaging. 2022;23(3):340-8. doi:10.1093/EHJCI/JEAB217.
47. Gil TCP, Castier MB, Gondar AFP, et al. Strain Analysis of Left Ventricular Function in the Association of Hypertrophic Cardiomyopathy and Systemic Arterial Hypertension. Arq Bras Cardiol. 2019;113(4):677-84. doi:10.5935/ABC.20190176.
48. Harper AR, Goel A, Grace C, et al. Common genetic variants and modifiable risk factors underpin hypertrophic cardiomyopathy susceptibility and expressivity. Nat Genet. 2021;53(2):135-42. doi:10.1038/S41588-020-00764-0.
49. Wang Z, Zheng Y, Ruan H, et al. The impact of hypertension on the prognosis of patients with hypertrophic cardiomyopathy: a single-center retrospective study. PeerJ. 2023;11: e14614. doi:10.7717/PEERJ.14614.
50. Zhang Y, Liu M-H, Zhang M, et al. Different clinical characteristics and outcomes of hypertrophic cardiomyopathy with and without hypertension: seeking the truth. J Geriatr Cardiol. 2023;20(2):109. doi:10.26599/1671-5411.2023.02.007.
51. Gruner C, Ivanov J, Care M, et al. Toronto hypertrophic cardiomyopathy genotype score for prediction of a positive genotype in hypertrophic cardiomyopathy. Circ Cardiovasc Genet. 2013;6(1):19-26. doi:10.1161/CIRCGENETICS.112.963363.
52. Ежова А. В., Зайцев В. В., Ишмухаметов Г. И. и др. Значение традиционных факторов риска сердечно-сосудистых заболеваний в фенотипических проявлениях гипертрофической кардиомиопатии. Артериальная гипертензия. 2023;29(4):371-9. doi:10.18705/1607-419X-2023-29-4-371-379.
53. Luo Q, Chen J, Zhang T, et al. Retrospective analysis of clinical phenotype and prognosis of hypertrophic cardiomyopathy complicated with hypertension. Sci Rep. 2020;10(1). doi:10.1038/S41598-019-57230-Z.
54. Ingles J, Burns C, Bagnall RD, et al. Nonfamilial Hypertrophic Cardiomyopathy: Prevalence, Natural History, and Clinical Implications. Circ Cardiovasc Genet. 2017;10(2): e001620. doi:10.1161/CIRCGENETICS.116.001620.
55. Maron BJ, Wolfson JK, Epstein SE, Roberts WC. Intramural ("small vessel") coronary artery disease in hypertrophic cardiomyopathy. J Am Coll Cardiol. 1986;8(3):545-57. doi:10.1016/S0735-1097(86)80181-4.
56. Rowin EJ, Maron BJ, Maron MS. The Hypertrophic Cardiomyopathy Phenotype Viewed Through the Prism of Multimodality Imaging: Clinical and Etiologic Implications. JACC Cardiovasc Imaging. 2020;13(9):2002-16. doi:10.1016/J.JCMG.2019.09.020.
57. Bonaventura J, Rowin EJ, Maron MS, Maron BJ. Is Hypertrophic Cardiomyopathy Always a Familial and Inherited Disease? J Am Heart Assoc. 2023;12(12): e028974. doi:10.1161/JAHA.122.028974.
58. Burton D, Abdulrazzak H, Knott A, et al. Two mutations in troponin I that cause hypertrophic cardiomyopathy have contrasting effects on cardiac muscle contractility. Biochem J. 2002;362(2):443-51. doi:10.1042/0264-6021:3620443.
59. Бокерия Л. А., Гудкова А. Я., Созин С. Е. и др. Экспрессия генов матриксной металлопротеиназы-1 (ММР-1), тканевого ингибитора матриксных металлопротеиназ-1 (TIMP-1), коллагена I и III типов в миокарде больных идиопатической гипертрофической кардиомиопатией. Бюллетень НЦССХ им. А. Н. Бакулева РАМН. 2005;6(4):35-42.
60. Gudkova AYa. Characteristics of the course of obstructive hypertrophic cardiomyopathy in adults (literature review and own research results). Arterial hypertension. 2008;14(2, Appendix 2):39-49. (In Russ.) Гудкова А. Я. Характеристика течения обструктивной гипертрофической кардиомиопатии у взрослых (обзор литературы и результаты собственных исследований). Артериальная гипертензия. 2008;14(2, Приложение 2):39-49.
61. Gudkova AYa, Rybakova MG, Bokeria LA, Shlyakhto EV. Hypertrophic cardiomyopathy. Clinical and morphological comparisons. Pathology archive. 2012;74(4):8-11. (In Russ.) Гудкова А. Я., Рыбакова М. Г., Бокерия Л. А., Шляхто Е. В. Гипертрофическая кардиомиопатия. Клинико-морфологические сопоставления. Архив патологии. 2012;74(4):8-11.
62. Гудкова А. Я., Шляхто Е. В. Клеточные механизмы гипертрофии миокарда при гипертрофической кардиомиопатии и эссенциальной артериальной гипертензии. Артериальная гипертензия. 2008;14(4):364-80.
63. Philipson DJ, DePasquale EC, Yang EH, Baas AS. Emerging pharmacologic and structural therapies for hypertrophic cardiomyopathy. Heart Fail Rev. 2017;22(6):879-88. doi:10.1007/s10741-017-9648-x.
64. Roberts R, Sigwart U. Current concepts of the pathogenesis and treatment of hypertrophic cardiomyopathy. Circulation. 2005;112(2):293-6. doi:10.1161/01.CIR.0000146788.30724.0A.
65. Зайцев В. В., Гурщенков А. В., Митрофанова Л. Б. и др. Клиническое значение различных методов оценки миокардиального фиброза при гипертрофической кардиомиопатии. Кардиология. 2020;60(3):44-50. doi:10.18087/cardio.2020.3.n561.
66. Arbelo E, Protonotarios A, Gimeno JR, et al. 2023 ESC Guidelines for the management of cardiomyopathies: Developed by the task force on the management of cardiomyopathies of the European Society of Cardiology (ESC). Eur Heart J. 2023;44(37):3503-626. doi:10.1093/EURHEARTJ/EHAD194.
67. Arbustini E, Narula N, Dec GW, et al. The MOGE(S) classification for a phenotypegenotype nomenclature of cardiomyopathy: Endorsed by the world heart federation. J Am Coll Cardiol. 2013;62(22):2046-72. doi:10.1016/j.jacc.2013.08.1644.
68. Bokhari S, Castaño A, Pozniakoff T, et al. 99mTc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging. 2013;6(2):195-201. doi:10.1161/CIRCIMAGING.112.000132.
69. Charron P, Villard E, Sébillon P, et al. Danon’s disease as a cause of hypertrophic cardiomyopathy: A systematic survey. Heart. 2004;90(8):842-6. doi:10.1136/hrt.2003.029504.
70. Frustaci A, Chimenti C, Doheny D, Desnick RJ. Evolution of cardiac pathology in classic Fabry disease: Progressive cardiomyocyte enlargement leads to increased cell death and fibrosis, and correlates with severity of ventricular hypertrophy. Int J Cardiol. 2017;248:257-62. doi:10.1016/j.ijcard.2017.06.079.
71. Tsai SB, Seldin DC, Wu H, et al. Myocardial infarction with "clean coronaries" caused by amyloid light-chain AL amyloidosis: A case report and literature review. Amyloid. 2011;18(3):160-4. doi:10.3109/13506129.2011.571319.
72. Wilkinson JD, Lowe AM, Salbert BA, et al. Outcomes in children with Noonan syndrome and hypertrophic cardiomyopathy: A study from the Pediatric Cardiomyopathy Registry. Am Heart J. 2012;164(3):442-8. doi:10.1016/j.ahj.2012.04.018.
73. Frustaci A, Russo MA, Chimenti C. Diagnostic contribution of left ventricular endomyocardial biopsy in patients with clinical phenotype of hypertrophic cardiomyopathy. Hum Pathol. 2013;44(1):133-41. doi:10.1016/j.humpath.2012.04.023.
74. Cook A, Giunti P. Friedreich’s ataxia: Clinical features, pathogenesis and management. Br Med Bull. 2017;124(1):19-30. doi:10.1093/bmb/ldx034.
75. Dubrey SW, Hawkins PN, Falk RH. Amyloid diseases of the heart: Assessment, diagnosis, and referral. Heart. 2011;97(1):75-84. doi:10.1136/hrt.2009.190405.
76. Planté-Bordeneuve V, Said G. Familial amyloid polyneuropathy. Lancet Neurol. 2011;10(12):1086-97. doi:10.1016/S1474-4422(11)70246-0.
77. Ibrahim M, Rao C, Ashrafian H, et al. Modern Management of Systolic Anterior Motion of the Mitral Valve. Eur J Cardiothorac Surg. 2012;41:60-70.
78. Deng L, Huang X, Yang C, et al. Numerical simulation study on systolic anterior motion of the mitral valve in hypertrophic obstructive cardiomyopathy. Int J Cardiol. 2018;266:167-73. doi:10.1016/j.ijcard.2018.01.062.
79. Manabe S, Kasegawa H, Arai H, Takanashi S. Management of systolic anterior motion of the mitral valve: a mechanism-based approach. Gen Thorac Cardiovasc Surg. 2018;66(7):379-89. doi:10.1007/s11748-018-0915-0.
80. Ro R, Halpern D, Sahn DJ, et al. Vector flow mapping in obstructive hypertrophic cardiomyopathy to assess the relationship of early systolic left ventricular flow and the mitral valve. J Am Coll Cardiol. 2014;64(19):1984-95. doi:10.1016/j.jacc.2014.04.090.
81. Hymel BJ, Townsley MM. Echocardiographic assessment of systolic anterior motion of the mitral valve. Anesth Analg. 2014;118(6):1197-201. doi:10.1213/ANE.0000000000000196.
82. Sherrid MV, Gunsburg DZ, Moldenhauer S, Pearle G. Systolic anterior motion begins at low left ventricular outflow tract velocity in obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2000;36(4):1344-54. doi:10.1016/S0735-1097(00)00830-5.
83. Silbiger JJ. Abnormalities of the Mitral Apparatus in Hypertrophic Cardiomyopathy: Echocardiographic, Pathophysiologic, and Surgical Insights. J Am Soc Echocardiogr. 2016;29(7):622-39. doi:10.1016/j.echo.2016.03.003.
84. Shah JS, Esteban MTT, Thaman R, et al. Prevalence of exercise-induced left ventricular outflow tract obstruction in symptomatic patients with non-obstructive hypertrophic cardiomyopathy. Heart. 2008;94(10):1288-94. doi:10.1136/hrt.2007.126003.
85. Geske JB, Sorajja P, Ommen SR, Nishimura RA. Variability of left ventricular outflow tract gradient during cardiac catheterization in patients with hypertrophic cardiomyopathy. JACC Cardiovasc Interv. 2011;4(6):704-9. doi:10.1016/j.jcin.2011.02.014.
86. Efthimiadis GK, Pagourelias ED, Parcharidou D, et al. Clinical characteristics and natural history of hypertrophic cardiomyopathy with midventricular obstruction. Circ J. 2013;77(9):2366-74. doi:10.1253/circj.CJ-12-1561.
87. Minami Y, Kajimoto K, Terajima Y, et al. Clinical implications of midventricular obstruction in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2011;57(23):2346-55. doi:10.1016/j.jacc.2011.02.033.
88. Yan LR, Zhao SH, Wang HY, et al. Clinical characteristics and prognosis of 60 patients with midventricular obstructive hypertrophic cardiomyopathy. J Cardiovasc Med. 2015;16(11):751-60. doi:10.2459/JCM.0000000000000163.
89. Hang D, Schaff HV, Ommen SR, et al. Combined transaortic and transapical approach to septal myectomy in patients with complex hypertrophic cardiomyopathy. J Thorac Cardiovasc Surg. 2018;155(5):2096-102. doi:10.1016/j.jtcvs.2017.10.054.
90. Pacheco Claudio C, Quesada O, Pepine CJ, Noel Bairey Merz C. Why names matter for women: MINOCA/INOCA (myocardial infarction/ischemia and no obstructive coronary artery disease). Clin Cardiol. 2018;41(2):185-93. doi:10.1002/clc.22894.
91. Аверкина Н. В., Габрусенко С. А., Овчинников А. Г. и др. Оценка перфузии миокарда у больных с гипертрофической кардиомиопатией в сопоставлении с клиническими и эхокардиографическими данными. Терапевтический архив. 2003;75(4):20-5.
92. Аверков О. В., Барбараш О. Л., Бойцов С. А. и др. Дифференцированный подход в диагностике, формулировке диагноза, ведении больных и статистическом учете инфаркта миокарда 2 типа (согласованная позиция). Российский кардиологический журнал. 2019;24(6):7-21. doi:10.15829/1560-4071-2019-6-7-21.
93. Каплунова В. Ю., Шакарьянц В. А., Кожевникова М. В. и др. Гипертрофическая кардиомиопатия и ишемическая болезнь сердца. Варианты сочетанной патологии. Кардиология. 2017;57(12):16-24.
94. Костин С. И. Морфологические и морфометрические особенности гипертрофической кардиомиопатии. Архив патологии. 1989;51(1):47-52.
95. Мухарлямов Н. Кардиомиопатии. Москва, 1990.
96. Aletras AH, Tilak GS, Hsu LY, Arai AE. Heterogeneity of intramural function in hypertrophic cardiomyopathy mechanistic insights from MRI late gadolinium enhancement and highresolution displacement encoding with stimulated echoes strain maps. Circ Cardiovasc Imaging. 2011;4(4):425-34. doi:10.1161/CIRCIMAGING.110.958751.
97. Camici PG, Olivotto I, Rimoldi OE. The coronary circulation and blood flow in left ventricular hypertrophy. J Mol Cell Cardiol. 2012;52(4):857-64. doi:10.1016/j.yjmcc.2011.08.028.
98. Einarsen E, Cramariuc D, Lønnebakken MT, et al. Comparison of Frequency of Ischemic Cardiovascular Events in Patients With Aortic Stenosis With Versus Without Asymmetric Septal Hypertrophy (from the SEAS Trial). Am J Cardiol. 2017;119(7):1082-7. doi:10.1016/j.amjcard.2016.11.064.
99. Foà A, Agostini V, Rapezzi C, et al. Histopathological comparison of intramural coronary artery remodeling and myocardial fibrosis in obstructive versus end-stage hypertrophic cardiomyopathy. Int J Cardiol. 2019;291:77-82. doi:10.1016/j.ijcard.2019.03.060.
100. Kwon DH, Smedira NG, Rodriguez ER, et al. Cardiac Magnetic Resonance Detection of Myocardial Scarring in Hypertrophic Cardiomyopathy. Correlation With Histopathology and Prevalence of Ventricular Tachycardia. J Am Coll Cardiol. 2009;54(3):242-9. doi:10.1016/j.jacc.2009.04.026.
101. Maron MS, Olivotto I, Maron BJ, et al. The Case for Myocardial Ischemia in Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2009;54(9):866-75. doi:10.1016/j.jacc.2009.04.072.
102. Mundhenke M, Schwartzkopff B, Strauer BE. Structural analysis of arteriolar and myocardial remodelling in the subendocardial region of patients with hypertensive heart disease and hypertrophic cardiomyopathy. Virchows Arch. 1997;431(4):265-73. doi:10.1007/s004280050098.
103. Nakamura T, Sakamoto K, Yamano T, et al. Increased plasma brain natriuretic peptide level as a guide for silent myocardial ischemia in patients with non-obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;39(10):1657-63. doi:10.1016/S07351097(02)01813-2.
104. Raphael CE, Cooper R, Parker KH, et al. Mechanisms of Myocardial Ischemia in Hypertrophic Cardiomyopathy: Insights From Wave Intensity Analysis and Magnetic Resonance. J Am Coll Cardiol. 2016;68(15):1651-60. doi:10.1016/j.jacc.2016.07.751.
105. Sciagrà R, Calabretta R, Cipollini F, et al. Myocardial blood flow and left ventricular functional reserve in hypertrophic cardiomyopathy: a 13NH3 gated PET study. Eur J Nucl Med Mol Imaging. 2017;44(5):866-75. doi:10.1007/s00259-016-3603-2.
106. Shin YJ, Lee JH, Yoo JY, et al. Clinical significance of evaluating coronary atherosclerosis in adult patients with hypertrophic cardiomyopathy who have chest pain. Eur Radiol. 2019;29(9):4593-602. doi:10.1007/s00330-018-5951-8.
107. Liu W, Sun D, Yang J. Diastolic Dysfunction of Hypertrophic Cardiomyopathy GenotypePositive Subjects Without Hypertrophy Is Detected by Tissue Doppler Imaging: A Systematic Review and Meta-analysis: A. J Ultrasound Med. 2017;36(10):2093-103. doi:10.1002/jum.14250.
108. Covella M, Rowin EJ, Hill NS, et al. Mechanism of Progressive Heart Failure and Significance of Pulmonary Hypertension in Obstructive Hypertrophic Cardiomyopathy. Circ Hear Fail. 2017;10(4): e003689. doi:10.1161/CIRCHEARTFAILURE.116.003689.
109. Germans T, Rüssel IK, Götte MJ, et al. How do hypertrophic cardiomyopathy mutations affect myocardial function in carriers with normal wall thickness? Assessment with cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2010;12(1):13. doi:10.1186/1532-429X-12-13.
110. Huang X, Yue Y, Wang Y, et al. Assessment of left ventricular systolic and diastolic abnormalities in patients with hypertrophic cardiomyopathy using real-time threedimensional echocardiography and two-dimensional speckle tracking imaging. Cardiovasc Ultrasound. 2018;16(1):23. doi:10.1186/s12947-018-0142-y.
111. Бокерия Л. А., Борисов К. В., Синев А. Ф. Улучшение диастолической функции левого и правого желудочков сердца после хирургической коррекции гипертрофической обструктивной кардиомиопатии при помощи оригинального способа. Грудная и сердечно-сосудистая хирургия. 1999;4:4-10.
112. Bravo PE, Luo HC, Pozios I, et al. Late gadolinium enhancement confined to the right ventricular insertion points in hypertrophic cardiomyopathy: An intermediate stage phenotype? Eur Heart J Cardiovasc Imaging. 2016;17(3):293-300. doi:10.1093/ehjci/jev154.
113. Fernández A, Vigliano CA, Casabé JH, et al. Comparison of prevalence, clinical course, and pathological findings of left ventricular systolic impairment versus normal systolic function in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2011;108(4):548-55. doi:10.1016/j.amjcard.2011.03.083.
114. Hiemstra YL, Debonnaire P, van Zwet EW, et al. Development of and Progression of Overt Heart Failure in Nonobstructive Hypertrophic Cardiomyopathy. Am J Cardiol. 2018;122(4):656-62. doi:10.1016/j.amjcard.2018.04.038.
115. Horimoto M, Yokota K, Inoue H, et al. Development of obstructive hypertrophic cardiomyopathy from nonobstructive hypertrophic cardiomyopathy. Am J Cardiol. 1998;82(3):403-5. doi:10.1016/S0002-9149(98)00337-3.
116. Melacini P, Basso C, Angelini A, et al. Clinicopathological profiles of progressive heart failure in hypertrophic cardiomyopathy. Eur Heart J. 2010;31(17):2111-23. doi:10.1093/eurheartj/ehq136.
117. Maron MS, Hauser TH, Dubrow E, et al. Right Ventricular Involvement in Hypertrophic Cardiomyopathy. Am J Cardiol. 2007;100(8):1293-8. doi:10.1016/j.amjcard.2007.05.061.
118. Li M, Zhang L, Zhang Z, et al. Isolated Severe Right Ventricular Hypertrophic Cardiomyopathy. Ann Thorac Surg. 2019;107(1): e23-5. doi:10.1016/J.ATHORACSUR.2018.05.061.
119. Falcone DM, Moore D, Lambert EC. Idiopathic hypertrophic cardiomyopathy involving the right ventricle. Am J Cardiol. 1967;19(5):735-40. doi:10.1016/0002-9149(67)90480-8.
120. Shimizu M, Kawai H, Yokota Y, Yokoyama M. Echocardiographic assessment of right ventricular obstruction in hypertrophic cardiomyopathy. Circ J. 2003;67(10):855-60. doi:10.1253/circj.67.855.
121. Бокерия Л. А., Борисов К. В., Синев А. и др. Результаты медикаментозного и хирургического лечения гипертрофической кардиомиопатии с обструкцией выводных отделов левого и правого желудочков сердца. Грудная и сердечно-сосудистая хирургия. 2004;(2):4-9.
122. Pagourelias ED, Efthimiadis GK, Parcharidou DG, et al. Prognostic Value of Right Ventricular Diastolic Function Indices in Hypertrophic Cardiomyopathy. Eur J Echocardiogr. 2011;12(11):809-17. doi:10.1093/EJECHOCARD/JER126.
123. Shah JP, Yang Y, Chen S, et al. Prevalence and Prognostic Significance of Right Ventricular Dysfunction in Patients With Hypertrophic Cardiomyopathy. Am J Cardiol. 2018;122(11):1932-8. doi:10.1016/j.amjcard.2018.08.043.
124. Sheppard MN, Westaby J, Zullo E, et al. Sudden arrhythmic death and cardiomyopathy are important causes of sudden cardiac death in the UK: results from a national coronial autopsy database. Histopathology. 2023;82(7):1056-66. doi:10.1111/HIS.14889.
125. Кактурский Л. Внезапная смерть (клиническая морфология). Москва, 2000.
126. Ревишвили А. Ш., Шляхто Е. В., Попов С. В. и др. Клинические рекомендации по проведению электрофизиологических исследований, катетерной абляции и применению имплантируемых антиаритмических устройств. Москва, 2017. 701 с. ISBN: 978-5-9500922-0-6.
127. Adabag AS, Casey SA, Kuskowski MA, et al. Spectrum and prognostic significance of arrhythmias on ambulatory Holter electrocardiogram in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2005;45(5):697-704. doi:10.1016/j.jacc.2004.11.043.
128. Czosek RJ, Jefferies JL, Khoury PR, et al. Arrhythmic Burden and Ambulatory Monitoring of Pediatric Patients with Cardiomyopathy. Pacing Clin Electrophysiol. 2016;39(5):443-51. doi:10.1111/pace.12835.
129. Desai MY, Mentias A. Risk stratification in hypertrophic cardiomyopathy. Aging (Albany NY). 2019;11(6):1617-8. doi:10.18632/aging.101895.
130. Elliott PM, Poloniecki J, Dickie S, et al. Sudden death in hypertrophic cardiomyopathy: Identification of high risk patients. J Am Coll Cardiol. 2000;36(7):2212-8. doi:10.1016/S0735-1097(00)01003-2.
131. Goyal V, Jassal DS, Dhalla NS. Pathophysiology and prevention of sudden cardiac death. Can J Physiol Pharmacol. 2015;94(3):237-44. doi:10.1139/cjpp-2015-0366.
132. Marrakchi S, Kammoun I, Bennour E, et al. Risk stratification in hypertrophic cardiomyopathy. Herz. 2020;45(1):50-64. doi:10.1007/s00059-018-4700-8.
133. Weissler-Snir A, Adler A, Williams L, et al. Prevention of Sudden Death in Hypertrophic Cardiomyopathy: Bridging the Gaps in Knowledge. Eur Hear J. 2017;38(22):1728-37.
134. Weissler-Snir A, Chan RH, Adler A, et al. Usefulness of 14-Day Holter for Detection of Nonsustained Ventricular Tachycardia in Patients With Hypertrophic Cardiomyopathy. Am J Cardiol. 2016;118(8):1258-63. doi:10.1016/j.amjcard.2016.07.043.
135. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Europace. 2006;8(9):746-837. doi:10.1093/europace/eul108.
136. Goff ZD, Calkins H. Sudden death related cardiomyopathies — Hypertrophic cardiomyopathy. Prog Cardiovasc Dis. 2019;62(3):212-6. doi:10.1016/j.pcad. 2019.04.001.
137. Zeppenfeld K, Tfelt-Hansen J, De Riva M, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022;43(40):3997-4126. doi:10.1093/EURHEARTJ/EHAC262.
138. Bois JP, Adams JC, Kumar G, et al. Relation between temperature extremes and symptom exacerbation in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2016;117(6):961-5. doi:10.1016/j.amjcard.2015.12.046.
139. Haghjoo M, Faghfurian B, Taherpour M, et al. Predictors of syncope in patients with hypertrophic cardiomyopathy. PACE — Pacing Clin Electrophysiol. 2009;32(5):642-7. doi:10.1111/j.1540-8159.2009.02338.x.
140. Seggewiß H, Koljaja-Batzner A, Seggewiß K, Meesmann M. Syncope in hypertrophic (obstructive) cardiomyopathy. Herzschrittmachertherapie Und Elektrophysiologie. 2018;29(2):178-82. doi:10.1007/s00399-018-0567-x.
141. Williams L, Frenneaux M. Syncope in Hypertrophic Cardiomyopathy: Mechanisms and Consequences for Treatment. Europace. 2007;9(9):817-22.
142. Farhad H, Seidelmann SB, Vigneault D, et al. Left Atrial structure and function in hypertrophic cardiomyopathy sarcomere mutation carriers with and without left ventricular hypertrophy. J Cardiovasc Magn Reson. 2017;19(1):107. doi:10.1186/s12968-0170420-0.
143. Burstein B, Nattel S. Atrial Fibrosis: Mechanisms and Clinical Relevance in Atrial Fibrillation. J Am Coll Cardiol. 2008;51(8):802-9. doi:10.1016/j.jacc.2007.09.064.
144. Philipson DJ, Rader F, Siegel RJ. Risk factors for atrial fibrillation in hypertrophic cardiomyopathy. Eur J Prev Cardiol. 2019: doi:10.1177/2047487319828474.
145. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the Management of Atrial Fibrillation Developed in Collaboration With EACTS. Eur Heart J. 2016;37:2893-962.
146. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the Europea. Eur Heart J. 2021;42(5):373-498. doi:10.1093/EURHEARTJ/EHAA612.
147. Maron BJ, Rowin EJ, Udelson JE, Maron MS. Clinical Spectrum and Management of Heart Failure in Hypertrophic Cardiomyopathy. JACC Hear Fail. 2018;6(5):353-63. doi:10.1016/j.jchf.2017.09.011.
148. Seferović PM, Polovina M, Bauersachs J, et al. Heart failure in cardiomyopathies: a position paper from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21(5):553-76. doi:10.1002/ejhf.1461.
149. Garg L, Gupta M, Sabzwari SRA, et al. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical impact, and management. Heart Fail Rev. 2019;24(2):189-97. doi:10.1007/s10741-018-9752-6.
150. Arakelyan MG, Bockeria LA, Vasilieva EY, et al. 2020 Clinical guidelines for Atrial fibrillation and atrial flutter. Russian Journal of Cardiology. 2021;26(7):4594. (In Russ.) Аракелян М. Г., Бокерия Л. А., Васильева Е. Ю. и др. Фибрилляция и трепетание предсердий. Клинические рекомендации 2020. Российский кардиологический журнал. 2021;26(7):4594. doi:10.15829/1560-4071-2021-4594.
151. Donnellan E, Wazni OM, Hanna M, et al. Atrial Fibrillation in Transthyretin Cardiac Amyloidosis: Predictors, Prevalence, and Efficacy of Rhythm Control Strategies. JACC Clin Electrophysiol. 2020;6(9):1118-27. doi:10.1016/J.JACEP.2020.04.019.
152. Marstrand P, Han L, Day SM, et al. Hypertrophic Cardiomyopathy With Left Ventricular Systolic Dysfunction: Insights From the SHaRe Registry. Circulation. 2020;141(17):137183. doi:10.1161/CIRCULATIONAHA.119.044366.
153. Russian Society of Cardiology (RSC) 2020 Clinical practice guidelines for Chronic heart failure. Russian Journal of Cardiology. 2020;25(11):4083. (In Russ.) Российское кардиологическое общество (РКО) Хроническая сердечная недостаточность. Клинические рекомендации 2020. Российский кардиологический журнал. 2020;25(11):4083. doi:10.15829/1560-4071-2020-4083.
154. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599-726. doi:10.1093/EURHEARTJ/EHAB368.
155. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17): e263-421. doi:10.1016/j.jacc.2021.12.012.
156. Pálinkás ED, Re F, Peteiro J, et al. Pulmonary congestion during Exercise stress Echocardiography in Hypertrophic Cardiomyopathy. Int J Cardiovasc Imaging. 2022;38(12):2593-604. doi:10.1007/S10554-022-02620-0.
157. Maron MS, Finley JJ, Bos JM, et al. Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy. Circulation. 2008;118(15):1541-9. doi:10.1161/CIRCULATIONAHA.108.781401.
158. Towe EC, Bos JM, Ommen SR, et al. Genotype-Phenotype Correlations in Apical Variant Hypertrophic Cardiomyopathy. Congenit Heart Dis. 2015;10(3): E139-45. doi:10.1111/CHD.12242.
159. Rowin EJ, Maron BJ, Haas TS, et al. Hypertrophic Cardiomyopathy With Left Ventricular Apical Aneurysm: Implications for Risk Stratification and Management. J Am Coll Cardiol. 2017;69(7):761-73. doi:10.1016/J.JACC.2016.11.063.
160. Yang K, Song YY, Chen XY, et al. Apical hypertrophic cardiomyopathy with left ventricular apical aneurysm: prevalence, cardiac magnetic resonance characteristics, and prognosis. Eur Hear Journal Cardiovasc Imaging. 2020;21(12):1341-50. doi:10.1093/EHJCI/JEAA246.
161. Calabretta R, Kokomani A, Fumagalli C, et al. Evaluation of stress myocardial blood flow patterns in patients with apical hypertrophic cardiomyopathy. J Nucl Cardiol. 2022;29(4):1946-51. doi:10.1007/S12350-022-02911-Y.
162. Cui L, Suo Y, Zhao Y, et al. Mid-Ventricular Obstructive Hypertrophic Cardiomyopathy and Apical Aneurysm Mimicking Acute ST-Elevation Myocardial Infarction. Ann Noninvasive Electrocardiol. 2016;21(1):98-101. doi:10.1111/ANEC.12284.
163. Mörner S, Johansson B, Henein M. Arrhythmogenic left ventricular apical aneurysm in hypertrophic cardiomyopathy. Int J Cardiol. 2011;151(1): e8. doi:10.1016/J.IJCARD.2010. 02.071.
164. Dilaveris P, Aggeli C, Synetos A, et al. Sustained ventricular tachycardia as a first manifestation of hypertrophic cardiomyopathy with mid-ventricular obstruction and apical aneurysm in an elderly female patient. Ann Noninvasive Electrocardiol. 2017;22(3): e12422. doi:10.1111/ANEC.12422.
165. Pérez-Riera AR, Barbosa-Barros R, de Lucca AA, et al. Mid-ventricular Hypertrophic Obstructive Cardiomyopathy with Apical Aneurysm Complicated with Syncope by Sustained Monomorphic Ventricular Tachycardia. Ann Noninvasive Electrocardiol. 2016;21(6):618-21. doi:10.1111/ANEC.12377.
166. Papanastasiou CA, Zegkos T, Karamitsos TD, et al. Prognostic role of left ventricular apical aneurysm in hypertrophic cardiomyopathy: A systematic review and meta-analysis. Int J Cardiol. 2021;332:127-32. doi:10.1016/J.IJCARD.2021.03.056.
167. Chang HC, Kuo L, Sung SH, et al. Left Ventricular Apical Aneurysm in Fabry Disease: Implications for Clinical Significance and Risk Stratification. J Am Heart Assoc. 2023;12(1): e027041. doi:10.1161/JAHA.122.027041.
168. Terai H, Shimizu M, Ino H, et al. Changes in cardiac sympathetic nerve innervation and activity in pathophysiologic transition from typical to end-stage hypertrophic cardiomyopathy. J Nucl Med. 2003;44(10):1612-7.
169. Ciampi Q, Olivotto I, Peteiro J, et al. Prognostic Value of Reduced Heart Rate Reserve during Exercise in Hypertrophic Cardiomyopathy. J Clin Med. 2021;10(7):1347. doi:10.3390/JCM10071347.
170. Maron BA, Kleiner DE, Arons E, et al. Evidence of Advanced Pulmonary Vascular Remodeling in Obstructive Hypertrophic Cardiomyopathy With Pulmonary Hypertension. Chest. 2023;163(3):678-86. doi:10.1016/J.CHEST.2022.09.040.
171. Re F, Halasz G, Moroni F, et al. Exercise-induced pulmonary hypertension in hypertrophic cardiomyopathy: a combined cardiopulmonary exercise test-echocardiographic study. Int J Cardiovasc Imaging. 2022;38(11):2345-52. doi:10.1007/S10554-022-02671-3.
172. Geske JB, Konecny T, Ommen SR, et al. Surgical myectomy improves pulmonary hypertension in obstructive hypertrophic cardiomyopathy. Eur Heart J. 2014;35(30):2032-9. doi:10.1093/EURHEARTJ/EHT537.
173. Maron BJ, Olivotto I, Spirito P, et al. Epidemiology of Hypertrophic CardiomyopathyRelated Death. Circulation. 2000;102(8):858-64. doi:10.1161/01.CIR.102.8.858.
174. Semsarian C, Ingles J, Maron MS, Maron BJ. New perspectives on the prevalence of hypertrophic cardiomyopathy. J Am Coll Cardiol. 2015;65(12):1249-54. doi:10.1016/j.jacc.2015.01.019.
175. Maurer MS, Hanna M, Grogan M, et al. Genotype and Phenotype of Transthyretin Cardiac Amyloidosis: THAOS (Transthyretin Amyloid Outcome Survey). J Am Coll Cardiol. 2016;68(2):161-72. doi:10.1016/J.JACC.2016.03.596.
176. Rigopoulos AG, Ali M, Abate E, et al. Advances in the diagnosis and treatment of transthyretin amyloidosis with cardiac involvement. Heart Fail Rev. 2019;24(4):521-33. doi:10.1007/S10741-019-09776-3.
177. Amano Y, Kitamura M, Takayama M, et al. MRI classification of asymmetric septal hypertrophic cardiomyopathy and its relation to the presence of risk factors. Int J Cardiovasc Imaging. 2012;28(8):2019-25. doi:10.1007/s10554-012-0034-4.
178. Geske JB, Ommen SR, Gersh BJ. Hypertrophic Cardiomyopathy: Clinical Update. JACC Hear Fail. 2018;6(5):364-75. doi:10.1016/j.jchf.2018.02.010.
179. Neubauer S, Kolm P, Ho CY, et al. Distinct Subgroups in Hypertrophic Cardiomyopathy in the NHLBI HCM Registry. J Am Coll Cardiol. 2019;74(19):2333-45. doi:10.1016/J.JACC.2019.08.1057.
180. Игнатенко Г. А., Тарадин Г. Г., Куглер Т. Е. Особенности гипертрофии левого желудочка и характеристика фенотипических вариантов у больных гипертрофической кардиомиопатией. Архивъ внутренней медицины. 2023;13(4):282-93. doi:10.20514/2226-6704-2023-13-4-282-293.
181. Rapezzi C, Arbustini E, Caforio ALP, et al. Diagnostic work-up in cardiomyopathies: bridging the gap between clinical phenotypes and final diagnosis. A position statement from the ESC Working Group on Myocardial and Pericardial Diseases. Eur Hear J. 2013;34:1448-58.
182. Gudkova A, Kostareva A, Sjoberg G, et al. Diagnostic challenge in desmin cardiomyopathy with transformation of clinical phenotypes. Pediatr Cardiol. 2013;34(2):467-70. doi:10.1007/s00246-012-0312-x.
183. Olivotto I, Cecchi F, Poggesi C, Yacoub MH. Patterns of disease progression in hypertrophic cardiomyopathy an individualized approach to clinical staging. Circ Hear Fail. 2012;5(4):535-46. doi:10.1161/CIRCHEARTFAILURE.112.967026.
184. Argirò A, Zampieri M, Marchi A, et al. Stage-specific therapy for hypertrophic cardiomyopathy. Eur Heart J Suppl. 2023;25(Suppl C): C155-61. doi:10.1093/EURHEARTJSUPP/SUAD042.
185. Rowin EJ, Maron MS, Chan RH, et al. Interaction of Adverse Disease Related Pathways in Hypertrophic Cardiomyopathy. Am J Cardiol. 2017;120(12):2256-64. doi:10.1016/j.amjcard.2017.08.048.
186. Габрусенко С. А., Сафрыгина Ю. В., Овчинников А. Г. и др. Клинико-гемодинамический статус и сердечные натрийуретические пептиды в плазме больных гипертрофической кардиомиопатией. Кардиологический вестник (Бюллетень РКНПК). 2006;1(2):25-31.
187. Дземешкевич С. Л., Фролова Ю. В., Ким С. Ю. и др. Анатомические и морфологические признаки диффузно-генерализованной формы гипертрофической кардиомиопатии. Российский кардиологический журнал. 2015;(5):58-63. doi:10.15829/1560-4071-2015-5-58-63.
188. Стрельцова А. А., Гудкова А. Я., Костарева А. А. Фибрилляция предсердий при гипертрофической кардиомиопатии: современные аспекты эпидемиологии, факторов риска, патогенеза и фармакотерапии. Cons Medicum. 2018;20(5):34-9.
189. Стрельцова А. А., Гудкова А. Я., Полякова А. А. и др. Полиморфный вариант rs1739843 гена белка теплового шока 7 (HSPB7) и его связь с вариантами клинического течения и исходами у пациентов с гипертрофической кардиомиопатией (результаты 10-летнего наблюдения). Российский кардиологический журнал. 2019;(10):7-15. doi:10.15829/1560-4071-2019-10-7-15.
190. Harris KM, Spirito P, Maron MS, et al. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation. 2006;114(3):216-25. doi:10.1161/CIRCULATIONAHA.105.583500.
191. Bos JM, Ommen SR, Ackerman MJ. Genetics of hypertrophic cardiomyopathy: one, two, or more diseases? Curr Opin Cardiol. 2007;22(3):193-9. doi:10.1097/HCO.0b013e3280e1cc7f.
192. Lancellotti P, Pellikka PA, Budts W, et al. The Clinical Use of Stress Echocardiography in Non-Ischaemic Heart Disease: Recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30(2):101-38. doi:10.1016/j.echo.2016.10.016.
193. Parato VM, Antoncecchi V, Sozzi F, et al. Echocardiographic diagnosis of the different phenotypes of hypertrophic cardiomyopathy. Cardiovasc Ultrasound. 2016;14(1):30. doi:10.1186/s12947-016-0072-5.
194. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution. Eur J Heart Fail. 2016;18(8):891-975. doi:10.1002/ejhf.592.
195. Maron BJ, McKenna WJ, Danielson GK, et al. American College of Cardiology/ European Society of Cardiology Clinical Expert Consensus Document on Hypertrophic Cardiomyopathy: A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European S. Eur Heart J. 2003;24(21):1965-91. doi:10.1016/S0195-668X(03)00479-2.
196. Merlo M, Pagura L, Porcari A, et al. Unmasking the prevalence of amyloid cardiomyopathy in the real world: results from Phase 2 of the AC-TIVE study, an Italian nationwide survey. Eur J Heart Fail. 2022;24(8):1377-86. doi:10.1002/EJHF.2504.
197. Cantwell JD. Preparticipation physical evaluation: Getting to the heart of the matter. Med Sci Sports Exerc. 1998;30(10):341-4. doi:10.1097/00005768-199810001-00001.
198. Efthimiadis GK, Parcharidou D, Pagourelias ED, et al. Prevalence and Clinical Outcomes of Incidentally Diagnosed Hypertrophic Cardiomyopathy. Am J Cardiol. 2010;105(10):144550. doi:10.1016/j.amjcard.2009.12.066.
199. Harmon KG, Zigman M, Drezner JA. The effectiveness of screening history, physical exam, and ECG to detect potentially lethal cardiac disorders in athletes: A systematic review/ meta-analysis. J Electrocardiol. 2015;48(3):329-38. doi:10.1016/j.jelectrocard.2015.02.001.
200. Raviele A, Giada F, Bergfeldt L, et al. Management of Patients With Palpitations: A Position Paper From the European Heart Rhythm Association. Europace. 2011;13(7):920-34.
201. Attenhofer Jost CH, Turina J, Mayer K, et al. Echocardiography in the evaluation of systolic murmurs of unknown cause. Am J Med. 2000;108(8):614-20. doi:10.1016/S00029343(00)00361-2.
202. Barrett MJ, Ayub B, Martinez MW. Cardiac auscultation in sports medicine: Strategies to improve clinical care. Curr Sports Med Rep. 2012;11(2):78-84. doi:10.1249/JSR.0b013e318249c0ff.
203. Nagueh SF, Phelan D, Abraham T, et al. Recommendations for Multimodality Cardiovascular Imaging of Patients with Hypertrophic Cardiomyopathy: An Update from the American Society of Echocardiography, in Collaboration with the American Society of Nuclear Cardiology, the Society for Cardiovascula. J Am Soc Echocardiogr. 2022;35(6):533-69. doi:10.1016/J.ECHO.2022.03.012.
204. Barcia G, Rachid M, Magen M, et al. Pitfalls in molecular diagnosis of Friedreich ataxia. Eur J Med Genet. 2018;61(8):455-8. doi:10.1016/j.ejmg.2018.03.004.
205. Monserrat L, Gimeno-Blanes JR, Marín F, et al. Prevalence of Fabry Disease in a Cohort of 508 Unrelated Patients With Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2007;50(25):2399-403. doi:10.1016/j.jacc.2007.06.062.
206. Rapezzi C, Quarta CC, Obici L, et al. Disease profile and differential diagnosis of hereditary transthyretin-related amyloidosis with exclusively cardiac phenotype: an Italian perspective. Eur Hear J. 2013;34(7):520-8.
207. Sarkozy A, Digilio MC, Dallapiccola B. Leopard syndrome. Orphanet J Rare Dis. 2008;3(1): Article number: 13. doi:10.1186/1750-1172-3-13.
208. Scaglia F, Towbin JA, Craigen WJ, et al. Clinical Spectrum, Morbidity, and Mortality in 113 Pediatric Patients with Mitochondrial Disease. Pediatrics. 2004;114(4):925-31. doi:10.1542/peds.2004-0718.
209. Yang Z, Vatta M. Danon disease as a cause of autophagic vacuolar myopathy. Congenit Heart Dis. 2007;2(6):404-9. doi:10.1111/j.1747-0803.2007.00132.x.
210. Yang Z, McMahon CJ, Smith LR, et al. Danon Disease as an Underrecognized Cause of Hypertrophic Cardiomyopathy in Children. Circulation. 2005;112(11):1612-7. doi:10.1161/CIRCULATIONAHA.105.546481.
211. Pagourelias ED, Efthimiadis GK, Kouidi E, et al. Efficacy of various "classic" echocardiographic and laboratory indices in distinguishing the "gray zone" between athlete’s heart and hypertrophic cardiomyopathy: A pilot study. Echocardiography. 2013;30(2):131-9. doi:10.1111/echo.12014.
212. Grogan M, Scott CG, Kyle RA, et al. Natural History of Wild-Type Transthyretin Cardiac Amyloidosis and Risk Stratification Using a Novel Staging System. J Am Coll Cardiol. 2016;68(10):1014-20. doi:10.1016/J.JACC.2016.06.033.
213. Vergaro G, Castiglione V, Aimo A, et al. N-terminal pro-B-type natriuretic peptide and high-sensitivity troponin T hold diagnostic value in cardiac amyloidosis. Eur J Heart Fail. 2023;25(3):1014-20. doi:10.1002/EJHF.2769.
214. Witteles RM, Bokhari S, Damy T, et al. Screening for Transthyretin Amyloid Cardiomyopathy in Everyday Practice. JACC Heart Fail. 2019;7(8):709-16. doi:10.1016/J. JCHF.2019.04.010.
215. Damy T, Costes B, Hagège AA, et al. Prevalence and clinical phenotype of hereditary transthyretin amyloid cardiomyopathy in patients with increased left ventricular wall thickness. Eur Heart J. 2016;37(23):1826-34. doi:10.1093/EURHEARTJ/EHV583.
216. Maurizi N, Rella V, Fumagalli C, et al. Prevalence of cardiac amyloidosis among adult patients referred to tertiary centres with an initial diagnosis of hypertrophic cardiomyopathy. Int J Cardiol. 2020;300:191-5. doi:10.1016/J.IJCARD.2019.07.051.
217. Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405-24. doi:10.1038/gim.2015.30.
218. Ackerman MJ, Priori SG, Willems S, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Hear Rhythm. 2011;8(8):1308-39. doi:10.1016/J.HRTHM.2011.05.020.
219. Hershberger RE, Givertz MM, Ho CY, et al. Genetic Evaluation of Cardiomyopathy — A Heart Failure Society of America Practice Guideline. J Card Fail. 2018;24(5):281-302. doi:10.1016/j.cardfail.2018.03.004.
220. Wilde AAM, Semsarian C, Márquez MF, et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) Expert Consensus Statement on the state of genetic testing for cardiac diseases. Europace. 2022;24(8):1307-67. doi:10.1002/joa3.12717.
221. Gabrusenko SA, Seleznev DM, Naumov VG. Genetic aspects of hypertrophic cardiomyopathy (literature review). A practicing doctor. 2000;18(2):2-5. (In Russ.) Габрусенко С. А., Селезнёв Д. М., Наумов В. Г. Генетические аспекты гипертрофической кардиомиопатии (обзор литературы). Практикующий врач. 2000;18(2):2-5.
222. Селезнев Д. М., Габрусенко С. А., Парфенова Е. В. и др. Роль мутаций в гене тяжелой цепи сердечного бета-миозина в российской популяции больных с гипертрофической кардиомиопатией. Кардиология. 2005;45(4):15-20.
223. E, et al. Accuracy of European diagnostic criteria for familial hypertrophic cardiomyopathy in a genotyped population. Int J Cardiol. 2003 90(1):33-8. doi:10.1016/S0167-5273(02)00534-X.
224. Дроздов Д. В., Макаров Л. М., Баркан В. С. и др. Регистрация электрокардиограммы покоя в 12 общепринятых отведениях взрослым и детям 2023. Методические рекомендации. Российский кардиологический журнал. 2023;28(10):5631. doi:10.15829/1560-4071-2023-5631. EDN: JAVUJL.
225. Jalanko M, Heliö T, Mustonen P, et al. Novel electrocardiographic features in carriers of hypertrophic cardiomyopathy causing sarcomeric mutations. J Electrocardiol. 2018;51(6):983-9. doi:10.1016/J.JELECTROCARD.2018.07.009.
226. Lakdawala NK, Thune JJ, Maron BJ, et al. Electrocardiographic features of sarcomere mutation carriers with and without clinically overt hypertrophic cardiomyopathy. Am J Cardiol. 2011;108(11):1606-13. doi:10.1016/J.AMJCARD.2011.07.019.
227. Finocchiaro G, Sheikh N, Biagini E, et al. The electrocardiogram in the diagnosis and management of patients with hypertrophic cardiomyopathy. Hear Rhythm. 2020;17(1):142-51. doi:10.1016/J.HRTHM.2019.07.019.
228. Bernardini A, Crotti L, Olivotto I, Cecchi F. Diagnostic and prognostic electrocardiographic features in patients with hypertrophic cardiomyopathy. Eur Heart J Suppl. 2023;25(Suppl C): C173-8. doi:10.1093/EURHEARTJSUPP/SUAD074.
229. McLeod CJ, Ackerman MJ, Nishimura RA, et al. Outcome of Patients With Hypertrophic Cardiomyopathy and a Normal Electrocardiogram. J Am Coll Cardiol. 2009;54(3):229-33. doi:10.1016/j.jacc.2009.02.071.
230. Arima N, Ochi Y, Takahashi M, et al. Transient decrease in the depth of the negative T wave in apical hypertrophic cardiomyopathy is a sign of left anterior descending artery stenosis: a case series. Eur Hear Journal Case Reports. 2023;7(1): ytad034. doi:10.1093/EHJCR/YTAD034.
231. Delcrè SDL, Di Donna P, Leuzzi S, et al. Relationship of ECG findings to phenotypic expression in patients with hypertrophic cardiomyopathy: a cardiac magnetic resonance study. Int J Cardiol. 2013;167(3):1038-45. doi:10.1016/J.IJCARD.2012.03.074.
232. Biagini E, Pazzi C, Olivotto I, et al. Usefulness of Electrocardiographic Patterns at Presentation to Predict Long-term Risk of Cardiac Death in Patients With Hypertrophic Cardiomyopathy. Am J Cardiol. 2016;118(3):432-9. doi:10.1016/J.AMJCARD.2016.05.023.
233. Bi X, Yang C, Song Y, et al. Quantitative fragmented QRS has a good diagnostic value on myocardial fibrosis in hypertrophic obstructive cardiomyopathy based on clinical-pathological study. BMC Cardiovasc Disord. 2020;20(1):298. doi:10.1186/S12872-020-01590-2.
234. Kang KW, Janardhan AH, Jung KT, et al. Fragmented QRS as a candidate marker for highrisk assessment in hypertrophic cardiomyopathy. Hear Rhythm. 2014;11(8):1433-40. doi:10.1016/J.HRTHM.2014.05.002.
235. Fananapazir L, Tracy CM, Leon MB, et al. Electrophysiologic abnormalities in patients with hypertrophic cardiomyopathy. A consecutive analysis in 155 patients. Circulation. 1989;80(5):1259-68. doi:10.1161/01.CIR.80.5.1259.
236. Kelly BS, Mattu A, Brady WJ. Hypertrophic cardiomyopathy: electrocardiographic manifestations and other important considerations for the emergency physician. Am J Emerg Med. 2007;25(1):72-9. doi:10.1016/j.ajem.2006.04.017.
237. Wilke I, Witzel K, Münch J, et al. High Incidence of De Novo and Subclinical Atrial Fibrillation in Patients With Hypertrophic Cardiomyopathy and Cardiac Rhythm Management Device. J Cardiovasc Electrophysiol. 2016;27(7):779-84. doi:10.1111/jce.12982.
238. Хирманов В. Н., Трешкур Т. В., Тюрина Т. В. и др. Электрокардиографические методы в диагностике, выборе метода и тактики лечения гипертрофической кардиомиопатии. Prog Biomed Res. 1997;2(1):7-22.
239. O’Mahony C, Jichi F, Pavlou M, et al. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM Risk-SCD). Eur Hear J. 2014;35(30): 2010-20. doi:10.1093/eurheartj/eht439.
240. Wasfy MM, Weiner RB. Differentiating the athlete’s heart from hypertrophic cardiomyopathy. Curr Opin Cardiol. 2015:500-5. doi:10.1097/HCO.0000000000000203.
241. Weigner MJ, Caulfield TA, Danias PG, et al. Risk for clinical thromboembolism associated with conversion to sinus rhythm in patients with atrial fibrillation lasting less than 48 hours. Ann Intern Med. 1997;126(8):615-20. doi:10.7326/0003-4819-126-8-199704150-00005.
242. Guttmann OP, Rahman MS, O’Mahony C, et al. Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: Systematic review. Heart. 2014;100(6):46572. doi:10.1136/heartjnl-2013-304276.
243. Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association. Europace. 2013;15(8):1070-118. doi:10.1093/europace/eut206.
244. Brignole M, Vardas P, Hoffman E, et al. Indications for the use of diagnostic implantable and external ECG loop recorders. Europace. 2009;11(5):671-87. doi:10.1093/europace/eup097.
245. Frangini PA, Cecchin F, Jordao L, et al. How revealing are insertable loop recorders in pediatrics? Pacing Clin Electrophysiol. 2008;31(3):338-43. doi:10.1111/j.15408159.2008.00995.x.
246. Solano A, Menozzi C, Maggi R, et al. Incidence, diagnostic yield and safety of the implantable loop-recorder to detect the mechanism of syncope in patients with and without structural heart disease. Eur Heart J. 2004;25(13):1116-9. doi:10.1016/j.ehj.2004.05.013.
247. Алехин М. Н., Бартош-Зеленая С. Ю., Берестень Н. Ф. Стандартизация проведения трансторакальной эхокардиографии у взрослых: консенсус экспертов Российской ассоциации специалистов ультразвуковой диагностики в медицине (РАСУДМ) и Российской ассоциации специалистов функциональной диагностики (РАСФД). Ультразвуковая и функциональная диагностика. 2021;2:63-79. doi:10.24835/1607-0771-2021-2-63-79. EDN MUCMFC.
248. Мареев Ю. В., Джиоева О. Н., Зоря О. Т. и др. Фокусное ультразвуковое исследование в практике врача-кардиолога. Российский согласительный документ. Кардиология. 2021;61(11):4-23. doi:10.18087/CARDIO.2021.11.N1812.
249. Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2018;32(1):1-64. doi:10.1016/j.echo.2018.06.004.
250. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233-71. doi:10.1093/ehjci/jev014.
251. Cerqueira M, Weissman N, Dilsizian V, et al. Standardized Myocardial Segmentation and Nomenclature for Tomographic Imaging of the Heart A Statement for Healthcare Professionals From the Cardiac Imaging Committee. Circulation. 2002;105(4):539-42. doi:10.1161/hc0402.102975.
252. Flachskampf F, Badano L, Daniel W, et al. Recommendations for Transoesophageal Echocardiography: Update 2010. Eur J Echocardiogr. 2010;11(7):557-76. doi:10.1093/EJECHOCARD/JEQ057.
253. Nagueh S, Smiseth O, Appleton C, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Hear J Cardiovasc Imaging. 2016;17(12):1321-60. doi:10.1093/ehjci/jew082.
254. Senior R, Becher H, Monaghan M, et al. Contrast echocardiography: evi.dence-based recommendations by European Association of Echocardiography. Eur J Echocardiogr. 2009;10(2):194-212.
255. Klues HG, Schiffers A, Maron BJ. Phenotypic spectrum and patterns of left ventricular hypertrophy in hypertrophic cardiomyopathy: Morphologic observations and significance as assessed by two-dimensional echocardiography in 600 patients. J Am Coll Cardiol. 1995;26(7):1699-708. doi:10.1016/0735-1097(95)00390-8.
256. Maron BJ, Casey SA, Hauser RG, Aeppli DM. Clinical course of hypertrophic cardiomyopathy with survival to advanced age. J Am Coll Cardiol. 2003;42(5):882-8. doi:10.1016/S0735-1097(03)00855-6.
257. Maron BJ, Rowin EJ, Maron MS, Braunwald E. Nonobstructive Hypertrophic Cardiomyopathy Out of the Shadows: Known from the Beginning but Largely Ignored … Until Now. Am J Med. 2017;130(2):119-23. doi:10.1016/j.amjmed.2016.09.015.
258. Maron MS, Olivotto I, Zenovich AG, et al. Hypertrophic cardiomyopathy is predominantly a disease of left ventricular outflow tract obstruction. Circulation. 2006;114(21):2232-9. doi:10.1161/CIRCULATIONAHA.106.644682.
259. Elliott P, Gimeno J, Tomé M, McKenna W. Left ventricular outflow tract obstruction and sudden death in hypertrophic cardiomyopathy. Eur Heart J. 2006;27(24):3073-4. doi:10.1093/eurheartj/ehl383.
260. Spirito P, Bellone P, Harris KM, et al. Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med. 2000;342(24):1778-85. doi:10.1056/NEJM200006153422403.
261. Belenkie I, MacDonald RPR, Smith ER. Localized septal hypertrophy: Part of the spectrum of hypertrophic cardiomyopathy or an incidental echocardiographic finding? Am Heart J. 1988;115(2):385-90. doi:10.1016/0002-8703(88)90486-3.
262. Gardin J, Palabrica T, Dubria S, et al. Localized basal ventricular septal hypertrophy — prevalence, functional and clinical correlates in a population referred for echocardiography. Am J Noninvas Card. 1998;6(1):5-8.
263. Losi MA, Nistri S, Galderisi M, et al. Echocardiography in patients with hypertrophic cardiomyopathy: Usefulness of old and new techniques in the diagnosis and pathophysiological assessment. Cardiovasc Ultrasound. 2010;8(1): Article number: 7. doi:10.1186/1476-7120-8-7.
264. Alvares RF, Goodwin JF. Non-invasive assessment of diastolic function in hypertrophic cardiomyopathy on and off beta adrenergic blocking drugs. Br Heart J. 1982;48(3):20412. doi:10.1136/hrt.48.3.204.
265. Biagini E, Spirito P, Rocchi G, et al. Prognostic Implications of the Doppler Restrictive Filling Pattern in Hypertrophic Cardiomyopathy. Am J Cardiol. 2009;104(12):1727-31. doi:10.1016/j.amjcard.2009.07.057.
266. Matsumura Y, Elliott PM, Virdee MS, et al. Left ventricular diastolic function assessed using Doppler tissue imaging in patients with hypertrophic cardiomyopathy: Relation to symptoms and exercise capacity. Heart. 2002;87(3):247-51. doi:10.1136/heart.87.3.247.
267. Kubo T, Gimeno JR, Bahl A, et al. Prevalence, Clinical Significance, and Genetic Basis of Hypertrophic Cardiomyopathy With Restrictive Phenotype. J Am Coll Cardiol. 2007;49(25):2419-26. doi:10.1016/j.jacc.2007.02.061.
268. Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10(2):165-93. doi:10.1093/EJECHOCARD/JEP007.
269. Dimitrow PP, Bober M, Michałowska J, Sorysz D. Left ventricular outflow tract gradient provoked by upright position or exercise in treated patients with hypertrophic cardiomyopathy without obstruction at rest. Echocardiography. 2009;26(5):513-20. doi:10.1111/j.1540-8175.2008.00851.x.
270. Nistri S, Olivotto I, Maron MS, et al. Timing and significance of exercise-induced left ventricular outflow tract pressure gradients in hypertrophic cardiomyopathy. Am J Cardiol. 2010;106(9):1301-6. doi:10.1016/j.amjcard.2010.06.057.
271. Olivotto I, Montereggi A, Mazzuoli F, Cecchi F. Clinical utility and safety of exercise testing in patients with hypertrophic cardiomyopathy. G Ital Cardiol. 1999;29:11-9.
272. Sadoul N, Prasad K, Elliott PM, et al. Prospective prognostic assessment of blood pressure response during exercise in patients with hypertrophic cardiomyopathy. Circulation. 1997;96(9):2987-91. doi:10.1161/01.CIR.96.9.2987.
273. Tower-Rader A, Betancor J, Lever HM, Desai MY. A Comprehensive Review of Stress Testing in Hypertrophic Cardiomyopathy: Assessment of Functional Capacity, Identification of Prognostic Indicators, and Detection of Coronary Artery Disease. J Am Soc Echocardiogr. 2017;30(9):829-44. doi:10.1016/j.echo.2017.05.017.
274. Cardim N, Galderisi M, Edvardsen T, et al. Role of multimodality cardiac imaging in the management of patients with hypertrophic cardiomyopathy: An expert consensus of the European Association of Cardiovascular Imaging Endorsed by the Saudi Heart Association. Eur Heart J Cardiovasc Imaging. 2015;16(3):280. doi:10.1093/ehjci/jeu291.
275. Kim MS, Klein AJ, Groves BM, et al. Left Ventricular Outflow Tract Obstruction in the Presence of Asymmetric Septal Hypertrophy and Accessory Mitral Valve Tissue Treated With Alcohol Septal Ablation. Eur J Echocardiogr. 2008;9(5):720-4. doi:10.1093/EJECHOCARD/JEN152.
276. Monakier D, Woo A, Puri T, et al. Usefulness of myocardial contrast echocardiographic quantification of risk area for predicting postprocedural complications in patients undergoing septal ethanol ablation for obstructive hypertrophic cardiomyopathy. Am J Cardiol. 2004;94(12):1515-22. doi:10.1016/j.amjcard.2004.08.030.
277. Wallace EL, Thompson JJ, Faulkner MW, et al. Septal perforator anatomy and variability of perfusion bed by myocardial contrast echocardiography: A study of hypertrophic cardiomyopathy patients undergoing alcohol septal ablation. J Interv Cardiol. 2013;26(6):604-12. doi:10.1111/joic.12068.
278. Spirito P, Autore C, Formisano F, et al. Risk of sudden death and outcome in patients with hypertrophic cardiomyopathy with benign presentation and without risk factors. Am J Cardiol. 2014;113(9):1550-5. doi:10.1016/j.amjcard.2014.01.435.
279. Grigg LE, Wigle ED, Williams WG, et al. Transesophageal Doppler echocardiography in obstructive hypertrophic cardiomyopathy: Clarification of pathophysiology and importance in intraoperative decision making. J Am Coll Cardiol. 1992;20(1):42-52. doi:10.1016/0735-1097(92)90135-A.
280. Oki T, Fukuda N, Iuchi A, et al. Transesophageal echocardiographic evaluation of mitral regurgitation in hypertrophic cardiomyopathy: Contributions of eccentric left ventricular hypertrophy and related abnormalities of the mitral complex. J Am Soc Echocardiogr. 1995;8(4)503-10. doi:10.1016/S0894-7317(05)80338-4.
281. Yu EHC, Omran AS, Wigle ED, et al. Mitral regurgitation in hypertrophic obstructive cardiomyopathy: Relationship to obstruction and relief with myectomy. J Am Coll Cardiol. 2000;36(7):2219-25. doi:10.1016/S0735-1097(00)01019-6.
282. Marwick TH, Stewart WJ, Lever HM, et al. Benefits of intraoperative echocardiography in the surgical management of hypertrophic cardiomyopathy. J Am Coll Cardiol. 1992;20(5):1066-72. doi:10.1016/0735-1097(92)90359-U.
283. Huurman R, Van Der Velde N, Schinkel AFL, et al. Contemporary family screening in hypertrophic cardiomyopathy: the role of cardiovascular magnetic resonance. Eur Hear Journal Cardiovasc Imaging. 2022;23(9):1144-54. doi:10.1093/EHJCI/JEAC099.
284. Bois JP, Geske JB, Foley TA, et al. Comparison of Maximal Wall Thickness in Hypertrophic Cardiomyopathy Differs Between Magnetic Resonance Imaging and Transthoracic Echocardiography. Am J Cardiol. 2017;119(4):643-50. doi:10.1016/J.AMJCARD.2016.11.010.
285. Гурщенков А. В., Моисеева О. М., Зайцев В. В. и др. Анализ анатомии межжелудочковой перегородки при обструктивных формах гипертрофической кардиомиопатии. Кардиология и сердечно-сосудистая хирургия. 2025;18(1):15-22. doi:10.17116/kardio20251801115.
286. Falk RH. Diagnosis and management of the cardiac amyloidoses. Circulation. 2005;112(13):2047-60. doi:10.1161/CIRCULATIONAHA.104.489187.
287. Gillmore JD, Maurer MS, Falk RH, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016;133(24):2404-12. doi:10.1161/CIRCULATIONAHA.116.021612.
288. Quarta CC, Guidalotti PL, Longhi S, et al. Defining the diagnosis in echocardiographically suspected senile systemic amyloidosis. JACC Cardiovasc Imaging. 2012;5(7):755-8. doi:10.1016/j.jcmg.2012.02.015.
289. Syed IS, Glockner JF, Feng DL, et al. Role of Cardiac Magnetic Resonance Imaging in the Detection of Cardiac Amyloidosis. JACC Cardiovasc Imaging. 2010;3(2):155-64. doi:10.1016/j.jcmg.2009.09.023.
290. Vogelsberg H, Mahrholdt H, Deluigi CC, et al. Cardiovascular Magnetic Resonance in Clinically Suspected Cardiac Amyloidosis. Noninvasive Imaging Compared to Endomyocardial Biopsy. J Am Coll Cardiol. 2008;51(10):1022-30. doi:10.1016/j.jacc.2007.10.049.
291. Dungu JN, Valencia O, Pinney JH, et al. CMR-based differentiation of AL and ATTR cardiac amyloidosis. JACC Cardiovasc Imaging. 2014;7(2):133-42. doi:10.1016/J. JCMG.2013.08.015.
292. Moon JCC, Fisher NG, McKenna WJ, Pennell DJ. Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart. 2004;90(6):645-9. doi:10.1136/hrt.2003.014969.
293. O’Hanlon R, Assomull RG, Prasad SK. Use of cardiovascular magnetic resonance for diagnosis and management in hypertrophic cardiomyopathy. Curr Cardiol Rep. 2007;9(1):51-6. doi:10.1007/s11886-007-0010-0.
294. Webb J, Fovargue L, Tøndel K, et al. The Emerging Role of Cardiac Magnetic Resonance Imaging in the Evaluation of Patients with HFpEF. Curr Heart Fail Rep. 2018;15(1):1-9. doi:10.1007/s11897-018-0372-1.
295. Patel P, Dhillon A, Popovic ZB, et al. Left ventricular outflow tract obstruction in hypertrophic cardiomyopathy patients without severe septal hypertrophy: Implications of mitral valve and papillary muscle abnormalities assessed using cardiac magnetic resonance and echocardiography. Circ Cardiovasc Imaging. 2015;8(7): e003132. doi:10.1161/CIRCIMAGING.115.003132.
296. Olivotto I, Maron MS, Autore C, et al. Assessment and Significance of Left Ventricular Mass by Cardiovascular Magnetic Resonance in Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2008;52(7):559-66. doi:10.1016/j.jacc.2008.04.047.
297. Rudolph A, Abdel-Aty H, Bohl S, et al. Noninvasive Detection of Fibrosis Applying Contrast-Enhanced Cardiac Magnetic Resonance in Different Forms of Left Ventricular Hypertrophy. Relation to Remodeling. J Am Coll Cardiol. 2009;53(3):284-91. doi:10.1016/j.jacc.2008.08.064.
298. Gruner C, Chan RH, Crean A, et al. Significance of left ventricular apical-basal muscle bundle identified by cardiovascular magnetic resonance imaging in patients with hypertrophic cardiomyopathy. Eur Heart J. 2014;35(39):2706-13. doi:10.1093/eurheartj/ehu154.
299. Brouwer WP, Germans T, Head MC, et al. Multiple myocardial crypts on modified longaxis view are a specific finding in pre-hypertrophic HCM mutation carriers. Eur Hear J Cardiovasc Imaging. 2012;13(4):292-7. doi:10.1093/ehjci/jes005.
300. Sado DM, White SK, Piechnik SK, et al. Identification and assessment of anderson-fabry disease by cardiovascular magnetic resonance noncontrast myocardial T1 mapping. Circ Cardiovasc Imaging. 2013;6(3):392-8. doi:10.1161/CIRCIMAGING.112.000070.
301. Maron BJ, Pelliccia A, Spirito P. Cardiac disease in young trained athletes: Insights into methods for distinguishing athlete’s heart from structural heart disease, with particular emphasis on hypertrophic cardiomyopathy. Circulation. 1995;91(5):1596-601. doi:10.1161/01.CIR.91.5.1596.
302. Schroeder S, Achenbach S, Bengel F, et al. Cardiac Computed Tomography: Indications, Applications, Limitations, and Training Requirements: Report of a Writing Group Deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuc. Eur Hear J. 2008;29(4):531-56.
303. Esposito A, Colantoni C, De Cobelli F, et al. Multidetector computed tomography for coronary stents imaging: High-voltage (140-KVP) prospective ecg-triggered versus standard-voltage (120-kvp) retrospective ecg-gated helical scanning. J Comput Assist Tomogr. 2013;37(3):395-401. doi:10.1097/RCT.0b013e3182873559.
304. Shiozaki AA, Senra T, Arteaga E, et al. Myocardial fibrosis detected by cardiac CT predicts ventricular fibrillation/ventricular tachycardia events in patients with hypertrophic cardiomyopathy.JCardiovascComputTomogr.2013;7(3):173-81.doi:10.1016/j.jcct.2013.04.002.
305. Rapezzi C, Quarta CC, Guidalotti PL, et al. Usefulness and limitations of 99mTc-3, 3-diphosphono-1, 2-propanodicarboxylic acid scintigraphy in the aetiological diagnosis of amyloidotic cardiomyopathy. Eur J Nucl Med Mol Imaging. 2011;38(3):470-8. doi:10.1007/s00259-010-1642-7.
306. Rapezzi C, Quarta CC, Guidalotti PL, et al. Role of 99mTc-DPD scintigraphy in diagnosis and prognosis of hereditary transthyretin-related cardiac amyloidosis. JACC Cardiovasc Imaging. 2011;4(6):659-70. doi:10.1016/j.jcmg.2011.03.016.
307. Dorbala S, Ando Y, Bokhari S, et al. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI Expert Consensus Recommendations for Multimodality Imaging in Cardiac Amyloidosis: Part 1 of 2-Evidence Base and Standardized Methods of Imaging. J Card Fail. 2019;25(11): e1-39. doi:10.1016/j.cardfail.2019.08.001.
308. Dorbala S, Ando Y, Bokhari S, et al. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI Expert Consensus Recommendations for Multimodality Imaging in Cardiac Amyloidosis: Part 2 of 2—Diagnostic Criteria and Appropriate Utilization. J Card Fail. 2019;25(11):85465. doi:10.1016/j.cardfail.2019.08.002.
309. Kawai C, Sakurai T, Fujiwara H, et al. Hypertrophic obstructive and non-obstructive cardiomyopathy in Japan. Diagnosis of the disease with special reference to endomyocardial catheter biopsy. Eur Hear J. 1983;4(1):121-5.
310. Scalone G, Niccoli G, Crea F. Editor’s ChoicePathophysiology, diagnosis and management of MINOCA: an update. Eur Hear Journal Acute Cardiovasc Care. 2019;8(1):54-62. doi:10.1177/2048872618782414.
311. Mitsutake R, Miura S, Sako H, et al. Usefulness of multi-detector row computed tomography for the management of percutaneous transluminal septal myocardial ablation in patient with hypertrophic obstructive cardiomyopathy. Int J Cardiol. 2008;129(2):61-3. doi:10.1016/j.ijcard.2007.06.132.
312. Okayama S, Uemura S, Soeda T, et al. Role of cardiac computed tomography in planning and evaluating percutaneous transluminal septal myocardial ablation for hypertrophic obstructive cardiomyopathy. J Cardiovasc Comput Tomogr. 2010;4(1):62-5. doi:10.1016/j.jcct.2009.10.004.
313. Villa ADM, Sammut E, Zarinabad N, et al. Microvascular ischemia in hypertrophic cardiomyopathy: New insights from high-resolution combined quantification of perfusion and late gadolinium enhancement. J Cardiovasc Magn Reson. 2016;18: Article number 4 (2015). doi:10.1186/s12968-016-0223-8.
314. Chen JM, Levin HR, Michler RE, et al. Reevaluating the significance of pulmonary hypertension before cardiac transplantation: Determination of optimal thresholds and quantification of the effect of reversibility on perioperative mortality. J Thorac Cardiovasc Surg. 1997;114(4):627-34. doi:10.1016/S0022-5223(97)70053-9.
315. Kato TS, Takayama H, Yoshizawa S, et al. Cardiac transplantation in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2012;110(4):568-74. doi:10.1016/j.amjcard.2012.04.030.
316. Lindelöw B, Andersson B, Waagstein F, Bergh CH. High and low pulmonary vascular resistance in heart transplant candidates. A 5-year follow-up after heart transplantation shows continuous reduction in resistance and no difference in complication rate. Eur Heart J. 1999;20(2):148-56. doi:10.1053/euhj.1998.1155.
317. Maron MS, Kalsmith BM, Udelson JE, et al. Survival after cardiac transplantation in patients with hypertrophic cardiomyopathy. Circ Hear Fail. 2010;3(5):574-9. doi:10.1161/CIRCHEARTFAILURE.109.922872.
318. Mehra MR, Kobashigawa J, Starling R, et al. Listing Criteria for Heart Transplantation: International Society for Heart and Lung Transplantation Guidelines for the Care of Cardiac Transplant Candidates-2006. J Hear Lung Transplant. 2006;25(9):1024-42. doi:10.1016/j.healun.2006.06.008.
319. Torres MF, Perez-Villa F. Heart transplantation in patients with hypertrophic cardiomyopathy. Glob Cardiol Sci Pract. 2018;2018(3):32. doi:10.21542/gcsp.2018.32.
320. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC Guidelines for the Management of Patients with Supraventricular Arrhythmias — Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology. J Am Coll Cardiol. 2003;42(8):1493-531. doi:10.1016/j.jacc.2003.08.013.
321. Bokeria LA, Berseneva MI, Malenkov DA. Arrhythmogenic complications of hypertrophic cardiomyopathy. Annals of arrhythmology. 2010;7(3):62-9. (In Russ.) Бокерия Л. А., Берсенёва М. И., Маленков Д. А. Аритмогенные осложнения гипертрофической кардиомиопатии. Анналы аритмологии. 2010;7(3):62-9.
322. Muresan L, Cismaru G, Martins RP, et al. Recommendations for the use of electrophysiological study: Update 2018. Hell J Cardiol. 2019;60(2):82-100. doi:10.1016/j.hjc.2018.09.002.
323. Wang W, Lian Z, Rowin EJ, et al. Prognostic Implications of Nonsustained Ventricular Tachycardia in High-Risk Patients With Hypertrophic Cardiomyopathy. Circ Arrhythm Electrophysiol. 2017;10(3): e004604. doi:10.1161/CIRCEP.116.004604.
324. Inada K, Seiler J, Roberts-Thomson KC, et al. Substrate characterization and catheter ablation for monomorphic ventricular tachycardia in patients with apical hypertrophic cardiomyopathy. J Cardiovasc Electrophysiol. 2011;22(1):41-8. doi:10.1111/j.15408167.2010.01875.x.
325. Lim KK, Maron BJ, Knight BP. Successful catheter ablation of hemodynamically unstable monomorphic ventricular tachycardia in a patient with hypertrophic cardiomyopathy and apical aneurysm. J Cardiovasc Electrophysiol. 2009;20(4):445-7. doi:10.1111/j.15408167.2008.01366.x.
326. Refaat MM, Hotait M, Tseng ZH. Utility of the exercise electrocardiogram testing in sudden cardiac death risk stratification. Ann Noninvasive Electrocardiol. 2014;19(4):311-8. doi:10.1111/anec.12191.
327. Yi G, Poloniecki J, Dickie S, et al. Can the Assessment of Dynamic QT Dispersion on Exercise Electrocardiogram Predict Sudden Cardiac Death in Hypertrophic Cardiomyopathy? Pacing Clin Electrophysiol. 2000;23(11Pt2):1953-6. doi:10.1111/j.1540-8159.2000.tb07060.x.
328. Nistri S, Olivotto I, Maron MS, et al. β-blockers for prevention of exercise-induced left ventricular outflow tract obstruction in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2012;110(5):715-9. doi:10.1016/j.amjcard.2012.04.051.
329. Rowin EJ, Maron BJ, Olivotto I, Maron MS. Role of Exercise Testing in Hypertrophic Cardiomyopathy. JACC Cardiovasc Imaging. 2017;10(11):1374-86. doi:10.1016/j.jcmg.2017.07.016.
330. Yalçin F, Muderrisoglu H, Korkmaz ME, et al. The effect of dobutamine stress on left ventricular outflow tract gradients in hypertensive patients with basal septal hypertrophy. Angiology. 2004;55(3):295-301. doi:10.1177/000331970405500309.
331. Mancini DM, Eisen H, Kussmaul W, et al. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation. 1991;83(3):778-86. doi:10.1161/01.CIR.83.3.778.
332. Sharma S, Elliott P, Whyte G, et al. Utility of cardiopulmonary exercise in the assessment of clinical determinants of functional capacity in hypertrophic cardiomyopathy. Am J Cardiol. 2000;86(2):162-8. doi:10.1016/S0002-9149(00)00854-7.
333. Колоскова Н. Н., Шаталов К. В., Бокерия Л. А. Определение пикового потребления кислорода: клиническое использование и перспективы. Креативная кардиология. 2014;2:20-8.
334. Coats CJ, Rantell K, Bartnik A, et al. Cardiopulmonary Exercise Testing and Prognosis in Hypertrophic Cardiomyopathy. Circ Hear Fail. 2015;8(6):1022-31. doi:10.1161/ CIRCHEARTFAILURE.114.002248.
335. Arena R, Owens DS, Arevalo J, et al. Ventilatory efficiency and resting hemodynamics in hypertrophic cardiomyopathy. Med Sci Sports Exerc. 2008;40(5):799-805. doi:10.1249/MSS.0b013e31816459a1.
336. Olivotto I, Maron BJ, Montereggi A, et al. Prognostic value of systemic blood pressure response during exercise in a community-based patient population with hypertrophic cardiomyopathy. J Am Coll Cardiol. 1999;33(7):2044-51. doi:10.1016/S0735-1097(99)00094-7.
337. Bennett MK, Gilotra NA, Harrington C, et al. Evaluation of the role of endomyocardial biopsy in 851 patients with unexplained heart failure from 2000-2009. Circ Hear Fail. 2013;6(4):676-84. doi:10.1161/CIRCHEARTFAILURE.112.000087.
338. Leone O, Veinot JP, Angelini A, et al. 2011 Consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology. Cardiovasc Pathol. 2012;21(4):245-74. doi:10.1016/j.carpath.2011.10.001.
339. Quarta CC, Gonzalez-Lopez E, Gilbertson JA, et al. Diagnostic Sensitivity of Abdominal Fat Aspiration in Cardiac Amyloidosis. Eur Hear J. 2017;38(24):1905-8.
340. Schönland SO, Hegenbart U, Bochtler T, et al. Immunohistochemistry in the classification of systemic forms of amyloidosis: A systematic investigation of 117 patients. Blood. 2012;119(2):488-93. doi:10.1182/blood-2011-06-358507.
341. Крылова Н. С., Хашиева Ф. М., Демкина А. Е. и др. Гипертрофическая кардиомиопатия и артериальная гипертензия: возможно ли сочетание? Сердце. Журнал для практикующих врачей. 2015;14(3(83)):164-9.
342. Полякова А. А., Гудкова А. Я., Крутиков А. Н. и др. Гипертрофическая кардиомиопатия в старшей возрастной группе: влияние факторов кардиометаболического риска и полиморфизма гена MADD. Артериальная гипертензия. 2018;24(1):29-40.
343. Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity. Physiol Rev. 2008:389-419. doi:10.1152/physrev.00017.2007.
344. Ommen SR, Lopez-Jimenez F. Obesity and hypertrophic cardiomyopathy: Chickens, eggs, and causality: Clinical skills remain the key to caring for patients. J Am Coll Cardiol. 2013;62(5):458-9. doi:10.1016/j.jacc.2013.03.063.
345. Olivotto I, Maron BJ, Tomberli B, et al. Obesity and its association to phenotype and clinical course in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2013;62(5):449-57. doi:10.1016/j.jacc.2013.03.062.
346. Di Tommaso L, Stassano P, Mannacio V, et al. Asymmetric septal hypertrophy in patients with severe aortic stenosis: The usefulness of associated septal myectomy. J Thorac Cardiovasc Surg. 2013;145(1):171-5. doi:10.1016/j.jtcvs.2011.10.096.
347. Dweck MR, Joshi S, Murigu T, et al. Left ventricular remodeling and hypertrophy in patients with aortic stenosis: Insights from cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2012;14(1):50. doi:10.1186/1532-429X-14-50.
348. Katayama M, Panse PM, Kendall CB, et al. Left ventricular septal hypertrophy in elderly patients with aortic stenosis. J Ultrasound Med. 2017;37(1):217-24. doi:10.1002/jum.14320.
349. Maron BJ, Edwards J, Epstein SE. Disproportionate ventricular septal thickening in patients with systemic hypertension. Chest. 1978;73(4):466-70. doi:10.1378/chest.73.4.466.
350. Rodrigues JCL, Amadu AM, Dastidar AG, et al. Prevalence and Predictors of Asymmetric Hypertensive Heart Disease: Insights From Cardiac and Aortic Function With Cardiovascular Magnetic Resonance. Eur Hear J Cardiovasc Imaging. 2016;17(12):1405-13.
351. Tuseth N, Cramariuc D, Rieck ÅE, et al. Asymmetric septal hypertrophy — A marker of hypertension in aortic stenosis (a SEAS substudy). Blood Press. 2010;19(3):140-4. doi:10.3109/08037051.2010.481816.
352. Van Straten AHM, Soliman Hamad MA, Peels KCH, et al. Increased septum wall thickness in patients undergoing aortic valve replacement predicts worse late survival. Ann Thorac Surg. 2012;94(1):66-71. doi:10.1016/j.athoracsur.2012.03.027.
353. Shapiro LM, Howat AP, Crean PA, Westgate CJ. An echocardiographic study of localized subaortic hypertrophy. Eur Heart J. 1986;7(2):127-32. doi:10.1093/oxfordjournals.eurheartj.a062034.
354. Gutiérrez-Barrios A, Camacho-Jurado F, Díaz-Retamino E, et al. Invasive assessment of coronary microvascular dysfunction in hypertrophic cardiomyopathy: The index of microvascular resistance. Cardiovasc Revascularization Med. 2015;16(7):426-8. doi:10.1016/j.carrev.2015.06.008.
355. Ismail TF, Hsu LY, Greve AM, et al. Coronary microvascular ischemia in hypertrophic cardiomyopathy — A pixel-wise quantitative cardiovascular magnetic resonance perfusion study. J Cardiovasc Magn Reson. 2014;16(1):49. doi:10.1186/s12968-014-0049-1.
356. Olivotto I, Girolami F, Sciagr R, et al. Microvascular function is selectively impaired in patients with hypertrophic cardiomyopathy and sarcomere myofilament gene mutations. J Am Coll Cardiol. 2011;58(8):839-48. doi:10.1016/j.jacc.2011.05.018.
357. Raissuni Z, Doghmi N, Mousseaux E, et al. Hypertrophic cardiomyopathy mimicking STEMI: The role of cardiac magnetic resonance imaging in the detection of microvascular coronary dysfunction. Diagn Interv Imaging. 2014;95(11):1111-2. doi:10.1016/j.diii.2013.12.020.
358. Timmer SAJ, Knaapen P. Coronary Microvascular Function, Myocardial Metabolism, and Energetics in Hypertrophic Cardiomyopathy: Insights From Positron Emission Tomography. Eur Hear J Cardiovasc Imaging. 2013;14(2):95-101.
359. Zhang YD, Li M, Qi L, et al. Hypertrophic cardiomyopathy: Cardiac structural and microvascular abnormalities as evaluated with multi-parametric MRI. Eur J Radiol. 2015;84(8):1480-6. doi:10.1016/j.ejrad.2015.04.028.
360. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation. 2006;114(10): e385-484. doi:10.1161/CIRCULATIONAHA.106.178233.
361. Basavarajaiah S, Wilson M, Whyte G, et al. Prevalence of Hypertrophic Cardiomyopathy in Highly Trained Athletes. Relevance to Pre-Participation Screening. J Am Coll Cardiol. 2008;51(10):1033-9. doi:10.1016/j.jacc.2007.10.055.
362. Malhotra A, Sharma S. Hypertrophic cardiomyopathy in athletes. Eur Cardiol Rev. 2017;12(2):80-2. doi:10.15420/ecr.2017:12:1.
363. Pelliccia A, Corrado D, Bjãrnstad HH, et al. Recommendations for participation in competitive sport and leisure-time physical activity in individuals with cardiomyopathies, myocarditis and pericarditis. Eur J Prev Cardiol. 2006;13(6):876-85. doi:10.1097/01.hjr.0000238393.96975.32.
364. Liebregts M, Faber L, Jensen MK, et al. Validation of the HCM Risk-SCD model in patients with hypertrophic cardiomyopathy following alcohol septal ablation. Europace. 2018;20(FI2):198-203. doi:10.1093/europace/eux251.
365. Vriesendorp PA, Schinkel AFL, Liebregts M, et al. Validation of the 2014 European Society of Cardiology Guidelines Risk Prediction Model for the Primary Prevention of Sudden Cardiac Death in Hypertrophic Cardiomyopathy. Circ Arrhythmia Electrophysiol. 2015;8(4):829-35. doi:10.1161/CIRCEP.114.002553.
366. Tsuda T, Hayashi K, Konno T, et al. J Waves for Predicting Cardiac Events in Hypertrophic Cardiomyopathy. JACC Clin Electrophysiol. 2017;3(10):1136-42. doi:10.1016/J. JACEP.2017.03.010.
367. Veselka J, Liebregts M, Cooper R, et al. Prediction of Sudden Cardiac Arrest After Alcohol Septal Ablation for Hypertrophic Obstructive Cardiomyopathy: ASA-SCARRE Risk Score. Am J Cardiol. 2022;184:120-6. doi:10.1016/J.AMJCARD.2022.08.028.
368. Spoladore R, Maron MS, D’Amato R, et al. Pharmacological Treatment Options for Hypertrophic Cardiomyopathy: High Time for Evidence. Eur Hear J. 2012;33(14):1724-33.
369. Patten M, Pecha S, Aydin A. Atrial Fibrillation in Hypertrophic Cardiomyopathy: Diagnosis and Considerations for Management. J Atr Fibrillation. 2018;10(5):1556.
370. Rujirachun P, Charoenngam N, Wattanachayakul P, et al. Efficacy and safety of direct oral anticoagulants (DOACs) versus vitamin K antagonist (VKA) among patients with atrial fibrillation and hypertrophic cardiomyopathy: a systematic review and meta-analysis. Acta Cardiol. 2019;75(8):724-31. doi:10.1080/00015385.2019.1668113.
371. Maron BJ, Casey SA, Olivotto I, et al. Clinical Course and Quality of Life in High-Risk Patients With Hypertrophic Cardiomyopathy and Implantable Cardioverter-Defibrillators. Circ Arrhythm Electrophysiol. 2018;11(4). doi:10.1161/CIRCEP.117.005820.
372. Klopotowski M, Kukula K, Jamiolkowski J, et al. Sudden Cardiac Death Risk over Time in HCM Patients with Implantable Cardioverter-Defibrillator. J Clin Med. 2022;11(6). doi:10.3390/JCM11061633.
373. Lambiase PD, Barr C, Theuns DAMJ, et al. Worldwide Experience With a Totally Subcutaneous Implantable Defibrillator: Early Results From the EFFORTLESS S-ICD Registry. Eur Hear J. 2014;35(25):1657-65.
374. Dearani JA, Ommen SR, Gersh BJ, et al. Surgery Insight: Septal myectomy for obstructive hypertrophic cardiomyopathy — The Mayo Clinic experience. Nat Clin Pract Cardiovasc Med. 2007;4(9):503-12. doi:10.1038/ncpcardio0965.
375. Leonardi RA, Kransdorf EP, Simel DL, Wang A. Meta-analyses of septal reduction therapies for obstructive hypertrophic cardiomyopathy comparative rates of overall mortality and sudden cardiac death after treatment. Circ Cardiovasc Interv. 2010;3(2):97-104. doi:10.1161/CIRCINTERVENTIONS.109.916676.
376. Afanasyev AV, Bogachev-Prokophiev AV, Ovcharov MA, et al. Single-Centre Experience of Surgical Myectomy for Hypertrophic Obstructive Cardiomyopathy. Hear Lung Circ. 2019;29(6):949-55. doi:10.1016/j.hlc.2019.07.009.
377. Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Rev Esp Cardiol (Engl Ed). 2022;75(5):429. doi:10.1016/ J.REC.2022.04.003.
378. Ammirati E, Contri R, Coppini R, et al. Pharmacological treatment of hypertrophic cardiomyopathy: current practice and novel perspectives. Eur J Heart Fail. 2016;18(9):1106-18. doi:10.1002/ejhf.541.
379. Udelson JE, Bonow RO, O’Gara PT, et al. Verapamil prevents silent myocardial perfusion abnormalities during exercise in asymptomatic patients with hypertrophic cardiomyopathy. Circulation. 1989;79(5):1052-60. doi:10.1161/01.CIR.79.5.1052.
380. Sherrid MV, Shetty A, Winson G, et al. Treatment of obstructive hypertrophic cardiomyopathy symptoms and gradient resistant to first-line therapy with β-blockade or verapamil. Circ Hear Fail. 2013;6(4):694-702. doi:10.1161/CIRCHEARTFAILURE.112.000122.
381. Sherrid MV. Drug Therapy for Hypertrophic Cardiomypathy: Physiology and Practice. Curr Cardiol Rev. 2016;12(1):52-65. doi:10.2174/1573403x1201160126125403.
382. Monda E, Lioncino M, Palmiero G, et al. Bisoprolol for treatment of symptomatic patients with obstructive hypertrophic cardiomyopathy. The BASIC (bisoprolol AS therapy in hypertrophic cardiomyopathy) study. Int J Cardiol. 2022;354:22-8. doi:10.1016/J.IJCARD.2022.03.013.
383. Dybro AM, Rasmussen TB, Nielsen RR, et al. Metoprolol Improves Left Ventricular Longitudinal Strain at Rest and during Exercise in Obstructive Hypertrophic Cardiomyopathy. J Am Soc Echocardiogr. 2023;36(2):196-204. doi:10.1016/J.ECHO.2022.09.008.
384. Toshima H, Koga Y, Nagata H, et al. Comparable effects of oral diltiazem and verapamil in the treatment of hypertrophic cardiomyopathy. Double-blind crossover study. Jpn Hear J. 1986;27(5):701-15. doi:10.1536/ihj.27.701.
385. Bonow RO, Dilsizian V, Rosing DR, et al. Verapamil-induced improvement in left ventricular diastolic filling and increased exercise tolerance in patients with hypertrophic cardiomyopathy: Shortand long-term effects. Circulation. 1985;72(4):853-64. doi:10.1161/01. CIR.72.4.853.
386. Tezuka A, Higo K, Nakamukae Y, et al. Bisoprolol successfully improved the intraventricular pressure gradient in a patient with midventricular obstructive hypertrophic cardiomyopathy with an apex aneurysm due to apical myocardial damage. Intern Med. 2019;58(4): 535-9. doi:10.2169/internalmedicine.0997-18.
387. Said SM, Schaff HV, Abel MD, Dearani JA. Transapical approach for apical myectomy and relief of midventricular obstruction in hypertrophic cardiomyopathy. J Card Surg. 2012;27(4):443-8. doi:10.1111/j.1540-8191.2012.01475.x.
388. Богачев-Прокофьев А. В., Железнев С. И., Фоменко М.С. и др. Эффективность расширенной миоэктомии у пациентов с желудочковой обструкцией при гипертрофической кардиомиопатии. Кардиология. 2017;57(5):38-43.
389. Nguyen A, Schaff HV. Surgical Myectomy: Subaortic, Midventricular, and Apical. Cardiol Clin. 2019;37(1):95-104. doi:10.1016/J.CCL.2018.08.006.
390. Schaff HV, Brown ML, Dearani JA, et al. Apical myectomy: a new surgical technique for management of severely symptomatic patients with apical hypertrophic cardiomyopathy. J Thorac Cardiovasc Surg. 2010;139(3):634-40. doi:10.1016/J.JTCVS.2009.07.079.
391. Batzner A, Schäfers H-J, Borisov KV, Seggewiß H. Hypertrophic Obstructive Cardiomyopathy. Dtsch Arztebl Int. 2019;116(4):47-53. doi:10.3238/ARZTEBL.2019.0047.
392. Epstein SE, Rosing DR. Verapamil: Its potential for causing serious complications in patients with hypertrophic cardiomyopathy. Circulation. 1981;64(3):437-41. doi:10.1161/01.CIR.64.3.437.
393. Maron BJ, Rowin EJ, Casey SA, et al. Hypertrophic Cardiomyopathy in Adulthood Associated With Low Cardiovascular Mortality With Contemporary Management Strategies. J Am Coll Cardiol. 2015;65(18):1915-28. doi:10.1016/J.JACC.2015.02.061.
394. Charron P, Elliott PM, Gimeno JR, et al. The Cardiomyopathy Registry of the EURObservational Research Programme of the European Society of Cardiology: baseline data and contemporary management of adult patients with cardiomyopathies. Eur Heart J. 2018;39(20):1784-93. doi:10.1093/EURHEARTJ/EHX819.
395. Olivotto I, Cecchi F, Casey SA, et al. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001;104(21):2517-24. doi:10.1161/hc4601.097997.
396. Kuperstein R, Klempfner R, Ofek E, et al. De novo mitral regurgitation as a cause of heart failure exacerbation in patients with hypertrophic cardiomyopathy. Int J Cardiol. 2018;252:122-7. doi:10.1016/J.IJCARD.2017.11.060.
397. Subramanian M, Sravani V, Krishna SP, et al. Efficacy of SGLT2 Inhibitors in Patients With Diabetes and Nonobstructive Hypertrophic Cardiomyopathy. Am J Cardiol. 2023;188: 80-6. doi:10.1016/J.AMJCARD.2022.10.054.
398. Maron MS, Chan RH, Kapur NK, et al. Effect of Spironolactone on Myocardial Fibrosis and Other Clinical Variables in Patients with Hypertrophic Cardiomyopathy. Am J Med. 2018;131(7):837-41. doi:10.1016/j.amjmed.2018.02.025.
399. Olivotto I, Oreziak A, Barriales-Villa R, et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, doubleblind, placebo-controlled, phase 3 trial. Lancet (London, England). 2020;396(10253):7569. doi:10.1016/S0140-6736(20)31792-X.
400. Pelliccia F, Cecchi F, Olivotto I, Camici PG. Microvascular Dysfunction in Hypertrophic Cardiomyopathy. J Clin Med. 2022;11(21):6560. doi:10.3390/JCM11216560.
401. Cannon RO, Rosing DR, Maron BJ, et al. Myocardial ischemia in patients with hypertrophic cardiomyopathy: contribution of inadequate vasodilator reserve and elevated left ventricular filling pressures. Circulation. 1985;71(2):234-43. doi:10.1161/01.CIR.71.2.234.
402. Krams R, Kofflard MJM, Duncker DJ, et al. Decreased coronary flow reserve in hypertrophic cardiomyopathy is related to remodeling of the coronary microcirculation. Circulation. 1998;97(3):230-3. doi:10.1161/01.CIR.97.3.230.
403. Shariat M, Thavendiranathan P, Nguyen E, et al. Utility of coronary CT angiography in outpatients with hypertrophic cardiomyopathy presenting with angina symptoms. J Cardiovasc Comput Tomogr. 2014;8(6):429-37. doi:10.1016/J.JCCT.2014.09.007.
404. van der Velde N, Huurman R, Yamasaki Y, et al. Frequency and Significance of Coronary Artery Disease and Myocardial Bridging in Patients With Hypertrophic Cardiomyopathy. Am J Cardiol. 2020;125(9):1404-12. doi:10.1016/J.AMJCARD.2020.02.002.
405. Dias A, Núñez Gil IJ, Santoro F, et al. Takotsubo syndrome: State-of-the-art review by an expert panel — Part 2. Cardiovasc Revasc Med. 2019;20(2):153-66. doi:10.1016/J.CARREV.2018.11.016.
406. Pelliccia F, Limongelli G, Autore C, et al. Sex-related differences in cardiomyopathies. Int J Cardiol. 2019;286:239-43. doi:10.1016/J.IJCARD.2018.10.091.
407. Crea F, Camici PG, Merz CNB. Coronary microvascular dysfunction: an update. Eur Heart J. 2014;35(17):1101-11. doi:10.1093/EURHEARTJ/EHT513.
408. Puwanant S, Trongtorsak A, Wanlapakorn C, et al. Acute coronary syndrome with nonobstructive coronary arteries (ACS-NOCA) in patients with hypertrophic cardiomyopathy. BMC Cardiovasc Disord. 2021;21(1):556. doi:10.1186/S12872-021-02373-Z.
409. Российское кардиологическое общество (РКО). Стабильная ишемическая болезнь сердца. Клинические рекомендации 2020. Российский кардиологический журнал. 2020;25(11):4076. doi:10.15829/29/1560-4071-2020-4076.
410. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41(37):3504-20. doi:10.1093/EURHEARTJ/EHAA503.
411. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407-77. doi:10.1093/EURHEARTJ/EHZ425.
412. Dybro AM, Rasmussen TB, Nielsen RR, et al. Randomized Trial of Metoprolol in Patients With Obstructive Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2021;78(25):2505-17. doi:10.1016/J.JACC.2021.07.065.
413. Wilmshurst PT, Thompson DS, Juul SM, et al. Effects of verapamil on haemodynamic function and myocardial metabolism in patients with hypertrophic cardiomyopathy. Heart. 1986;56(6):544-53. doi:10.1136/hrt.56.6.544.
414. Petkow Dimitrow P, Krzanowski M, Nizankowski R, et al. Effect of verapamil on systolic and diastolic coronary blood flow velocity in asymptomatic and mildly symptomatic patients with hypertrophic cardiomyopathy. Heart. 2000;83(3):262-6. doi:10.1136/HEART.83.3.262.
415. Mengesha HG, Weldearegawi B, Petrucka P, et al. Effect of ivabradine on cardiovascular outcomes in patients with stable angina: meta-analysis of randomized clinical trials. BMC Cardiovasc Disord. 2017;17(1):105. doi:10.1186/S12872-017-0540-3.
416. Gupta T, Harikrishnan P, Kolte D, et al. Outcomes of acute myocardial infarction in patients with hypertrophic cardiomyopathy. Am J Med. 2015;128(8):879-87.e1. doi:10.1016/J.AMJMED.2015.02.025.
417. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20): e618-51. doi:10.1161/CIR.0000000000000617.
418. Yang YJ, Fan CM, Yuan JQ, et al. Long-term survival after acute myocardial infarction in patients with hypertrophic cardiomyopathy. Clin Cardiol. 2017;40(1):26-31. doi:10.1002/CLC.22601.
419. Tamis-Holland JE, Jneid H, Reynolds HR, et al. Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association. Circulation. 2019;139(18): E891-908. doi:10.1161/CIR.0000000000000670.
420. Российское кардиологическое общество (РКО). Острый инфаркт миокарда с подъемом сегмента ST электрокардиограммы. Клинические рекомендации 2020. Российский кардиологический журнал. 2020;25(11):4103. doi:10.15829/29/15604071-2020-4103.
421. Барбараш О. Л., Дупляков Д. В., Затейщиков Д. А. и др. Острый коронарный синдром без подъема сегмента ST электрокардиограммы. Клинические рекомендации 2020. Российский кардиологический журнал. 2021;26(4):4449. doi:10.15829/1560-4071-2021-4449.
422. De Filippo O, Russo C, Manai R, et al. Impact of secondary prevention medical therapies on outcomes of patients suffering from Myocardial Infarction with NonObstructive Coronary Artery disease (MINOCA): A meta-analysis. Int J Cardiol. 2022;368(1):1-9. doi:10.1016/J.IJCARD.2022.08.034.
423. Samaras A, Papazoglou AS, Balomenakis C, et al. Prognostic impact of secondary prevention medical therapy following myocardial infarction with non-obstructive coronary arteries: a Bayesian and frequentist meta-analysis. Eur Hear J Open. 2022;2(6):077. doi:10.1093/EHJOPEN/OEAC077.
424. Abdu FA, Liu L, Mohammed AQ, et al. Effect of Secondary Prevention Medication on the Prognosis in Patients With Myocardial Infarction With Nonobstructive Coronary Artery Disease. J Cardiovasc Pharmacol. 2020;76(6):678-83. doi:10.1097/FJC. 0000000000000918.
425. Paolisso P, Bergamaschi L, Saturi G, et al. Secondary Prevention Medical Therapy and Outcomes in Patients With Myocardial Infarction With Non-Obstructive Coronary Artery Disease. Front Pharmacol. 2020;10:1606. doi:10.3389/FPHAR.2019.01606.
426. Bossard M, Gao P, Boden W, et al. Antiplatelet therapy in patients with myocardial infarction without obstructive coronary artery disease. Heart. 2021;107(21):1739-47. doi:10.1136/HEARTJNL-2020-318045.
427. Аверков О. В., Арутюнян Г. К., Дупляков Д. В. и др. Острый инфаркт миокарда без подъема сегмента ST электрокардиограммы. Клинические рекомендации 2024. Российский кардиологический журнал. 2025;30(5):6319. doi:10.15829/1560-4071-2025-6319. EDN CXJUIB.
428. Кобалава Ж. Д., Конради А. О., Недогода С. В. и др. Артериальная гипертензия у взрослых. Клинические рекомендации 2024. Российский кардиологический журнал. 2024;29(9):6117. doi:10.15829/1560-4071-2024-6117. EDN GUEWLU.
429. Rosing DR, Idänpään-Heikkilä U, Maron BJ, et al. Use of calcium-channel blocking drugs in hypertrophic cardiomyopathy. Am J Cardiol. 1985;55(3). doi:10.1016/00029149(85)90630-7.
430. Betocchi S, Piscione F, Losi MA, et al. Effects of diltiazem on left ventricular systolic and diastolic function in hypertrophic cardiomyopathy. Am J Cardiol. 1996;78(4):451-7. doi:10.1016/S0002-9149(96)00336-0.
431. López-Sendón J, Swedberg K, McMurray J, et al. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341-62. doi:10.1016/J. EHJ.2004.06.002.
432. Maron BJ. Hypertrophic Cardiomyopathy: A Systematic Review. JAMA. 2002;287(10): 1308-20.
433. Maron BJ, Olivotto I, Bellone P, et al. Clinical profile of stroke in 900 patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;39(2):301-7. doi:10.1016/S07351097(01)01727-2.
434. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart R. J Am Coll Cardiol. 2019;74(1):104-32. doi:10.1016/J.JACC.2019.01.011.
435. Di Cori A, Lilli A, Zucchelli G, Zaca V. Role of cardiac electronic implantable device in the stratification and management of embolic risk of silent atrial fibrillation: are all atrial fibrillations created equal? Expert Rev Cardiovasc Ther. 2018;16(3):175-81. doi:10.1080/14779072.2018.1438267.
436. Camm CF, Camm AJ. Atrial fibrillation and anticoagulation in hypertrophic cardiomyopathy. Arrhythmia Electrophysiol Rev. 2017;6(2):63-8. doi:10.15420/aer.2017.4.2.
437. Miller CAS, Maron MS, Estes NAM, et al. Safety, Side Effects and Relative Efficacy of Medications for Rhythm Control of Atrial Fibrillation in Hypertrophic Cardiomyopathy. Am J Cardiol. 2019;123(11):1859-62. doi:10.1016/j.amjcard.2019.02.051.
438. Гринева Е. Н., Цой У. А., Каронова Т. Л. и др. Проект федеральных клинических рекомендаций по диагностике и лечению амиодарон-индуцированной дисфункции щитовидной железы. Клиническая и экспериментальная тиреоидология. 2020;16(2):12-24. doi:10.14341/KET12693.
439. Bartalena L, Bogazzi F, Chiovato L, et al. 2018 European Thyroid Association (ETA) Guidelines for the Management of Amiodarone-Associated Thyroid Dysfunction. Eur Thyroid J. 2018;7(2):55-66. doi:10.1159/000486957.
440. Theodoraki A, Vanderpump MPJ. Thyrotoxicosis associated with the use of amiodarone: the utility of ultrasound in patient management. Clin Endocrinol (Oxf). 2016;84(2):172-6. doi:10.1111/CEN.12988.
441. Zhou YY, He W, Zhou YY, Zhu W. Non-vitamin K antagonist oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation: a systematic review and metaanalysis. J Thromb Thrombolysis. 2020;50(2):311-7. doi:10.1007/s11239-019-02008-3.
442. Lee HJ, Kim HK, Jung JH, et al. Novel Oral Anticoagulants for Primary Stroke Prevention in Hypertrophic Cardiomyopathy Patients with Atrial Fibrillation. Stroke. 2019;50(9): 2582-6. doi:10.1161/STROKEAHA.119.026048.
443. Dominguez F, Climent V, Zorio E, et al. Direct oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation. Int J Cardiol. 2017;248:232-8. doi:10.1016/j.ijcard.2017.08.010.
444. Li B, Sun C, Qin F, et al. Could direct oral anticoagulants be an alternative to vitamin K antagonists in patients with hypertrophic cardiomyopathy and atrial fibrillation? Int J Cardiol. 2018;256:39. doi:10.1016/j.ijcard.2017.10.113.
445. Lozier MR, Sanchez AM, Lee JJ, et al. Thromboembolic outcomes of different anticoagulation strategies for patients with atrial fibrillation in the setting of hypertrophic cardiomyopathy: A systematic review. J Atr Fibrillation. 2019;12(4):2207. doi:10.4022/jafib.2207.
446. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The euro heart survey. Chest. 2010;138(5):1093-100. doi:10.1378/chest.10-0134.
447. Veselka J, Faber L, Liebregts M, et al. Shortand long-term outcomes of alcohol septal ablation for hypertrophic obstructive cardiomyopathy in patients with mild left ventricular hypertrophy: a propensity score matching analysis. Eur Hear J. 2019;40(21):1681-7.
448. Каштанов М. Г., Чернышев С. Д., Кардапольцев Л. В. и др. Этаноловая септальная аблация в лечении обструктивной гипертрофической кардиомиопатии: отбор пациентов и рациональность ее применения. Патология кровообращения и кардиохирургия. 2017;21(1):104-16.
449. Ommen SR, Maron BJ, Olivotto I, et al. Long-term effects of surgical septal myectomy on survival in patients with obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2005;46(3):470-6. doi:10.1016/J.JACC.2005.02.090.
450. Mitra A, Ghosh RK, Bandyopadhyay D, et al. Significance of Pulmonary Hypertension in Hypertrophic Cardiomyopathy. Curr Probl Cardiol. 2020;45(6):00398. doi:10.1016/J.CPCARDIOL.2018.10.002.
451. Desai MY, Bhonsale A, Patel P, et al. Exercise echocardiography in asymptomatic HCM: exercise capacity, and not LV outflow tract gradient predicts long-term outcomes. JACC Cardiovasc Imaging. 2014;7(1):26-36. doi:10.1016/J.JCMG.2013.08.010.
452. Nguyen A, Schaff HV, Nishimura RA, et al. Determinants of Reverse Remodeling of the Left Atrium After Transaortic Myectomy. Ann Thorac Surg. 2018;106(2):447-53. doi:10.1016/j.athoracsur.2018.03.039.
453. Finocchiaro G, Haddad F, Kobayashi Y, et al. Impact of Septal Reduction on Left Atrial Size and Diastole in Hypertrophic Cardiomyopathy. Echocardiography. 2016;33(5):686-94. doi:10.1111/ECHO.13158.
454. Blackshear JL, Stark ME, Agnew RC, et al. Remission of recurrent gastrointestinal bleeding after septal reduction therapy in patients with hypertrophic obstructive cardiomyopathyassociated acquired von Willebrand syndrome. J Thromb Haemost. 2015;13(2):191-6. doi:10.1111/JTH.12780.
455. Desai MY, Smedira NG, Dhillon A, et al. Prediction of sudden death risk in obstructive hypertrophic cardiomyopathy: Potential for refinement of current criteria. J Thorac Cardiovasc Surg. 2018;156(2):750-759.e3. doi:10.1016/J.JTCVS.2018.03.150.
456. McLeod CJ, Ommen SR, Ackerman MJ, et al. Surgical septal myectomy decreases the risk for appropriate implantable cardioverter defibrillator discharge in obstructive hypertrophic cardiomyopathy. Eur Heart J. 2007;28(21):2583-8. doi:10.1093/EURHEARTJ/EHM117.
457. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;70(2):252-89. doi:10.1016/J.JACC.2017.03.011.
458. Sorajja P, Nishimura RA, Gersh BJ, et al. Outcome of mildly symptomatic or asymptomatic obstructive hypertrophic cardiomyopathy: a long-term follow-up study. J Am Coll Cardiol. 2009;54(3):234-41. doi:10.1016/J.JACC.2009.01.079.
459. Ball W, Ivanov J, Rakowski H, et al. Long-term survival in patients with resting obstructive hypertrophic cardiomyopathy comparison of conservative versus invasive treatment. J Am Coll Cardiol. 2011;58(22):2313-21. doi:10.1016/J.JACC.2011.08.040.
460. Mestres CA, Bartel T, Sorgente A, et al. Hypertrophic Obstructive Cardiomyopathy: What, When, Why, for Whom? Eur J Cardiothorac Surg. 2018;53(4):700-7.
461. Хитрова М. Э., Бокерия Л. А., Берсенева М. И. и др. Метаанализ результатов хирургического лечения гипертрофической обструктивной кардиомиопатии. Креативная кардиология. 2017;11(4):337-47. doi:10.24022/19973187-2017-11-4-337-347.
462. Veselka J, Jensen MK, Liebregts M, et al. Long-term clinical outcome after alcohol septal ablation for obstructive hypertrophic cardiomyopathy: Results from the Euro-ASA registry. Eur Heart J. 2016;37(19):1517-23. doi:10.1093/eurheartj/ehv693.
463. Bogachev-Prokophiev A, Afanasyev A, Zheleznev S, et al. Mitral Valve Repair or Replacement in Hypertrophic Obstructive Cardiomyopathy: A Prospective Randomized Study. Interact Cardiovasc Thorac Surg. 2017;25(3):356-62. doi:10.1093/ICVTS/IVX152.
464. Bogachev-Prokophiev A, Afanasyev AV, Zheleznev S, et al. Septal Myectomy With Vs Without Subvalvular Apparatus Intervention in Patients With Hypertrophic Obstructive Cardiomyopathy: A Prospective Randomized Study. Semin Thorac Cardiovasc Surg. 2019;31(3):424-31. doi:10.1053/j.semtcvs.2019.01.011.
465. Afanasyev A, Bogachev-Prokophiev A, Lenko E, et al. Myectomy With Mitral Valve Repair Versus Replacement in Adult Patients With Hypertrophic Obstructive Cardiomyopathy: A Systematic Review and Meta-Analysis. Interact Cardiovasc Thorac Surg. 2019;28(3):46572. doi:10.1093/ICVTS/IVY269.
466. Гурщенков А. В., Сухова И. В., Зайцев В. В. и др. Пятилетний опыт использования мобилизации сердца при септальной миоэктомии. Кардиология и сердечно-сосудистая хирургия. 2018;11(4):54-8.
467. Morrow AG, Reitz BA, Epstein SE, et al. Operative treatment in hypertrophic subaortic stenosis. Techniques, and the results of pre and postoperative assessments in 83 patients. Circulation. 1975;52(1):88-102. doi:10.1161/01.CIR.52.1.88.
468. Messmer BJ, Klues HG, Reith S, et al. Hypertrophic obstructive cardiomyopathy. Adv Card Surg. 1998;10:245-70.
469. Хитрова М. Э., Бокерия Л. А., Берсенева М. И., Маленков Д. А. Клинические случаи успешного хирургического лечения гипертрофической обструктивной кардиомиопатии с митральной недостаточностью и samсиндромом, выполненного методом миэктомии межжелудочковой перегородки из правого желудочка. Бюллетень НЦССХ им. А. Н. Бакулева РАМН. 2017;18(6):609-17.
470. Sun D, Schaff HV, Nishimura RA, et al. Transapical Septal Myectomy for Hypertrophic Cardiomyopathy With Midventricular Obstruction. Ann Thorac Surg. 2021;111(3):836-44. doi:10.1016/J.ATHORACSUR.2020.05.182.
471. Tang Y, Song Y, Duan F, et al. Extended myectomy for hypertrophic obstructive cardiomyopathy patients with midventricular obstruction. Eur J Cardiothorac Surg. 2018;54(5):875-83. doi:10.1093/EJCTS/EZY203.
472. Borisov KV. Right ventricle myectomy. Ann Cardiothorac Surg. 2017;6(4):402-9. doi:10.21037/acs.2017.07.10.
473. Wehman B, Ghoreishi M, Foster N, et al. Transmitral Septal Myectomy for Hypertrophic Obstructive Cardiomyopathy. Ann Thorac Surg. 2018;105(4):1102-8. doi:10.1016/j.athoracsur.2017.10.045.
474. Бокерия Л. А. Гипертрофическая обструктивная кардиомиопатия. Анналы хирургии. 2013;5:5-14.
475. Takahashi J, Wakamatsu Y, Okude J, et al. Septal Myectomy, Papillary Muscle Resection, and Mitral Valve Replacement for Hypertrophic Obstructive Cardiomyopathy: A Case Report. Ann Thorac Cardiovasc Surg. 2008;14(4):258-62.
476. Holst KA, Hanson KT, Ommen SR, et al. Septal Myectomy in Hypertrophic Cardiomyopathy: National Outcomes of Concomitant Mitral Surgery. Mayo Clin Proc. 2019;94(1): 66-73. doi:10.1016/J.MAYOCP.2018.07.022.
477. Hong JH, Schaff HV, Nishimura RA, et al. Mitral Regurgitation in Patients With Hypertrophic Obstructive Cardiomyopathy: Implications for Concomitant Valve Procedures. J Am Coll Cardiol. 2016;68(14):1497-504. doi:10.1016/J.JACC.2016.07.735.
478. Stassano P, Tommaso LDi, Triggiani D, et al. Mitral Valve Replacement and Limited Myectomy for Hypertrophic Obstructive Cardiomyopathy: A 25-Year Follow-Up. Texas Hear Inst J. 2004;31(2):137-42.
479. Afanasyev AV, Bogachev-Prokophiev AV, Zheleznev SI, et al. Edge-to-Edge Repair Versus Secondary Cord Cutting During Septal Myectomy in Patients With Hypertrophic Obstructive Cardiomyopathy: A Pilot Randomised Study. Heart Lung Circ. 2021;30(3):43845. doi:10.1016/J.HLC.2020.05.106.
480. Ferrazzi P, Spirito P, Iacovoni A, et al. Transaortic Chordal Cutting: Mitral Valve Repair for Obstructive Hypertrophic Cardiomyopathy With Mild Septal Hypertrophy. J Am Coll Cardiol. 2015;66(15):1687-96. doi:10.1016/J.JACC.2015.07.069.
481. Nguyen A, Schaff HV, Nishimura RA, et al. Apical myectomy for patients with hypertrophic cardiomyopathy and advanced heart failure. J Thorac Cardiovasc Surg. 2020;159(1):14552. doi:10.1016/J.JTCVS.2019.03.088.
482. Afanasyev A, Bogachev-Prokophiev A, Zheleznev S, et al. Transapical Approach to Septal Myectomy for Hypertrophic Cardiomyopathy. Life (Basel, Switzerland). 2024;14(1):125. doi:10.3390/LIFE14010125.
483. Афанасьев А. В., Богачев-Прокофьев А. В., Кирилова В. С. и др. Трансапикальная миоэктомия как альтернатива трансплантации сердца у пациента с апикальной гипертрофической кардиомиопатией. Клиническая и экспериментальная хирургия, журнал им. акад. Б. В. Петровского. 2024;12(1):127-34.
484. Boll G, Rowin EJ, Maron BJ, et al. Efficacy of Combined Cox-Maze IV and Ventricular Septal Myectomy for Treatment of Atrial Fibrillation in Patients With Obstructive Hypertrophic Cardiomyopathy. Am J Cardiol. 2020;125(1):120-6. doi:10.1016/J.AMJCARD.2019.09.029.
485. Bogachev-Prokophiev AV, Afanasyev AV, Zheleznev SI, et al. Concomitant ablation for atrial fibrillation during septal myectomy in patients with hypertrophic obstructive cardiomyopathy. J Thorac Cardiovasc Surg. 2018;155(4):1536-42.e2. doi:10.1016/ j.jtcvs.2017.08.063.
486. Prinz C, Schwarz M, Ilic I, et al. Myocardial Fibrosis Severity on Cardiac Magnetic Resonance Imaging Predicts Sustained Arrhythmic Events in Hypertrophic Cardiomyopathy. Can J Cardiol. 2013;29(3):358-63. doi:10.1016/j.cjca.2012.05.004.
487. Sherrid MV, Massera D. Risk Stratification and Hypertrophic Cardiomyopathy Subtypes. J Am Coll Cardiol. 2019;74(19):2346-9. doi:10.1016/j.jacc.2019.09.020.
488. O’Hanlon R, Grasso A, Roughton M, et al. Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2010;56(11):867-74. doi:10.1016/ j.jacc.2010.05.010.
489. Topilsky Y, Pereira NL, Shah DK, et al. Left ventricular assist device therapy in patients with restrictive and hypertrophic cardiomyopathy. Circ Hear Fail. 2011;4(3):266-75. doi:10.1161/CIRCHEARTFAILURE.110.959288.
490. Sreenivasan J, Kaul R, Khan MS, et al. Left Ventricular Assist Device Implantation in Hypertrophic and Restrictive Cardiomyopathy: A Systematic Review. ASAIO J. 2021;67(3):239-44. doi:10.1097/MAT.0000000000001238.
491. Patel SR, Saeed O, Naftel D, et al. Outcomes of Restrictive and Hypertrophic Cardiomyopathies After LVAD: An INTERMACS Analysis. J Card Fail. 2017;23(12):859-67. doi:10.1016/J.CARDFAIL.2017.09.011.
492. Yagi N, Seguchi O, Mochizuki H, et al. Implantation of ventricular assist devices in hypertrophic cardiomyopathy with left ventricular systolic dysfunction. ESC Hear Fail. 2021;8(6):5513-22. doi:10.1002/EHF2.13653.
493. Grupper A, Park SJ, Pereira NL, et al. Role of ventricular assist therapy for patients with heart failure and restrictive physiology: Improving outcomes for a lethal disease. J Heart Lung Transplant. 2015;34(8):1042-9. doi:10.1016/J.HEALUN.2015.03.012.
494. Coutu M, Perrault LP, White M, et al. Cardiac transplantation for hypertrophic cardiomyopathy: a valid therapeutic option. J Heart Lung Transplant. 2004;23(4):413-7. doi:10.1016/S1053-2498(03)00225-0.
495. Диагностикаилечение сердечно-сосудистых заболеваний при беременности 2018. Национальные рекомендации. Российский кардиологический журнал. 2018;(3):91-134. doi:10.15829/1560-4071-2018-3-91-134.
496. Bowyer L. The Confidential Enquiry into Maternal and Child Health (CEMACH). Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer 2003-2005. The Seventh Report of the Confidential Enquiries into Maternal Deaths in the UK. Obstet Med. 2008;1(1):54. doi:10.1258/om.2008.080017.
497. Billebeau G, Etienne M, Cheikh-Khelifa R, et al. Pregnancy in women with a cardiomyopathy: Outcomes and predictors from a retrospective cohort. Arch Cardiovasc Dis. 2018;111(3):199-209. doi:10.1016/j.acvd.2017.05.010.
498. Krul SP, van der Smagt JJ, van den Berg MP, et al. Systematic Review of Pregnancy in Women With Inherited Cardiomyopathies. Eur J Hear Fail. 2011;13:584-94.
499. Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165-241. doi:10.1093/eurheartj/ehy340.
500. Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011;32(24):3147-97. doi:10.1093/EURHEARTJ/ EHR218.
501. Schaufelberger M. Cardiomyopathy and pregnancy. Heart. 2019;105(20):1543-51. doi:10.1136/heartjnl-2018-313476.
502. Goland S, Hagen IM van, Elbaz-Greener G, et al. Pregnancy in women with hypertrophic cardiomyopathy: data from the European Society of Cardiology initiated Registry of Pregnancy and Cardiac disease (ROPAC). Eur Hear J. 2017;38(35):2683-90.
503. Pieper PG, Walker F. Pregnancy in women with hypertrophic cardiomyopathy. Neth Heart J. 2013;21(1):14-8. doi:10.1007/S12471-012-0358-7.
504. Lee MS, Chen W, Zhang Z, et al. Atrial Fibrillation and Atrial Flutter in Pregnant Women-A Population-Based Study. J Am Heart Assoc. 2016;5(4): e003182. doi:10.1161/JAHA.115.003182.
505. Tromp CHN, Nanne ACM, Pernet PJM, et al. Electrical cardioversion during pregnancy: Safe or not? Netherlands Hear J. 2011;19(3):134-6. doi:10.1007/s12471-011-0077-5.
506. Miyoshi T, Kamiya CA, Katsuragi S, et al. Safety and efficacy of implantable cardioverterdefibrillator during pregnancy and after delivery. Circ J. 2013;77(5):1166-70. doi:10.1253/CIRCJ.CJ-12-1275.
507. Elliott P, Spirito P. Prevention of hypertrophic cardiomyopathy-related deaths: Theory and practice. Heart. 2008;94(10):1269-75. doi:10.1136/hrt.2008.154385.
508. Elliott PM, Gimeno JR, Thaman R, et al. Historical trends in reported survival rates in patients with hypertrophic cardiomyopathy. Heart. 2006;92(6):785-91. doi:10.1136/ hrt.2005.068577.
509. Maron BJ, Gardin JM, Flack JM, et al. Prevalence of hypertrophic cardiomyopathy in a general population of young adults: Echocardiographic analysis of 4111 subjects in the CARDIA study. Circulation. 1995;92(4):785-9. doi:10.1161/01.CIR.92.4.785.
510. Robinson K, Frenneaux MP, Stockins B, et al. Atrial fibrillation in hypertrophie cardiomyopathy: A longitudinal study. J Am Coll Cardiol. 1990;15(6):1279-85. doi:10.1016/ S0735-1097(10)80014-2.
511. Monserrat L, Elliott PM, Gimeno JR, et al. Non-sustained ventricular tachycardia in hypertrophic cardiomyopathy: An independent marker of sudden death risk in young patients. J Am Coll Cardiol. 2003;42(5):873-9. doi:10.1016/S0735-1097(03)00827-1.
512. Todiere G, Aquaro GD, Piaggi P, et al. Progression of myocardial fibrosis assessed with cardiac magnetic resonance in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2012;60(10):922-9. doi:10.1016/j.jacc.2012.03.076.
513. Burton H, Alberg C, Stewart A. Heart to Heart: Inherited Cardiovascular Conditions Services — A Needs Assessment and Service Review. 2009. p. 164. ISBN: 978-1-907198-01-4.
514. Maron BJ, Nishimura RA, Maron MS. Shared decision-making in HCM. Nat Rev Cardiol. 2017;14(3):125-6. doi:10.1038/NRCARDIO.2017.6.
515. Monda E, Limongelli G. The hospitalizations in hypertrophic cardiomyopathy: "The dark side of the moon". Int J Cardiol. 2020;318:101-2. doi:10.1016/J.IJCARD.2020.08.054.
516. Matsubara K, Nakamura T, Kuribayashi T, et al. Sustained cavity obliteration and apical aneurysm formation in apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2003;42(2):288-95. doi:10.1016/S0735-1097(03)00576-X.
517. Eriksson MJ, Sonnenberg B, Woo A, et al. Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;39(4):638-45. doi:10.1016/S07351097(01)01778-8.
518. Chen CC, Lei MH, Hsu YC, et al. Apical hypertrophic cardiomyopathy: correlations between echocardiographic parameters, angiographic left ventricular morphology, and clinical outcomes. Clin Cardiol. 2011;34(4):233-8. doi:10.1002/CLC.20874.
519. Hughes RK, Knott KD, Malcolmson J, et al. Apical Hypertrophic Cardiomyopathy: The Variant Less Known. J Am Heart Assoc. 2020;9(5): e015294. doi:10.1161/JAHA.119.015294.
520. Deva DP, Hanneman K, Li Q, et al. Cardiovascular magnetic resonance demonstration of the spectrum of morphological phenotypes and patterns of myocardial scarring in Anderson-Fabry disease. J Cardiovasc Magn Reson. 2016;18(1):14. doi:10.1186/ S12968-016-0233-6.
521. Ünlü S, Özden Tok Ö, Avcı Demir F, et al. Differential diagnosis of apical hypertrophic cardiomyopathy and apical displacement of the papillary muscles: a multimodality imaging point of view. Echocardiography. 2021;38(1):103-13. doi:10.1111/ECHO.14895.
522. Ruberg FL, Berk JL. Transthyretin (TTR) cardiac amyloidosis. Circulation. 2012;126(10):1286-300. doi:10.1161/CIRCULATIONAHA.111.078915.
523. Efthimiadis GK, Pagourelias ED, Gossios T, Zegkos T. Hypertrophic cardiomyopathy in 2013: Current speculations and future perspectives. World J Cardiol. 2014;6(2):26-37. doi:10.4330/wjc.v6.i2.26.
524. Efthimiadis GK, Pagourelias E, Zegkos T, et al. An Overview of Pharmacotherapy in Hypertrophic Cardiomyopathy: Current Speculations and Clinical Perspectives. Rev Cardiovasc Med. 2016;17(3-4):115-23.
Об авторах
Л. А. БокерияРоссия
академик РАН, д.м.н., профессор
Москва
Е. В. Шляхто
академик РАН, д.м.н., профессор
Санкт-Петербург
С. А. Габрусенко
д.м.н., профессор
Москва
А. Я. Гудкова
д.м.н.
Санкт-Петербург
Н. А. Козиолова
д.м.н., профессор
Пермь
С. А. Александрова
к.м.н.
Москва
М. Н. Алехин
д.м.н., профессор
Москва
А. В. Афанасьев
д.м.н.
Новосибирск
М. М-Б. Богатырева
к.м.н., доцент
Магас
А. В. Богачев-Прокофьев
д.м.н.
Новосибирск
Д. В. Богданов
д.м.н., профессор
Челябинск
М. И. Берсенева
к.м.н., доцент
Москва
М. Л. Гордеев
д.м.н., профессор
Санкт-Петербург
С. Л. Дземeшкевич
д.м.н., профессор
Москва
А. В. Евтушенко
д.м.н.
Кемерово
Е. В. Заклязьминская
д.м.н.
Москва
Д. И. Зенченко
к.м.н.
Волгоград
О. Б. Иртюга
д.м.н., доцент
Санкт-Петербург
В. Ю. Каплунова
д.м.н.
Москва
М. Г. Каштанов
к.м.н.
Екатеринбург
А. А. Костарева
д.м.н., профессор
Санкт-Петербург
А. Н. Крутиков
к.м.н.
Санкт-Петербург
Д. А. Маленков
Москва
Т. Н. Новикова
д.м.н., доцент
Санкт-Петербург
С. Д. Рудь
к.м.н., доцент
Санкт-Петербург
М. М. Рыбка
д.м.н., профессор
Москва
М. А. Саидова
д.м.н., профессор
Москва
А. А. Стрельцова
Санкт-Петербург
Конфликт интересов:
St. Petersburg
О. В. Стукалова
к.м.н., доцент
Москва
М. П Чмелевский
Санкт-Петербург
И. И. Шапошник
д.м.н., профессор
Челябинск
Е. А. Шлойдо
к.м.н.
Санкт-Петербург
Рецензия
Для цитирования:
Бокерия Л.А., Шляхто Е.В., Габрусенко С.А., Гудкова А.Я., Козиолова Н.А., Александрова С.А., Алехин М.Н., Афанасьев А.В., Богатырева М.М., Богачев-Прокофьев А.В., Богданов Д.В., Берсенева М.И., Гордеев М.Л., Дземeшкевич С.Л., Евтушенко А.В., Заклязьминская Е.В., Зенченко Д.И., Иртюга О.Б., Каплунова В.Ю., Каштанов М.Г., Костарева А.А., Крутиков А.Н., Маленков Д.А., Новикова Т.Н., Рудь С.Д., Рыбка М.М., Саидова М.А., Стрельцова А.А., Стукалова О.В., Чмелевский М.П., Шапошник И.И., Шлойдо Е.А. Гипертрофическая кардиомиопатия. Клинические рекомендации 2025. Российский кардиологический журнал. 2025;30(5):6387. https://doi.org/10.15829/1560-4071-2025-6387. EDN: BUUCJT
For citation:
Bokeria l.A., Shlyakhto E.V., Gabrusenko S.A., Gudkova A.Ya., Koziolova N.A., Alexandrova S.A., Alekhin M.N., Afanasyev A.V., Bogatyreva M.M., Bogachev-Prokofiev A.V., Bogdanov D.V., Berseneva M.I., Gordeev M.L., Dzemeshkevich S.L., Yevtushenko A.V., Zaklyazminskaya E.V., Zenchenko D.I., Irtyuga O.B., Kaplunova V.Yu., Kashtanov M.G., Kostareva A.A., Krutikov A.N., Malenkov D.A., Novikova T.N., Rud S.D., Rybka M.M., Saidova M.A., Streltsova A.A., Stukalova O.V., Chmelevsky M.P., Shaposhnik I.I., Shloido E.A. 2025 Clinical practice guidelines for Hypertrophic cardiomyopathy. Russian Journal of Cardiology. 2025;30(5):6387. (In Russ.) https://doi.org/10.15829/1560-4071-2025-6387. EDN: BUUCJT
JATS XML