DISSYNCHRONY. RESYNCHRONIZATION. STIMULATION. CHRONIC HEART FAILURE
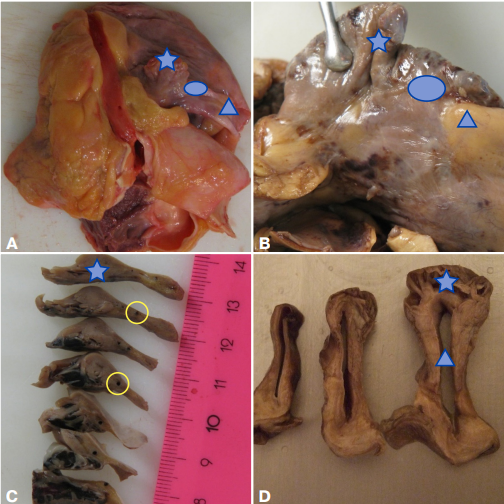
The review provides a current view of the anatomy, histology, immunohistochemistry, electron microscopy, and electron immunocytochemistry of the cardiac conduction system (CCS) based on literature data and the author's own research over more than 30 years. The article describes a new specialized x-structure of the CCS, discovered by the author and published in 2014, and another type of cells that are part of the sinus and atrioventricular nodes — telocytes, capable of generating and conducting an electrical impulse. Based on layer-by-layer dissection and serial histological sections performed on more than 400 adult hearts, the topographic anatomy of the atrial muscular framework is given. The article also describes the atrial innervation.
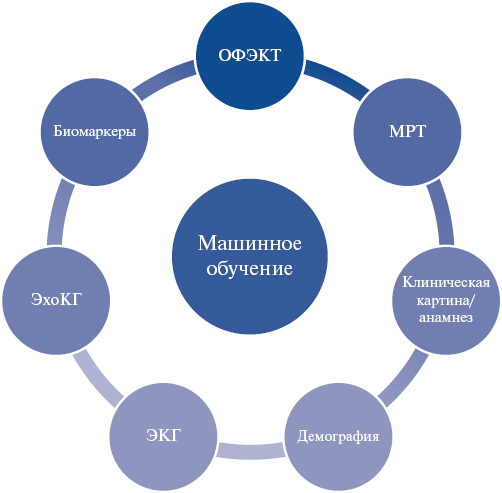
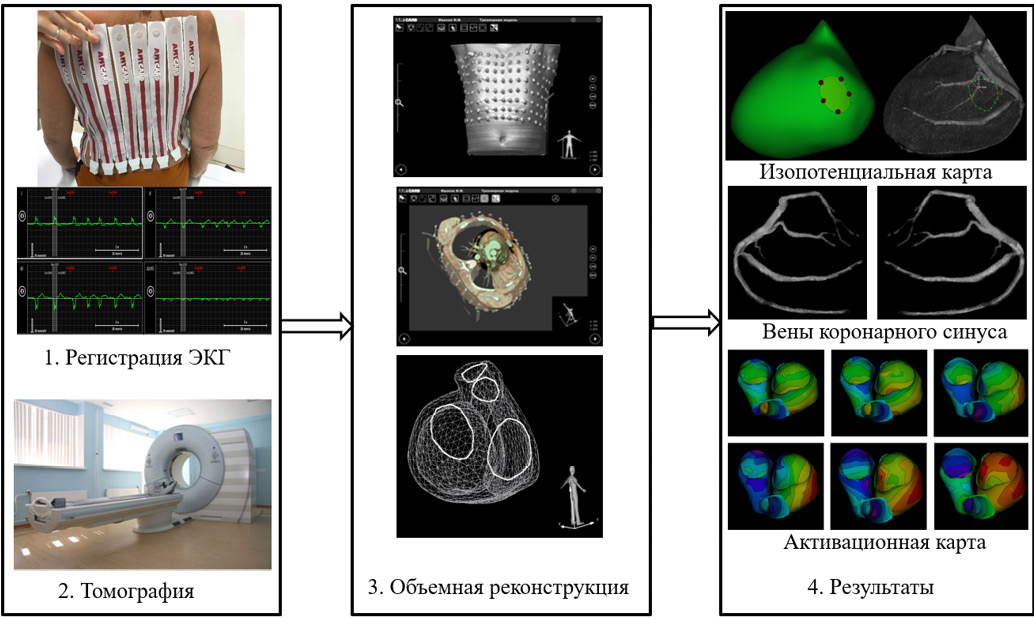
- This article reviews articles that use modern methods of artificial intelligence and multiscale modeling in cardiac dyssynchrony and cardiac resynchronization therapy (CRT).
- For the first time, promising approaches combining mechanistic and artificial intelligence models are analyzed.
- The article describes the features of using clinical data of various modalities, as well as the results of personalized modeling for phenotyping patient groups, predicting and optimization of CRT using machine learning methods.
- The authors’ own works are considered, in which, for the first time, an algorithm for selecting candidates for CRT and optimizing the position of the left ventricular lead in biventricular pacing was developed and validated based on a prognostic model built on combined clinical and model data.
The review is devoted to the current status of artificial intelligence (AI), mathematical modeling (MM) and their combination in the analysis of cardiac dyssynchrony mechanisms and its treatment using cardiac resynchronization therapy (CRT). Recent articles and reviews demonstrate the high promise of AI and MM in personalized medicine, but also identify existing obstacles to their implementation in clinical practice. The works discussed are devoted to a number of topical problems of clinical cardiology as follows: analysis of phenotypes of patients with cardiac dyssynchrony, search for novel prognostic factors of CRT effectiveness, pacing optimization, creation of highly accurate predictive models of response to CRT. For the first time, a review of studies is given that use combined approaches of mechanistic MM and AI. Such approaches break new ground for the application of personalized heart models both for generating realistic synthetic data (digital twins) on which AI models are trained, and as predictors that, along with clinical signs, are used in trained prognostic AI models to improve the accuracy of personalized diagnostics, predict the effectiveness and optimize treatment. The review consists of three sections focused on studies using AI, personalized MM of heart ventricles, and combined approaches (MM+AI).
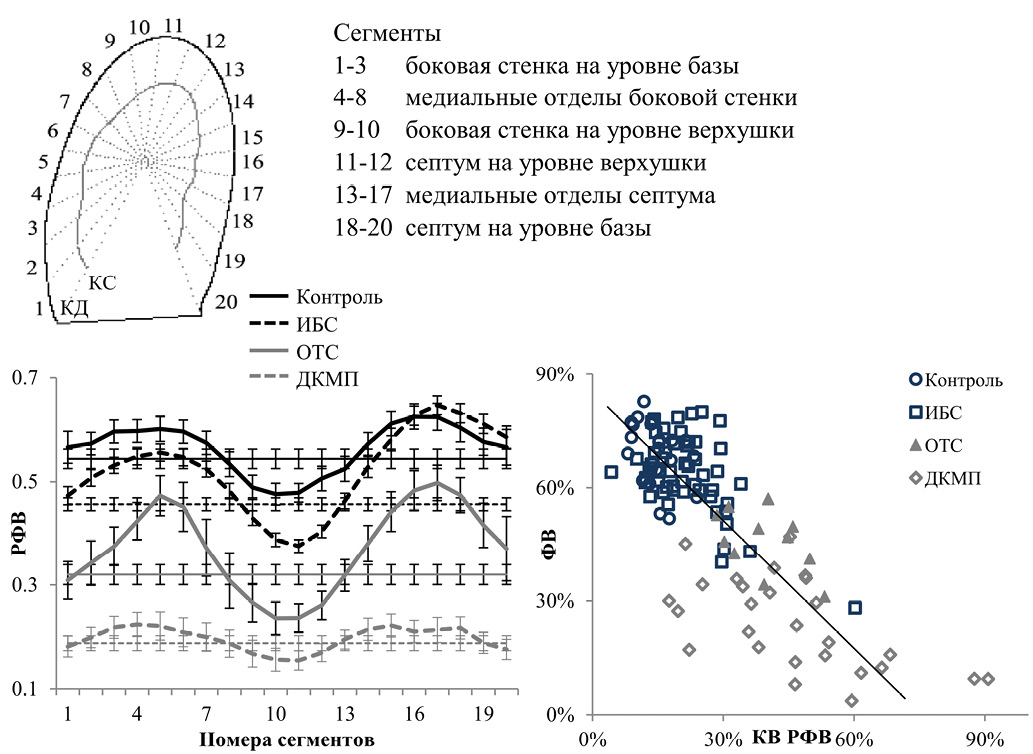
- The first review of shape analysis methods as applied to cardiology is conducted.
- The studies of left ventricular shape, regional features of the left ventricular wall motion, and the diagnostic significance of shape features are considered.
- Using examples from our own studies, the features of left ventricular wall motion heterogeneity with and without pathology are demonstrated, and an approach of left ventricular functional geometry for assessing and diagnosing ventricular contraction pathology is described.
- A description of geometric morphometrics on echocardiographic data is given.
The review discusses the importance of left ventricular shape analysis for diagnosis, severity assessment and prediction of treatment effectiveness in cardiac dyssynchrony. Various methods for assessing the left ventricle shape are consistently considered, starting from the sphericity index common in clinical practice, moving on to more complex and/or rare indices, then to the author's indices of left ventricular functional geometry, as well as to the methods of geometric morphometrics. The results obtained using left ventricular shape analysis in diagnostics and treatment planning are presented.
- There are various methods for imaging electrical and mechanical cardiac dyssynchrony.
- Potential of qualitative and quantitative assessment of dyssynchrony before and after cardiac resynchronization therapy are demonstrated.
- A comprehensive assessment is required, since there is no single universal method for diagnosing dyssynchrony.
The article presents an analysis of our own experience in the light of world literature on a wide range of methods for assessing electrical and mechanical cardiac dyssynchrony. Over the past decades, various options have been proposed, ranging from simple and easily performed ones, such as 12-lead electrocardiography, to more complex and expensive methods, such as invasive electroanatomical mapping. Despite promising results, none of the methods has yet become universal, capable of answering all questions. In this regard, the multifaceted process of assessing dyssynchrony continues.
- Diagnosis of left bundle branch block (LBBB) remains a complex clinical problem due to the variety of ventricular activation patterns, as well as different conduction block location with a similar electrocardiographic pattern.
- A comparative analysis of Russian and international criteria for LBBB diagnosis and their prognostic value for cardiac resynchronization therapy (CRT) is presented.
- The advantages and limitations of current electrocardiographic criteria for predicting response to CRT are identified.
- Novel diagnostic approaches and criteria for proximal LBBB, identified based on a study of patients with surgically induced proximal left bundle branch block, are described.
The paper presents an analysis of Russian and foreign studies on left bundle branch block (LBBB) and the analysis of electrocardiographic (ECG) criteria for selecting patients for cardiac resynchronization therapy. The features of LBBB classification are considered, including true and false forms, as well as differences in conduction block location with a similar ECG performance. Particular attention is paid to the problem of variability of existing ECG criteria and the prognostic significance of individual ECG signs. The importance of developing new criteria for improving diagnostics and increasing the effectiveness of treatment of LBBB patients is emphasized to improve selection for biventricular and conduction system pacing.
- Pacemaker-induced cardiomyopathy (PICM) is a complication of frequent right ventricular pacing.
- Cases of PICM with preserved left ventricular ejection fraction are insufficiently described.
- An analysis of the studies on the role of constant right ventricular pacing and its contribution to PICM development is carried out.
Pacemaker-induced cardiomyopathy (PICM) is a complication of frequent right ventricular pacing, which in most studies is regarded as a decrease in the left ventricular ejection fraction with constant right ventricular pacing. However, cases of PICM with preserved left ventricular ejection fraction are insufficiently described, since the onset most often occurs as a phenotype of heart failure with preserved ejection fraction. The paper analyzes the studies on the role of constant right ventricular pacing and its contribution to PICM development.
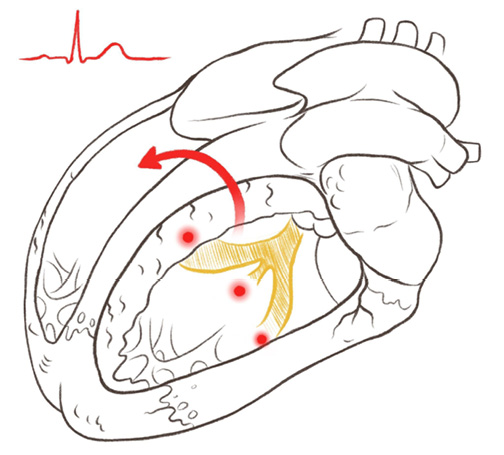
- Cardioneuroablation is an alternative treatment for vasovagal syncope and functional neurogenic bradyarrhythmias (atrioventricular conduction disorders or sinus node dysfunction).
- Before pacemaker implantation, additional examination of the patient is required to exclude the neurogenic bradyarrhythmia and consider cardiac neuroablation, which allows avoiding pacemaker implantation or delaying it.
Interest in the autonomic regulation of the cardiovascular system does not wane. Changes in autonomic nervous system activity are involved in the pathogenesis of acute and chronic conditions, such as sinus bradycardia, sinus arrest and atrioventricular block, vasovagal syncope and other types of syncopal conditions. Traditional methods of prevention and treatment of such conditions include lifestyle changes, pharmacotherapy and, in some cases, pacemaker implantation, but in many cases they are unable to eliminate the symptoms or cure the disease. We conducted a descriptive review of the most significant publications on effectiveness and development of the cardiac neuroablation technique in patients with vasovagal syncope and neurogenic functional bradyarrhythmias — sinus node dysfunction and atrioventricular conduction disorders. This technique allows to effectively prevent neurocardiogenic syncope relapses, reduce the tendency to functional bradyarrhythmias by eliminating pathological parasympathetic tone. Cardioneuroablation allows to eliminate indications for pacemaker implantation or to delay its implementation.
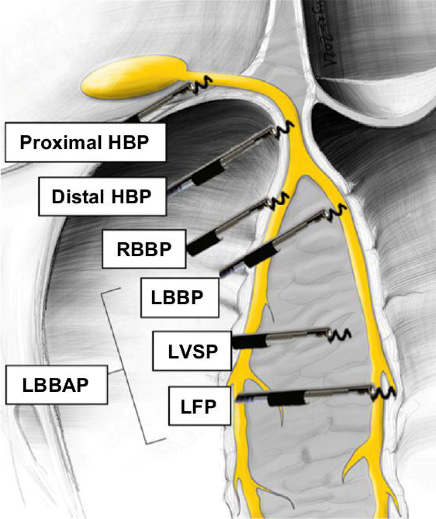
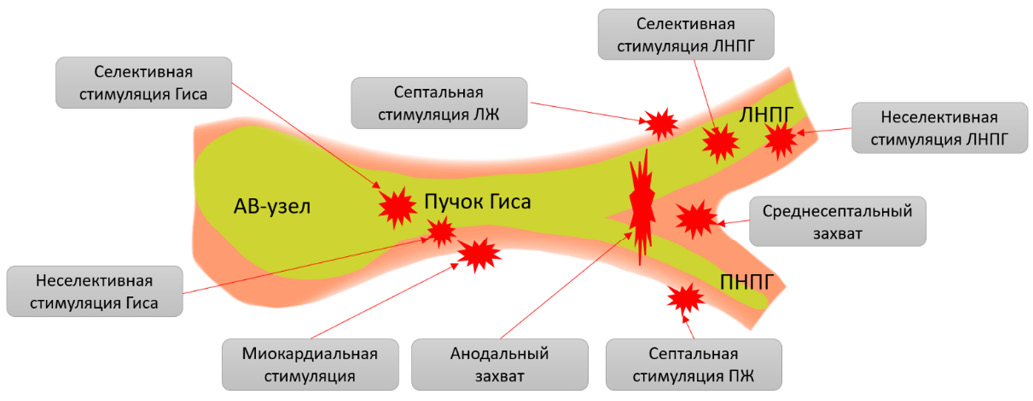
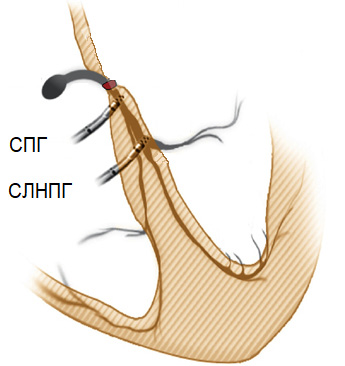
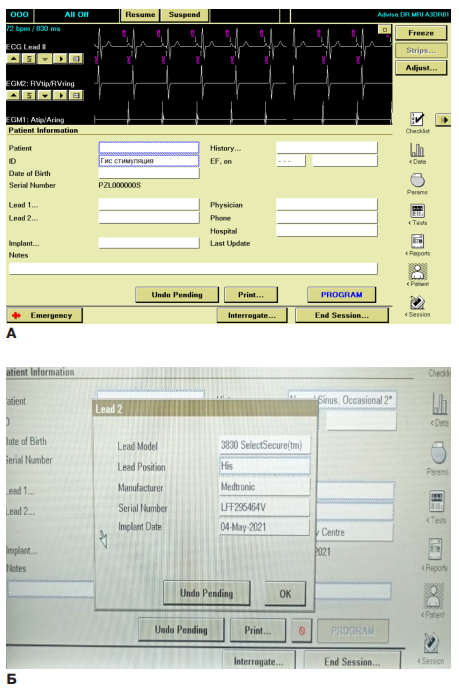
- His bundle pacing is the most physiological type of cardiac pacing.
- Conduction system pacing can correct conduction disorders in the His bundle branches.
- Conduction system stimulation can be an alternative to traditional biventricular pacing in cardiac resynchronization therapy.
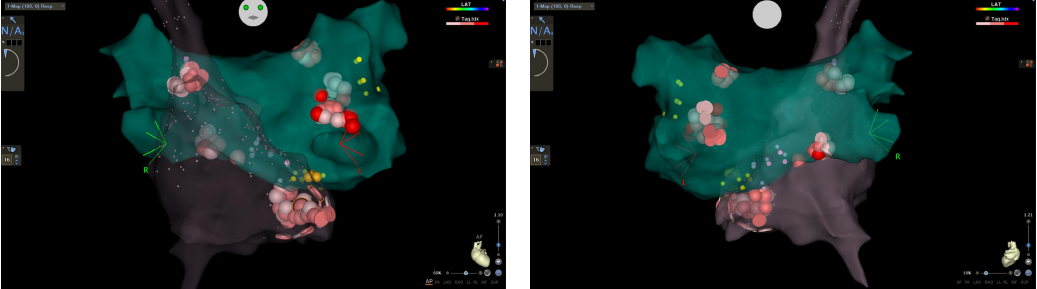
His bundle pacing is a direct pacing of the specialized His-Purkinje conduction system with the aim of physiological ventricular activation, in contrast to the dyssynchronous activation by conventional myocardial pacing.
In this review article on His-Purkinje conduction system pacing, the authors evaluate the available data and current practice, and assess emerging and future directions in this fast growing area. We analyzed the available publications on His bundle and conduction system pacing.
Since the first report of permanent His-bundle pacing (HBP) in 2000, the earliest incarnation of stylet-driven technique has been replaced by the more effective non-stylet-driven approach. Widespread adoption has generated a large evidence base. Single-center observational studies have been complemented by large multicenter international registries, mechanistic studies, and the first randomized controlled trials. New data have clarified the mechanisms of РИЗ and illustrated the nature and extent of its potential benefits in preventing pacing cardiomyopathy and correcting bundle branch block.
Conduction system stimulation is the most physiological type of cardiac pacing in patients with a narrow QRS complex. Conduction system pacing may be an effective alternative to biventricular pacing in cardiac resynchronization therapy. Randomized controlled trials are needed to expand the evidence base.
- The technique of left bundle branch pacing is safe, effective and reproducible. At the same time, it allows ventricular physiological depolarization.
- In the context of cardiac resynchronization therapy, left bundle branch pacing shows promise and may be used in a large number of patients as an alternative to conventional biventricular pacing.
Left bundle branch pacing is a new type of physiological cardiac pacing. It has advantages in patients with bradycardia and heart failure. However, this type of treatment raises a number of questions among specialists. There is a misunderstanding of implantation technical aspects, and evidence base for this method remains unclear due to the small number of large-scale studies in the world literature, as well as the absence of this type of treatment in Russian clinical guidelines. In this article, a group of authors reflects the solution of the above problems in clinical practice by describing the technical aspects of left bundle branch pacing and showing its advantages as an alternative to resynchronization therapy and conventional electrical pacing.
- The article analyzes the development and advancement of the approach to physiological pacing, highlighting the programming of modern pacing systems in different practical situations.
Conduction system pacing is widely used as an alternative to right ventricular pacing and, in some cases, as an alternative to biventricular pacing for cardiac resynchronization therapy. Proper programming of an implantable electronic device is essential to ensure patient safety and maximize the benefits. The aim of this article is to provide information on the practical aspects of programming His bundle and left bundle branch pacing and subsequent monitoring.
ISSN 2618-7620 (Online)